Medical practice management software (PMS) is a specialized digital solution designed to streamline the administrative, financial, and operational workflows of healthcare practices. Unlike purely clinical systems, PMS focuses on the business side of running a medical facility—handling tasks such as appointment scheduling, billing, insurance claims, patient communications, and performance reporting. Whether implemented in a small private clinic or a multi-specialty hospital, the core aim of PMS is to reduce manual workload, improve accuracy, and allow healthcare professionals to focus more on patient care instead of administrative burdens.
Medical practice management software is not just a single application but a suite of interconnected tools that support day-to-day operations. A well-designed PMS covers scheduling, patient data management, claims processing, payment collection, compliance tracking, and even inventory oversight for medical supplies. Some systems extend into patient engagement features such as automated reminders, online bill payment, and secure messaging portals. The scope of PMS has expanded significantly in recent years, now often integrating with telehealth platforms, lab systems, and data analytics tools to give healthcare administrators a complete operational overview.
Difference Between Practice Management Software, EHR, and EMR
While the terms are sometimes used interchangeably, practice management software, electronic health records (EHR), and electronic medical records (EMR) serve distinct purposes.
- Practice Management Software (PMS): Handles operational and financial management—appointments, billing, claims, reporting, and resource allocation.
- Electronic Health Record (EHR): A comprehensive digital record of a patient’s health history, designed for interoperability across providers and facilities.
- Electronic Medical Record (EMR): A digital version of a patient’s chart within a single practice, focusing on clinical data such as diagnoses, prescriptions, and lab results.
The difference lies in focus: PMS manages the business side, EHRs and EMRs manage the clinical side. Modern systems often integrate PMS with EHR/EMR platforms to create a unified ecosystem where clinical and administrative data flow seamlessly.
Why Every Modern Clinic and Hospital Needs It
Healthcare providers today face increasing patient volumes, rising administrative complexity, and stricter compliance demands. Without automation, staff can spend hours on repetitive tasks like scheduling, claims follow-ups, and payment reconciliation—time that could be spent on patient care. PMS reduces these inefficiencies by providing a central dashboard for all operational activities, enabling faster decision-making and improving service delivery.
For clinics, PMS can reduce appointment no-shows through automated reminders, accelerate revenue cycles by minimizing insurance claim denials, and maintain accurate patient data for compliance. For hospitals, especially multi-department facilities, it enables centralized coordination, resource optimization, and data-driven performance monitoring.
In competitive healthcare markets, patient satisfaction also plays a significant role in retention. PMS supports this by offering patient-friendly features such as self-service booking, mobile payment options, and secure communication channels—all of which contribute to a better patient experience.
Quick Stats and Market Growth Insights
The medical practice management software market has been experiencing sustained growth, driven by both regulatory pressures and technological advancements. According to market research reports, The global practice management system market was valued at USD 14.45 billion in 2024 and is expected to grow to USD 25.54 billion by 2030, registering a CAGR of 10.19% between 2025 and 2030. In the United States, adoption is widespread, with most medium-to-large practices already using some form of PMS. The European and UK markets are catching up quickly, with digital transformation initiatives and telehealth adoption accelerating demand.
Cloud-based PMS solutions are seeing the fastest growth, especially among small and mid-sized practices, due to their lower upfront costs, easier scalability, and remote accessibility. Artificial intelligence is also starting to play a role, with AI-powered features such as predictive scheduling, automated coding, and advanced analytics becoming standard in next-generation platforms.
In short, medical practice management software has evolved from a nice-to-have administrative tool into an essential infrastructure component for healthcare organizations seeking efficiency, compliance, and better patient outcomes. As regulatory requirements tighten and patient expectations rise, PMS adoption is no longer optional—it’s a competitive necessity.
AI and Automation Trends in Practice Management
Artificial intelligence is reshaping PMS capabilities, moving the software from reactive task management to proactive decision support. Some notable AI-driven trends include:
- Predictive Scheduling: AI models forecast patient appointment patterns and optimize schedules to reduce no-shows and idle time.
- Automated Medical Coding and Billing: Natural language processing (NLP) tools convert physician notes into accurate billing codes, reducing claim rejections.
- Revenue Cycle Optimization: Machine learning models detect anomalies in claims processing and recommend corrective actions to improve reimbursement rates.
- Patient Communication Automation: AI-powered chatbots and virtual assistants manage appointment reminders, answer FAQs, and handle pre-visit forms.
These advancements not only reduce administrative burdens but also contribute directly to better patient engagement and higher operational efficiency.
The medical practice management software market is mature enough to support robust, feature-rich systems, yet dynamic enough to reward innovation. With global adoption trends pointing toward cloud-native, AI-augmented, and compliance-first platforms, there is significant opportunity for healthcare organizations and software developers to enter the space. The next phase of competition will be won by PMS solutions that combine seamless interoperability, regulatory compliance, and patient-centric design.
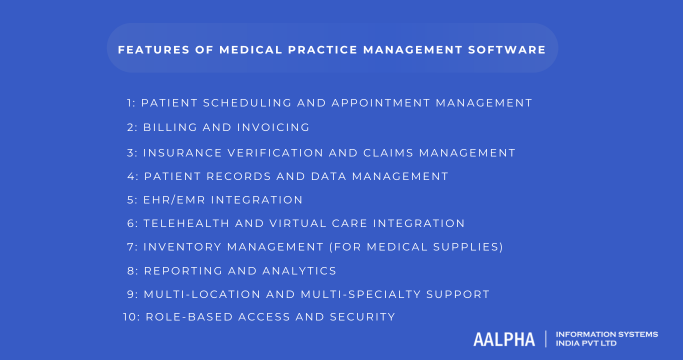
Core Features of Medical Practice Management Software
1. Patient Scheduling and Appointment Management
Efficient scheduling is fundamental to keeping a healthcare practice running smoothly. Delays, double-bookings, or missed appointments can lead to wasted resources and lost revenue. A powerful scheduling module in medical practice management software (PMS) centralizes all appointments in one place, allowing staff to view availability in real time, assign patients to the right providers, and manage multiple appointment types—from quick consultations to complex multi-step treatment plans.
Modern systems extend beyond simple appointment booking by enabling patients to schedule their own visits through self-service portals, reducing phone calls and administrative load. They also incorporate automated reminders sent via SMS, email, or push notifications to reduce no-shows, which directly improves revenue and patient care efficiency. Advanced scheduling features include waitlist management to automatically fill cancelled slots and integration with telehealth platforms to manage both in-person and virtual visits seamlessly.
Key capabilities include:
- Online Self-Booking: Patients can choose their preferred time slot without contacting the clinic.
- Automated Reminders: Notifications sent before appointments to reduce no-show rates.
- Waitlist Management: Filling cancelled slots automatically to maximize provider utilization.
- Multi-Provider Coordination: Linking related appointments across different specialists.
2. Billing and Invoicing
Billing is one of the most error-prone and time-consuming administrative tasks in healthcare. A well-designed PMS automates the entire medical billing cycle, from generating invoices to accepting payments, ensuring accuracy and transparency. By pulling service and treatment details directly from appointment records, the system minimizes missed charges and incorrect codes.
Patients increasingly expect clear, itemized bills and multiple payment options. Integrated payment gateways allow instant settlement via credit/debit cards, bank transfers, or digital wallets, while recurring billing features support ongoing treatments like physiotherapy or chronic disease management. The billing system should also work hand-in-hand with insurance claims processing to streamline reimbursement.
Key capabilities include:
- Automatic Invoice Generation: Creates bills immediately after a visit, reducing delays.
- Integrated Payment Gateways: Supports multiple online payment methods for patient convenience.
- Recurring Billing Support: Automates periodic payments for long-term treatment plans.
- Transparent, Itemized Statements: Improves patient trust and reduces billing disputes.
3. Insurance Verification and Claims Management
Insurance-related errors are a leading cause of delayed or lost revenue. A PMS with robust insurance management tools verifies patient eligibility before the appointment, ensuring providers are reimbursed without unnecessary denials. The software should automate claims creation, check for errors, and submit them electronically to insurers or clearinghouses.
By integrating with insurance APIs, PMS platforms can check coverage in real time, identify missing documentation, and even preemptively flag claims that may be rejected. Effective denial management tools help staff quickly correct and resubmit rejected claims.
Key capabilities include:
- Real-Time Eligibility Checks: Confirms insurance coverage before a visit.
- Claims Scrubbing: Detects and fixes errors before submission to prevent rejections.
- Electronic Data Interchange (EDI): Enables faster, more accurate claim submissions.
- Denial Tracking and Resubmission: Speeds up recovery of lost revenue.
4. Patient Records and Data Management
While clinical records are typically stored in EHR/EMR systems, PMS platforms handle the administrative side of patient data—demographics, contact details, insurance information, and visit history. Having this information centralized reduces duplication and ensures accuracy across all workflows.
An effective PMS links administrative and clinical records for a unified view of each patient. This improves communication between departments, supports compliance, and helps provide personalized patient care.
Key capabilities include:
- Centralized Demographic Records: Stores patient contact and personal information in one place.
- Linked Clinical Data: Integrates with EHR/EMR for complete patient profiles.
- Visit and Payment History: Provides full operational insight for each patient.
- Data Accuracy Controls: Ensures consistency across systems to reduce errors.
5. EHR/EMR Integration
Interoperability is critical for efficient healthcare delivery. PMS systems should seamlessly integrate with existing EHR or EMR platforms to ensure clinical and administrative teams work from the same set of information.
A unified view of patient records improves efficiency, reduces errors during check-in, and speeds up access to treatment histories. The integration should follow industry standards like HL7 and FHIR to ensure compatibility across different healthcare systems.
Key capabilities include:
- Unified Patient View: Combines operational and clinical data in one place.
- Automated Data Sync: Reduces manual entry and risk of errors.
- Standards Compliance: Supports HL7 and FHIR protocols for interoperability.
- Lab and Imaging Integration: Enables direct access to diagnostic results.
6. Telehealth and Virtual Care Integration
Telehealth has moved from a convenience to a necessity. PMS systems that integrate telehealth features eliminate the need for separate platforms, making it easier to manage both physical and virtual appointments from a single dashboard.
Telehealth-ready PMS platforms offer secure video consultations, automated virtual appointment links, and the ability to record visit notes directly into the patient’s file during the call. This integration improves patient access to care while maintaining privacy and compliance.
Key capabilities include:
- Embedded Video Consultations: No need for separate telehealth tools.
- Automated Link Generation: Sends secure session links after booking.
- Documentation Integration: Allows note-taking during virtual visits.
- HIPAA-Compliant Communication: Ensures patient privacy and data protection.
7. Inventory Management (for Medical Supplies)
Medical inventory mismanagement can disrupt patient care and increase costs. A PMS with inventory management tracks stock levels, expiry dates, and supplier details to ensure essential items are always available.
Automated alerts notify staff when supplies are running low, while purchase history tracking helps optimize ordering. This is especially important for practices that use specialized consumables or maintain in-house pharmacies.
Key capabilities include:
- Stock Level Monitoring: Tracks quantities of supplies in real time.
- Expiry Date Alerts: Prevents the use of outdated or unsafe items.
- Supplier Management: Stores vendor details and past orders for quick reordering.
- Automated Reorder Triggers: Maintains optimal stock without over-purchasing.
8. Reporting and Analytics
Data-driven decision-making is key to operational and financial success. PMS platforms should offer robust reporting tools that help administrators track key metrics, spot inefficiencies, and identify growth opportunities.
Reports should be customizable and cover operational, financial, and patient engagement data. Advanced systems use predictive analytics to forecast appointment demand, optimize provider schedules, and identify high-value patient groups.
Important analytics include:
- Appointment Trends: No-show rates, peak booking times, provider utilization.
- Revenue Reports: Billing efficiency, reimbursement timelines, outstanding balances.
- Patient Demographics: Age, location, visit frequency for targeted outreach.
- Predictive Insights: Demand forecasting and resource allocation recommendations.
9. Multi-Location and Multi-Specialty Support
For healthcare groups with multiple locations or specialties, a PMS must centralize operations while allowing for localized control. It should manage location-specific schedules, providers, and resources while keeping all patient data unified.
Such systems enable administrators to oversee performance across locations, ensure consistency in service delivery, and adapt workflows for specialty-specific needs.
Key capabilities include:
- Centralized Scheduling: Manage all locations from one interface.
- Location-Based Reporting: Monitor productivity and revenue per site.
- Specialty Workflows: Adapt features for different departments.
- Unified Patient Records: Maintain one file per patient across all locations.
10. Role-Based Access and Security
Healthcare data is highly sensitive, making access control a critical PMS feature. Role-based access ensures that each staff member sees only the information relevant to their role.
In addition to permissions, the PMS should maintain audit trails that record who accessed or modified data and when. Multi-factor authentication (MFA) adds another layer of security to prevent unauthorized access.
Key capabilities include:
- Granular Permissions: Define access levels for each role.
- Audit Logs: Track all data access and changes.
- Multi-Factor Authentication: Strengthens login security.
- Regulatory Compliance: Meets HIPAA, GDPR, and other data protection requirements.
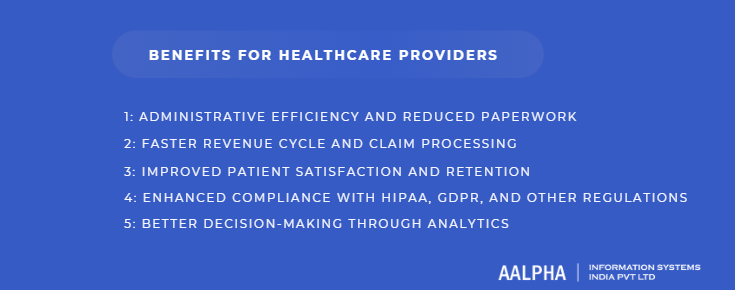
Benefits for Healthcare Providers
Implementing a medical practice management software (PMS) is more than a technology upgrade—it’s a strategic shift in how healthcare providers manage daily operations. From reducing administrative burdens to improving compliance and patient satisfaction, PMS delivers measurable advantages that directly impact both the quality of care and the financial health of a practice.
1. Administrative Efficiency and Reduced Paperwork
One of the most immediate benefits of PMS is the elimination of redundant manual tasks. In a traditional setup, front desk staff spend significant time on phone calls, paper forms, and manual data entry, which can lead to errors and inefficiencies. A PMS automates many of these processes, such as patient registration, appointment scheduling, and billing, allowing administrative staff to focus on higher-value activities.
Digital workflows also mean that forms can be completed online, signatures can be captured electronically, and patient records are instantly retrievable—saving hours of work each week. By replacing paper files with secure, centralized digital records, clinics reduce physical storage needs and the risk of misplaced documents.
Key advantages include:
- Automated Data Entry: Reduces manual input and human errors.
- Digital Forms and Signatures: Streamlines patient onboarding.
- Centralized Document Storage: Easy access to records from any location.
- Less Physical Storage: Eliminates the need for paper archives.
2. Faster Revenue Cycle and Claim Processing
Delays in billing and claim submission can significantly affect a practice’s cash flow. PMS platforms integrate billing with patient visits, ensuring that charges are applied instantly and claims are submitted electronically. Real-time insurance eligibility verification prevents wasted time on services that won’t be reimbursed, while claim scrubbing tools detect missing or incorrect information before submission.
By automating these processes, practices can reduce the average time from service delivery to payment, which in turn improves working capital and financial stability. Faster claims approval also means fewer follow-up calls and less time spent on reprocessing denied claims.
Key advantages include:
- Integrated Billing and Scheduling: Automatically generates bills after appointments.
- Real-Time Insurance Checks: Ensures coverage before treatment.
- Claims Scrubbing: Detects errors before submission to avoid rejections.
- Faster Reimbursements: Reduces the payment cycle from weeks to days.
3. Improved Patient Satisfaction and Retention
Patient experience is increasingly a competitive differentiator in healthcare. A PMS contributes to higher satisfaction by making interactions with the practice smoother and more convenient. Features such as online appointment booking, automated reminders, digital payment options, and secure patient communication channels reduce friction at every touchpoint.
Additionally, having accurate and complete patient records readily available means providers can offer more personalized care. When patients feel their time is respected and their concerns are addressed promptly, they are more likely to return for future care and recommend the practice to others.
Key advantages include:
- Self-Service Appointment Booking: Empowers patients to schedule visits at their convenience.
- Automated Reminders: Reduces missed appointments and last-minute cancellations.
- Digital Payments: Provides multiple payment options for patient ease.
- Personalized Care: Access to accurate patient histories enhances consultations.
4. Enhanced Compliance with HIPAA, GDPR, and Other Regulations
Healthcare regulations are strict for good reason—they protect patient privacy and data security. However, meeting compliance requirements manually can be resource-intensive and error-prone. PMS platforms are designed with compliance in mind, offering built-in safeguards such as data encryption, role-based access, and automatic audit logging.
These features not only help providers stay compliant with frameworks like HIPAA in the United States and GDPR in the European Union but also reduce the risk of costly penalties and reputational damage from data breaches. For multi-location or cross-border practices, having compliance features centralized within the PMS ensures consistent application of data protection policies.
Key advantages include:
- Role-Based Access Control: Limits data access to authorized users.
- Audit Trails: Tracks every change made to patient records.
- Data Encryption: Secures information both in transit and at rest.
- Regulatory Framework Support: Meets HIPAA, GDPR, and ISO 27001 standards.
5. Better Decision-Making Through Analytics
Data is one of the most valuable assets a healthcare practice has, but it’s only useful when analyzed effectively. PMS platforms come with reporting and analytics modules that help administrators and clinicians make informed decisions about operations, staffing, and patient care strategies.
Analytics can reveal patterns in appointment utilization, revenue trends, and patient demographics. This insight helps in resource allocation, identifying underperforming service areas, and even shaping marketing campaigns. More advanced systems leverage predictive analytics to forecast demand, optimize schedules, and anticipate supply needs, allowing providers to proactively address challenges before they impact service quality.
Key advantages include:
- Operational Insights: Tracks performance metrics like no-show rates and provider utilization.
- Financial Tracking: Monitors revenue streams, payment timelines, and outstanding balances.
- Patient Demographics: Identifies trends for targeted outreach.
- Predictive Forecasting: Anticipates demand for services and resources.
Medical practice management software delivers benefits that extend far beyond administrative convenience. By combining healthcare automation, compliance, and data-driven insights, PMS helps healthcare providers run more efficient operations, deliver better patient experiences, and remain financially healthy in a competitive environment. As the healthcare sector continues to digitize, providers who leverage these systems effectively will be best positioned for sustainable growth and improved patient outcomes.
How Medical Practice Management Software Works
Medical practice management software (PMS) functions as the operational backbone of a healthcare practice, coordinating administrative, financial, and—in many cases—clinical workflows in a single, integrated environment. Understanding how it works involves examining the data flow from patient booking to billing, the integration points with external systems, the role of APIs in interoperability, and a real-world example of a patient’s journey through a PMS-powered clinic.
1. Data Flow: From Appointment Booking to Billing
The lifecycle of a patient interaction in a PMS begins well before the patient arrives at the clinic. It starts with appointment scheduling and ends with payment collection, passing through multiple checkpoints that ensure smooth operations.
Step-by-step data flow:
- Appointment Scheduling: The process starts when a patient books an appointment—either online through a self-service portal or via front desk staff. The PMS captures details such as patient demographics, preferred time slot, and reason for visit.
- Pre-Visit Verification: If the patient is insured, the system automatically runs an insurance eligibility check to confirm coverage before the visit. This step reduces claim denials later.
- Check-In and Patient Intake: Upon arrival (or virtually for telehealth), the patient’s information is verified. The PMS may link to an EHR/EMR to retrieve medical history or previous visit notes.
- Service Delivery and Documentation: The provider conducts the consultation or procedure. While this is recorded in the EHR, the PMS logs service details and maps them to billing codes for later invoicing.
- Billing and Claims: The PMS automatically generates an invoice based on the services provided, applies insurance adjustments, and—if applicable—submits a claim to the insurance company.
- Payment Processing: The patient pays their portion through integrated payment gateways, while the PMS tracks pending reimbursements from insurers.
- Reporting and Follow-Up: Finally, all data from the interaction—financial, operational, and patient-specific—is stored for reporting, analytics, and any necessary follow-up communication.
This streamlined flow reduces manual intervention, ensures accuracy, and shortens the time from service to payment.
2. Integration with External Systems
PMS is most powerful when it works in harmony with other healthcare systems. By connecting to third-party services, it ensures that all aspects of patient care and practice operations are synchronized.
Key integration points include:
- Laboratory Information Systems (LIS): Allows providers to order lab tests directly from the PMS and receive results electronically, eliminating the need for manual data entry.
- Pharmacy Management Systems: Enables e-prescribing, with prescriptions sent directly to pharmacies, improving patient convenience and reducing prescription errors.
- Insurance Provider Systems: Supports real-time eligibility verification, claim submission, and payment status tracking.
- Telehealth Platforms: Integrates video conferencing and virtual care scheduling directly into the PMS, ensuring consistent record-keeping.
- Accounting and ERP Systems: For larger healthcare organizations, PMS can link to healthcare ERP and enterprise-level accounting software for unified financial reporting.
By integrating with these systems, PMS reduces operational silos and ensures that data flows seamlessly between different components of the healthcare ecosystem.
3. Role of APIs in Interoperability
The key to these integrations lies in APIs (Application Programming Interfaces). APIs allow different software systems to communicate in a secure and standardized way. In the healthcare context, APIs make it possible for PMS to exchange data with EHRs, lab systems, payment gateways, and insurance platforms without manual intervention.
Why APIs matter in PMS:
- Standardized Communication: Using healthcare standards like HL7 and FHIR, APIs ensure that data from different systems is compatible.
- Real-Time Updates: APIs enable instant data sharing—for example, an insurance eligibility API can confirm coverage in seconds during appointment booking.
- Scalability: Practices can start with core PMS features and add integrations later without replacing the entire system.
- Security and Compliance: Well-designed healthcare APIs use encryption, authentication tokens, and audit trails to maintain HIPAA and GDPR compliance.
As healthcare moves toward greater interoperability, API-driven PMS platforms are better positioned to adapt to new technologies and regulatory demands.
4. Example Workflow of a Typical Patient Journey
To understand how all these components work together, consider this real-world scenario of a patient named Sarah visiting a multi-specialty clinic:
Step 1: Appointment Booking
Sarah books an appointment with a dermatologist using the clinic’s online portal, selecting a date and time that works for her. The PMS sends her a confirmation email and automatically reserves the time slot in the provider’s calendar.
Step 2: Insurance Verification
Before the visit, the PMS runs an automated check with Sarah’s insurance provider, confirming that dermatology consultations are covered under her plan. If there were any coverage issues, the system would flag them for staff follow-up.
Step 3: Check-In and History Review
On the day of her visit, Sarah checks in via a self-service kiosk in the waiting room. The PMS verifies her contact details and retrieves her previous dermatology visit notes from the integrated EHR.
Step 4: Consultation and Documentation
During the appointment, the dermatologist enters clinical notes into the EHR. At the same time, the PMS automatically logs the service provided and links it to the appropriate billing code.
Step 5: Billing and Claims Submission
Immediately after the consultation, the PMS generates an invoice. It applies Sarah’s insurance details, calculates her co-pay, and submits the claim electronically to the insurer. Sarah pays her co-pay on the spot using the clinic’s integrated payment terminal.
Step 6: Follow-Up and Reporting
The PMS schedules Sarah’s follow-up appointment and sends her an automated reminder. The clinic administrator later reviews reports generated by the PMS, which show the day’s total revenue, claim submissions, and upcoming appointments.
This journey demonstrates how PMS coordinates every stage of the patient experience—from booking to billing—while ensuring that administrative, financial, and clinical data remain synchronized.
A medical practice management software solution operates as the central hub of a healthcare practice’s operations. By controlling the flow of data from appointment booking to billing, integrating with external systems, and using APIs for interoperability, it ensures that both patient care and business operations run efficiently. In a healthcare environment that demands speed, accuracy, and compliance, PMS is not just a tool—it’s the foundation of modern practice management.
Medical Practice Management Software Development Step-by-Step Process
Developing a medical practice management software (PMS) is not a one-size-fits-all project—it requires a methodical approach that accounts for the specific workflows, compliance needs, and user expectations of healthcare providers. Below is a step-by-step breakdown of the full development process, from initial market research to post-launch optimization.
Step 1: Market Research and Requirement Gathering
Every successful PMS project starts with a deep understanding of the target audience and market landscape. Healthcare practices differ significantly in size, specialty, and operational complexity. A small dental clinic, for example, will have very different needs from a multi-specialty hospital.
Key activities in this stage include:
- Competitive Analysis: Reviewing existing PMS solutions to identify gaps in features, usability, or pricing.
- Stakeholder Interviews: Engaging with doctors, administrative staff, billing teams, and IT managers to understand their pain points.
- Workflow Mapping: Documenting current processes—from patient registration to billing—to ensure the new system supports or improves them.
- Feature Prioritization: Deciding on core features (scheduling, billing, claims) versus advanced ones (AI analytics, telehealth integration).
- Regulatory Review: Identifying applicable compliance frameworks like HIPAA, GDPR, or ISO 27001.
At the end of this stage, you should have a detailed requirements document that guides the entire development process.
Step 2: Choosing the Right Tech Stack
Selecting the appropriate technology stack is critical for scalability, security, and long-term maintenance. Healthcare software must handle sensitive data, high availability demands, and integration with external systems.
Key considerations for the tech stack:
- Frontend Frameworks: React, Angular, or Vue.js for responsive and intuitive user interfaces.
- Backend Technologies: Node.js, .NET, or Django for secure, high-performance server-side logic.
- Database Options: PostgreSQL or MySQL for relational data; MongoDB for document-based storage.
- Cloud Infrastructure: AWS, Microsoft Azure, or Google Cloud for reliable hosting and scalability.
- Healthcare APIs: Support for HL7, FHIR, and DICOM standards to ensure interoperability.
The choice of stack should align with the development team’s expertise and the project’s integration needs.
Step 3: UI/UX Design for Healthcare Professionals
User interface and experience design play a crucial role in adoption. Healthcare professionals often work in high-pressure environments and need software that is fast, intuitive, and accessible. A poorly designed interface can lead to user frustration, slow task completion, and even medical errors.
Best practices in UI/UX for PMS:
- Role-Based Dashboards: Different layouts for doctors, administrators, and billing staff to surface relevant information quickly.
- Minimal Click Workflows: Reducing the number of steps needed to perform common tasks, such as booking an appointment or processing a claim.
- Accessible Design: Compliance with WCAG guidelines to accommodate users with disabilities.
- Responsive Layouts: Ensuring usability across desktops, tablets, and mobile devices.
- Error Prevention: Input validation, inline guidance, and undo options to reduce data entry mistakes.
Prototyping and usability testing at this stage help validate design decisions before development begins.
Step 4: Backend Development and API Integration
The backend is the engine of a PMS, handling data processing, business logic, and communication with external systems. Development should focus on building a modular, secure, and scalable architecture.
Core backend functions include:
- User Authentication & Authorization: Role-based access control for different staff members.
- Scheduling Logic: Algorithms to manage appointments, prevent double-bookings, and handle waitlists.
- Billing and Claims Processing: Automatic invoice creation and integration with insurance APIs.
- Data Synchronization: Real-time syncing with EHR/EMR, lab systems, and pharmacy platforms.
- API-First Approach: Designing the backend with APIs to enable future integrations and mobile app development.
Healthcare APIs such as FHIR and HL7 are crucial for interoperability, ensuring the PMS can communicate with other systems without manual data transfer.
Step 5: Compliance and Security Implementation
Compliance and security are not add-ons—they must be built into the PMS from day one. Healthcare providers operate under strict regulations, and any breach can lead to severe financial penalties and reputational damage.
Security and compliance measures include:
- HIPAA and GDPR Alignment: Encryption for data at rest and in transit, secure storage, and breach notification protocols.
- Role-Based Access Controls (RBAC): Restricting access to sensitive data based on job function.
- Audit Logging: Tracking all actions taken within the system for accountability.
- Secure API Communication: Using HTTPS and OAuth 2.0 for authentication.
- Data Backup & Disaster Recovery: Regular backups and tested recovery procedures to prevent data loss.
Security should be continuously monitored and updated to address emerging threats.
Step 6: Testing (Unit, Integration, Security)
Comprehensive testing ensures the PMS works as intended before going live. In healthcare, testing is particularly critical due to the sensitivity of the data and the need for flawless operation.
Types of testing to perform:
- Unit Testing: Verifies the functionality of individual components like the appointment scheduler or billing module.
- Integration Testing: Ensures that different modules work together, such as linking patient data with billing records.
- Security Testing: Includes penetration testing, vulnerability scanning, and compliance validation.
- Performance Testing: Confirms that the system can handle high volumes of simultaneous users without slowdown.
- User Acceptance Testing (UAT): Involving real users to validate that the PMS meets operational needs.
Automated testing frameworks can speed up this process and ensure consistent quality.
Step 7: Deployment and Training
Deployment involves moving the PMS from the development environment into live production. This phase must be carefully managed to avoid disrupting ongoing operations.
Key deployment activities:
- Pilot Launch: Rolling out the system to a small group of users to detect any last-minute issues.
- Data Migration: Transferring existing patient records, billing data, and appointment histories into the new system.
- Staff Training: Conducting role-specific training sessions to ensure users are comfortable with the new workflows.
- Go-Live Planning: Coordinating launch timing to minimize patient service disruptions.
A well-executed deployment strategy ensures a smooth transition and reduces resistance to adoption.
Step 8: Post-Launch Support and Updates
Once the PMS is live, the focus shifts to ongoing support, performance monitoring, and continuous improvement. Healthcare technology is constantly evolving, and PMS must adapt to changes in regulations, technology, and patient expectations.
Post-launch priorities include:
- Helpdesk and Technical Support: Providing prompt assistance for any user issues.
- System Monitoring: Tracking uptime, performance metrics, and error logs.
- Feature Enhancements: Rolling out new features based on user feedback and market trends.
- Compliance Updates: Ensuring the PMS remains aligned with evolving regulations.
- Security Patching: Regular updates to address vulnerabilities and emerging threats.
A strong post-launch support plan is essential for maintaining user trust and maximizing the system’s lifespan.
Building a medical practice management software solution is a complex but highly rewarding endeavor when approached systematically. By following a step-by-step process—from market research to post-launch updates—developers and healthcare organizations can create a system that is secure, compliant, and truly aligned with the needs of its users. A well-executed PMS project doesn’t just digitize administrative work—it transforms the way a practice operates, improving efficiency, compliance, and patient satisfaction.
Compliance and Data Security Considerations
Medical practice management software (PMS) handles one of the most sensitive types of data in existence—personal health information (PHI). Because PHI is a prime target for cybercriminals and is subject to strict legal protections, compliance and security are not optional—they are integral to the system’s design, development, and daily operation. A secure and compliant PMS must protect patient data against unauthorized access, maintain integrity and availability, and adhere to relevant regulatory requirements in every jurisdiction where it operates.
HIPAA, HITECH, and GDPR Requirements
HIPAA (Health Insurance Portability and Accountability Act) governs how healthcare organizations in the United States handle patient data. It requires PMS platforms to implement physical, technical, and administrative safeguards to protect PHI. This includes encryption, access controls, and audit logs, as well as policies for breach notification.
HITECH (Health Information Technology for Economic and Clinical Health Act) strengthens HIPAA by expanding compliance obligations, increasing penalties for violations, and promoting the secure adoption of electronic health records.
For organizations operating in Europe or serving EU citizens, GDPR (General Data Protection Regulation) applies. GDPR mandates strict rules on personal data processing, explicit patient consent, the right to access or delete data, and timely breach notifications. It also enforces heavy fines for non-compliance—up to 4% of global annual turnover.
Key compliance expectations for PMS include:
- HIPAA Compliance: Secure PHI handling, breach reporting, and minimum necessary access principles.
- HITECH Compliance: Enhanced security requirements for EHR integration and electronic data exchange.
- GDPR Compliance: Transparent data processing, lawful consent collection, and the right to be forgotten.
- Documentation and Training: Maintaining policies and training staff to follow them.
Role-Based Access Controls and Audit Trails
Not every staff member needs access to all patient data. Role-based access control (RBAC) ensures that users only see and edit the information necessary for their job function. For example, front desk staff may have access to patient demographics and appointment schedules but not clinical notes, while doctors have full access to medical histories.
Audit trails add another layer of accountability by recording every access, edit, and deletion of patient records. These logs are critical in investigating suspicious activity, proving compliance during audits, and maintaining trust.
Best practices include:
- Granular Permissions: Defining access rights per role (e.g., doctor, nurse, billing clerk, admin).
- Just-in-Time Access: Temporary elevated permissions for special tasks.
- Immutable Audit Logs: Records that cannot be altered, with timestamps and user IDs.
- Regular Log Reviews: Automated alerts for unusual access patterns.
Data Encryption (In Transit and at Rest)
Encryption is the foundation of PHI protection. Data should be encrypted both in transit—when it is being transmitted over a network—and at rest—when stored on a server or in the cloud.
For data in transit, Transport Layer Security (TLS) 1.2+ ensures that information transmitted between the PMS and user devices cannot be intercepted or read by unauthorized parties. For data at rest, encryption algorithms like AES-256 ensure that even if storage systems are compromised, the data remains unreadable without the proper decryption keys.
Encryption essentials for PMS:
- End-to-End Encryption: Secures communication from the sender to the receiver without intermediate decryption.
- Secure Key Management: Keys stored separately from the encrypted data.
- Encrypted Backups: Ensures backup files are as secure as live systems.
- Encryption for Mobile Access: Protects data accessed through mobile devices and tablets.
Secure Cloud Hosting Considerations
Most modern PMS platforms are cloud-based, offering advantages in scalability, cost-effectiveness, and remote access. However, not all cloud hosting environments are suitable for healthcare workloads. Providers must ensure their chosen hosting platform meets healthcare-specific compliance requirements such as HIPAA, HITECH, and GDPR.
Security-focused cloud hosting practices include:
- HIPAA-Compliant Hosting Providers: Using services that offer signed Business Associate Agreements (BAAs).
- Geographic Data Residency: Ensuring that data is stored in jurisdictions that meet regulatory obligations.
- Network Segmentation: Isolating PHI databases from public-facing application servers.
- Redundancy and Disaster Recovery: Multiple data centers and failover systems to prevent downtime.
- Continuous Monitoring: Real-time detection of threats, anomalies, and attempted breaches.
For added security, healthcare organizations should consider private cloud or hybrid cloud setups that allow them to maintain direct control over the most sensitive systems while still benefiting from cloud scalability.
Regular Security Audits
Security is not a one-time project but an ongoing process. Regular audits help identify vulnerabilities before they can be exploited. In healthcare, security audits are often required by regulators, insurers, or internal governance policies.
Key types of audits for PMS:
- Penetration Testing: Simulated attacks to evaluate system resilience.
- Vulnerability Scanning: Automated tools that detect known weaknesses in code or infrastructure.
- Compliance Audits: Formal reviews to verify adherence to HIPAA, GDPR, and other frameworks.
- Configuration Reviews: Ensuring systems are set up according to security best practices.
Audits should be followed by remediation plans, staff training, and policy updates. Partnering with external cybersecurity firms can provide an unbiased assessment and ensure best-in-class protections are in place.
A secure, compliant PMS is the result of deliberate design, disciplined development, and ongoing vigilance. Regulations like HIPAA, HITECH, and GDPR set the baseline, but real trust is built through transparent operations, strong access controls, robust encryption, and proactive monitoring. In a healthcare environment where cyberattacks and data breaches are increasingly common, a PMS that prioritizes security is not just meeting legal requirements—it’s protecting patient lives and the reputation of the practice.
Technology Stack for Medical Practice Management Software
Choosing the right healthcare technology stack is a critical decision in medical practice management software (PMS) development. The stack you select will determine not only performance and scalability but also the ease of integrating compliance, security, and interoperability features. Healthcare applications must handle sensitive patient data, support complex workflows, and remain flexible enough to integrate with EHRs, insurance systems, and telehealth platforms. Below is a breakdown of the most common and effective technologies for each layer of a PMS.
Frontend Frameworks: React, Angular, Vue
The front end is the user-facing component of PMS, where healthcare staff, administrators, and sometimes patients interact with the system. It must be fast, responsive, and intuitive—especially given the time-sensitive nature of healthcare workflows.
Popular frontend options include:
- React: A component-based JavaScript library developed by Facebook, React is known for its flexibility, performance, and vast ecosystem of UI libraries. It’s particularly well-suited for building role-specific dashboards and dynamic scheduling interfaces.
- Angular: A full-featured framework by Google, Angular provides built-in support for routing, forms, and dependency injection. It’s a strong choice for large-scale PMS platforms requiring structured development and enterprise-level maintainability.
- Vue.js: Lightweight and easy to learn, Vue is popular for rapid development and smooth integration into existing applications. It’s ideal for PMS projects that need a fast, reactive UI without heavy architectural overhead.
Key considerations for the PMS frontend:
- Responsive Design: Accessible across desktops, tablets, and mobile devices.
- Accessibility Compliance: Meeting WCAG standards to accommodate users with disabilities.
- Performance Optimization: Ensuring quick load times even with large datasets.
- Real-Time Updates: For schedules, patient queues, and billing dashboards.
Backend Options: Node.js, .NET, Django
The backend handles business logic, data processing, and integration with external systems. It must be secure, reliable, and capable of processing large volumes of requests without latency.
Strong backend frameworks include:
- Node.js: A JavaScript runtime ideal for building scalable, event-driven applications. Its non-blocking architecture supports high concurrency, making it effective for PMS platforms handling simultaneous appointment bookings and billing requests.
- .NET (C#): Developed by Microsoft, .NET is robust, secure, and integrates seamlessly with enterprise healthcare environments. It’s a top choice for clinics and hospitals already using Microsoft infrastructure.
- Django (Python): A high-level framework that emphasizes security and rapid development. Django’s built-in ORM and admin panel speed up the development of compliant, data-heavy healthcare applications.
Key backend priorities for PMS:
- Role-Based Access Control (RBAC): For secure user authentication and permissions.
- Interoperability Support: Compatibility with HL7 and FHIR standards.
- Scalability: Ability to handle growth in users and transactions without performance degradation.
- API-First Design: Facilitating mobile apps, telehealth integration, and third-party services.
Database Choices: PostgreSQL, MySQL, MongoDB
The database is the heart of PMS, storing everything from patient demographics to billing history. The choice of database depends on the type and structure of data, as well as scalability needs.
Recommended database options:
- PostgreSQL: A powerful open-source relational database with advanced features like JSONB support, full-text search, and strong data integrity controls. Well-suited for PMS systems requiring complex queries and compliance auditing.
- MySQL: A widely used relational database known for speed and reliability. It’s a good fit for PMS platforms that prioritize performance over advanced relational features.
- MongoDB: A NoSQL database designed for flexibility and scalability. Ideal for PMS modules dealing with unstructured or semi-structured data, such as patient notes, chat histories, or wearable device data.
Database best practices in PMS:
- Encryption at Rest: Securing stored data with AES-256 or similar algorithms.
- High Availability: Using replication and clustering to prevent downtime.
- Backup and Recovery: Automated, encrypted backups with regular restoration testing.
- Audit Logging: Storing change histories for compliance purposes.
Cloud Deployment: AWS, Azure, GCP
Cloud deployment allows PMS platforms to scale dynamically, reduce infrastructure costs, and support remote access for multi-location healthcare organizations.
Leading cloud providers include:
- Amazon Web Services (AWS): Offers HIPAA-compliant hosting with a signed Business Associate Agreement (BAA). AWS services like RDS (databases), S3 (secure storage), and EC2 (compute) are widely used in healthcare.
- Microsoft Azure: A strong choice for organizations using Microsoft tools. Azure provides healthcare-specific compliance certifications and seamless integration with Microsoft 365 and Dynamics.
- Google Cloud Platform (GCP): Known for its AI and analytics capabilities, GCP also offers HIPAA-compliant hosting and services like BigQuery for large-scale healthcare data analysis.
Cloud deployment considerations for PMS:
- HIPAA-Compliant Hosting: Ensuring the provider signs a BAA.
- Geographic Data Residency: Hosting in regions aligned with GDPR or local laws.
- Disaster Recovery and Redundancy: Multi-zone hosting to avoid service interruptions.
- Scalable Architecture: Auto-scaling for seasonal or demand spikes.
AI & ML Tools for Analytics and Automation
Artificial intelligence and machine learning can elevate PMS from a transactional tool to a predictive, decision-support system.
AI & ML applications in PMS include:
- Predictive Scheduling: Using historical patterns to optimize appointment allocation and reduce no-shows.
- Automated Medical Coding: Natural language processing (NLP) to translate clinical notes into accurate billing codes.
- Revenue Cycle Optimization: Machine learning models that identify claim denial trends and recommend corrective actions.
- Patient Engagement Bots: AI-driven chatbots for appointment reminders, FAQs, and pre-visit forms.
Popular tools and frameworks:
- TensorFlow & PyTorch: For building custom ML models tailored to a practice’s data.
- Google AI & AWS AI Services: Prebuilt AI APIs for NLP, image analysis, and data classification.
- Microsoft Azure Cognitive Services: AI-driven tools for speech-to-text, translation, and sentiment analysis.
Integrating AI requires careful consideration of data privacy, model explainability, and regulatory compliance to ensure ethical and secure usage.
The ideal technology stack for a PMS depends on the project’s scale, integration needs, and regulatory obligations. A well-chosen stack ensures not only technical performance but also compliance, scalability, and user satisfaction. By combining proven frontend and backend frameworks, secure database solutions, compliant cloud infrastructure, and intelligent AI capabilities, healthcare organizations can build PMS platforms that are future-ready and aligned with modern care delivery.
Cost of Developing Medical Practice Management Software
The cost of developing medical practice management software (PMS) can vary widely—from as low as $40,000 for a minimal viable product (MVP) to $300,000+ for a full-scale enterprise solution. Pricing depends on multiple factors, including feature set, software complexity, technology stack, and the geographic location of the development team. Understanding these cost drivers and planning strategically can help healthcare providers and startups balance budget constraints with the need for a secure, scalable, and compliant platform.
Factors Influencing Cost
Several variables determine the overall investment required to develop PMS:
- Feature Set:
The number and sophistication of features have the biggest impact on cost. Core functionalities like scheduling, billing, and patient record management are cheaper to implement than advanced capabilities such as AI-driven analytics, telehealth integration, or multi-location support.
- Complexity of Workflows:
A single-location clinic PMS is less complex than a multi-specialty, multi-location hospital solution that requires custom role hierarchies, interoperability with multiple EHR systems, and specialized billing workflows.
- Integration Requirements:
Integrating with insurance providers, lab systems, pharmacy platforms, and national health databases increases development effort and testing needs.
- Compliance and Security:
Building HIPAA, GDPR, and HITECH compliance into the software from day one involves encryption, audit logging, secure API communication, and regular security audits—each adding to cost.
- Location of Development Team:
Development rates vary significantly:
- North America & Western Europe: $80–$200/hour
- Eastern Europe: $40–$80/hour
- India & Southeast Asia: $25–$60/hour
- North America & Western Europe: $80–$200/hour
Breakdown of MVP vs. Full-Scale Product Costs
Healthcare organizations often choose to start with a healthcare MVP before investing in a full-featured PMS.
MVP (Minimum Viable Product) – $40,000–$80,000
Includes essential features to get the software operational for core administrative needs:
- Patient scheduling and appointment management
- Basic billing and invoicing
- Simple patient record management
- Role-based access controls
- Basic reporting
The MVP approach reduces time-to-market (typically 4–6 months) and allows real-world feedback before committing to additional investment.
Full-Scale Product – $120,000–$300,000+
Includes advanced, enterprise-ready capabilities:
- Telehealth and virtual care integration
- Insurance verification and electronic claims management
- Multi-location and multi-specialty support
- Inventory management
- Advanced analytics and AI-powered insights
- Custom integrations with EHR/EMR, labs, pharmacies, and accounting systems
- Fully optimized UI/UX for all roles
Full-scale development typically takes 9–18 months, depending on complexity and team size.
Ongoing Maintenance and Update Expenses
Healthcare development costs don’t end at launch. PMS systems require continuous monitoring, updates, and compliance adjustments to remain secure and effective.
Typical ongoing costs (per year):
- Bug Fixes & Technical Support: $5,000–$15,000
- Feature Enhancements & UI Updates: $10,000–$50,000
- Compliance & Security Updates: $5,000–$20,000
- Cloud Hosting & Infrastructure: $200–$1,000+ per month, depending on usage
- Regular Security Audits: $5,000–$10,000 annually
A good rule of thumb is to budget 15–25% of the initial development cost annually for maintenance and upgrades.
How to Optimize Cost Without Compromising Quality
Healthcare organizations can take strategic steps to control development costs while still building a high-quality PMS:
- Start with an MVP:
Focus on core features first, then expand based on real-world usage and feedback.
- Prioritize Integrations:
Not all integrations are essential from day one. Implement those that deliver the highest operational benefit first.
- Leverage Open-Source Components:
Use secure, well-maintained open-source frameworks and libraries to reduce development time.
- Adopt Agile Development:
Build in iterative sprints to adjust features mid-project and avoid costly rework.
- Outsource to Cost-Efficient Regions:
Partnering with experienced teams in India or Eastern Europe can reduce costs without sacrificing quality—provided the vendor has strong healthcare compliance experience.
- Cloud Over On-Premise:
Cloud deployment reduces upfront hardware investment and ongoing maintenance overhead.
The investment in PMS should be viewed in the context of long-term ROI rather than short-term expense. Even at the higher end of the cost spectrum, a well-designed PMS can pay for itself quickly by improving revenue cycle management, reducing administrative labor, and enhancing patient satisfaction. The key is to plan strategically—starting lean with an MVP, scaling based on actual needs, and ensuring every dollar spent aligns with measurable operational or patient care benefits.
Challenges in Development and Implementation
While medical practice management software (PMS) can transform healthcare operations, building and deploying it successfully comes with unique challenges. These obstacles stem from the sector’s heavy regulatory demands, complex data ecosystems, and the human factors that influence technology adoption. Addressing these issues early in the development cycle can significantly increase the chances of a smooth, cost-effective rollout.
1. Regulatory Compliance Challenges
Healthcare is one of the most heavily regulated industries, and PMS must meet strict legal requirements around data privacy, security, and record handling. In the United States, HIPAA and HITECH dictate how personal health information (PHI) is stored, transmitted, and accessed. In the European Union and UK, GDPR enforces equally stringent standards, with additional emphasis on patient consent and the right to data erasure.
The challenge is that regulations are not static—they evolve, and new compliance obligations may emerge after the system is deployed. Developers must anticipate these changes and build flexibility into the software’s architecture to adapt without costly rewrites.
Key pain points include:
- Multi-Jurisdiction Compliance: Serving patients in multiple regions often means meeting overlapping but different rules.
- Audit-Readiness: Maintaining logs, documentation, and policies that satisfy regulator audits.
- Secure Data Sharing: Balancing interoperability with strict privacy controls.
- Continuous Updates: Adjusting systems as laws change without disrupting operations.
2. Data Migration from Legacy Systems
Many healthcare providers already use older software or even paper-based systems for scheduling, billing, and records. Migrating this historical data into a new PMS is one of the most technically demanding parts of implementation.
Legacy systems often store data in incompatible formats, making automated migration difficult. Incomplete or inaccurate records also pose risks, as incorrect data can undermine patient care and billing accuracy. Successful healthcare migration requires careful planning, robust data mapping, and thorough validation before the system goes live.
Common migration challenges include:
- Data Quality Issues: Missing fields, duplicate entries, or outdated information.
- Format Incompatibility: Legacy databases not matching the new PMS schema.
- Downtime During Transition: Avoiding disruptions to patient care while data is moved.
- Validation and Testing: Ensuring migrated data is accurate and complete before launch.
3. Integration with Third-Party Healthcare Systems
A PMS rarely operates in isolation—it must interact with EHR/EMR platforms, lab information systems, insurance provider portals, pharmacy management systems, and sometimes even national health databases. Each integration point adds complexity and potential points of failure.
Some external systems use outdated APIs or proprietary formats, making interoperability more difficult. Additionally, compliance requirements mean that data transfers must be secure and properly logged, further increasing development time and cost.
Integration hurdles include:
- API Limitations: Restricted or poorly documented third-party APIs.
- Standards Variability: Different systems using HL7, FHIR, or custom formats.
- Latency Issues: Slow or unreliable data exchange impacting workflows.
- Security Constraints: Ensuring secure, encrypted communication without breaking compatibility.
4. User Adoption and Training Issues
Even the most feature-rich PMS can fail if end-users don’t embrace it. Healthcare staff often have established routines, and switching to a new system can be perceived as disruptive—especially in busy clinics or hospitals where time is scarce.
Resistance is most likely when the new system is perceived as complicated, unintuitive, or slower than existing methods. Without proper training, staff may revert to old habits, undermining the return on investment.
Barriers to adoption include:
- Learning Curve: Complexity of features overwhelming new users.
- Time Constraints: Staff unable to dedicate time for thorough training.
- Change Resistance: Preference for familiar workflows over new ones.
- Perceived Inefficiency: Early glitches or slow performance causing frustration.
Best practices to improve adoption:
- Conduct role-specific training sessions tailored to how each user will interact with the system.
- Implement pilot programs with small user groups before a full rollout.
- Gather feedback loops during the early stages to fix usability issues quickly.
- Provide on-demand support resources like video tutorials, chat support, and quick-reference guides.
The road to a successful PMS implementation is as much about strategy and change management as it is about coding and infrastructure. Regulatory complexity, messy legacy data, integration hurdles, and user resistance can derail a project if they’re not addressed early. By approaching development with compliance expertise, a robust migration plan, integration flexibility, and a user-first training approach, healthcare providers can navigate these challenges and unlock the full value of their investment.
Future of Medical Practice Management Software
Medical practice management software (PMS) is moving beyond administrative automation into a new era where advanced technologies like artificial intelligence (AI), predictive analytics, blockchain, and fully integrated telehealth ecosystems are redefining what’s possible. The future PMS will not only streamline operations but also proactively support clinical decision-making, strengthen data security, and enhance patient engagement.
1. AI-Driven Decision Support
AI will increasingly serve as a real-time assistant for healthcare providers and administrators, helping them make faster, more informed decisions. By analyzing historical patient data, appointment patterns, billing trends, and even clinical notes (via integration with EHR/EMR), AI-powered PMS modules can surface actionable recommendations on scheduling, staffing, and revenue optimization.
In clinical contexts, AI could help flag urgent cases based on patient-reported symptoms or vital signs collected through wearables, ensuring timely intervention. For administrators, AI might suggest rescheduling patients likely to cancel or flag anomalies in insurance claims before submission.
Potential capabilities include:
- Appointment Optimization: Recommending schedule adjustments to minimize no-shows.
- Claims Accuracy Checks: Using natural language processing (NLP) to validate billing codes.
- Patient Risk Alerts: Flagging cases requiring immediate follow-up based on historical patterns.
- Staffing Recommendations: Matching staffing levels to predicted patient demand.
2. Predictive Analytics for Patient Outcomes
Predictive analytics moves PMS from being a reactive tool to a proactive one. By leveraging large datasets—including demographics, historical visits, and social determinants of health—PMS systems will forecast patient needs and outcomes.
For example, a predictive model might identify which chronic care patients are at risk of missing follow-up appointments, allowing clinics to intervene early. Similarly, PMS could forecast seasonal appointment spikes (e.g., flu season) and recommend resource allocation accordingly.
Key use cases include:
- Preventive Care Outreach: Identifying patients due for screenings or vaccinations.
- Risk Stratification: Segmenting patients by likelihood of hospital readmission.
- Demand Forecasting: Anticipating busy periods for staff and facility planning.
- Treatment Plan Effectiveness: Measuring outcomes over time to refine care protocols.
By turning data into foresight, predictive analytics supports both better patient care and more efficient resource management.
3. Blockchain for Secure Patient Records
Blockchain’s potential in PMS lies in its ability to create tamper-proof, decentralized records that can be securely shared across providers, payers, and patients. Unlike traditional databases, blockchain entries are immutable—once a transaction (such as a patient record update) is logged, it cannot be altered without leaving a permanent trace.
This could address one of healthcare’s most persistent challenges: ensuring secure, interoperable access to accurate patient data. Blockchain-based PMS could allow patients to control who accesses their records, while giving providers confidence in the authenticity of the data.
Advantages of blockchain in PMS include:
- Immutable Audit Trails: Every data change is recorded and time-stamped.
- Patient-Controlled Access: Smart contracts enabling patients to grant and revoke data permissions.
- Cross-Organization Data Exchange: Secure interoperability between hospitals, clinics, and insurers.
- Fraud Prevention: Reducing insurance fraud through transparent, verifiable records.
4. Full Telehealth Ecosystem Integration
Telehealth adoption surged during the COVID-19 pandemic, and PMS systems are evolving to make virtual care a permanent fixture of healthcare delivery. The next generation of PMS will integrate telehealth not as an add-on but as a core component of patient care.
A fully integrated telehealth ecosystem means that virtual consultations, patient intake, billing, and follow-ups all happen seamlessly within the same platform. It also opens the door for hybrid care models, where patients switch between in-person and online visits without friction.
Future telehealth capabilities in PMS include:
- Unified Scheduling: Booking both in-person and virtual visits from one interface.
- Integrated Clinical Documentation: Recording telehealth visit notes directly into patient records.
- Remote Monitoring Integration: Incorporating data from wearable devices and home health kits.
- Multi-Specialty Virtual Care: Coordinating joint telehealth sessions with multiple providers.
By embedding telehealth deeply into PMS, providers can expand access to care, reduce overhead costs, and offer more flexibility to patients.
The future of medical practice management software lies in intelligence, security, and seamless care delivery. AI-driven decision support will make operations smarter, predictive analytics will enable proactive patient care, blockchain will safeguard and decentralize sensitive health data, and full telehealth integration will redefine accessibility. Providers that adopt these innovations early will be better positioned to deliver efficient, patient-centered care while maintaining a competitive edge in an increasingly digital healthcare landscape.
Why Choose Aalpha for Medical Practice Management Software Development
Selecting the right technology partner for medical practice management software (PMS) development is as important as choosing the right features or tech stack. Being a top-rated healthcare software development company-at Aalpha Information systems, we bring a proven track record in healthcare technology, a compliance-first mindset, and the ability to deliver tailor-made solutions that meet the operational and clinical needs of diverse medical specialties.
Experience in Healthcare Software Projects
Healthcare technology demands a deep understanding of complex workflows, regulatory obligations, and the unique challenges of clinical environments. Aalpha has successfully delivered software projects for hospitals, specialty clinics, diagnostic centers, and healthcare startups across the USA, Europe, and the UK.
Our team is skilled at mapping real-world medical processes—such as patient intake, scheduling, billing, insurance verification, and telehealth—into intuitive, high-performing digital platforms. We understand the nuances of integrating with EHR/EMR systems, laboratory information systems, and insurance provider networks, ensuring that your PMS functions seamlessly in a connected healthcare ecosystem.
Compliance-First Approach
Compliance is not an afterthought—it’s embedded into our development process from day one. Whether your practice operates under HIPAA and HITECH in the United States, GDPR in Europe, or other regional healthcare regulations, we design systems that meet and exceed data privacy and security standards.
Our compliance-focused practices include:
- Role-Based Access Control (RBAC): Limiting access to sensitive data based on job function.
- Audit Logging: Maintaining immutable records of data access and changes.
- End-to-End Encryption: Securing data both in transit and at rest.
- Regular Security Testing: Conducting penetration testing and vulnerability scans before launch.
This compliance-first mindset reduces legal risks, safeguards patient trust, and ensures long-term system integrity.
Custom Solutions for Different Medical Specialties
No two healthcare practices are alike, and a “one-size-fits-all” PMS rarely meets the unique needs of different medical specialties. At Aalpha, we design custom PMS solutions for general practitioners, dental clinics, dermatology practices, multi-specialty hospitals, and more.
For example:
- Dental Practices: PMS modules for treatment plan scheduling and imaging integration.
- Specialty Clinics: Advanced inventory management for high-value medical supplies.
- Multi-Location Hospitals: Centralized dashboards for managing resources across sites.
By tailoring workflows, user interfaces, and reporting features to your specialty, we ensure higher staff adoption rates and better patient outcomes.
End-to-End Development and Support
Our services go beyond initial development—we partner with clients through every phase of the PMS lifecycle:
- Discovery & Requirements Gathering: Understanding your workflows and priorities.
- Design & Development: Building intuitive, scalable, and compliant systems.
- Integration: Connecting your PMS with EHR, telehealth, labs, pharmacies, and insurance networks.
- Deployment & Training: Ensuring a smooth transition with minimal downtime.
- Post-Launch Support: Providing updates, compliance adjustments, and technical assistance.
With a dedicated support team, we ensure that your PMS remains secure, compliant, and aligned with your evolving operational needs.
The Aalpha Advantage
By combining healthcare domain expertise, a rigorous compliance framework, and a commitment to delivering fully customized solutions, Aalpha helps medical providers streamline operations, improve revenue cycles, and enhance patient experiences. Whether you are a small practice looking to digitize operations or a large healthcare network seeking a robust, multi-location system, Aalpha delivers the expertise and reliability needed to succeed in today’s competitive healthcare market.
Medical practice management software has evolved into an essential tool for modern healthcare providers, enabling them to streamline operations, maintain compliance, and deliver better patient experiences. From automating administrative tasks and optimizing revenue cycles to integrating telehealth and predictive analytics, PMS plays a central role in improving both clinical and operational efficiency.
In an era where patient expectations are higher, regulations are stricter, and competition is intense, investing in a well-designed, secure, and scalable PMS is not just a technology upgrade—it’s a strategic necessity. The right platform can reduce costs, increase productivity, and empower healthcare teams to focus more on delivering quality care instead of managing paperwork and manual processes.
At Aalpha, we specialize in developing custom medical practice management software tailored to the specific needs of healthcare providers. With deep domain expertise, a compliance-first approach, and end-to-end development capabilities, we help clinics, hospitals, and specialty practices implement solutions that are secure, user-friendly, and future-ready.
If you are ready to transform your practice operations, enhance patient satisfaction, and ensure regulatory compliance, Aalpha can be your trusted partner in building a PMS that delivers measurable results.
FAQs — Medical Practice Management Software Development
1. How long does it take to develop medical practice management software?
An MVP with core features (scheduling, billing, basic records) takes 4–6 months. A full-scale solution with telehealth, insurance automation, and analytics can take 9–18 months. Timeline depends on features, integrations, compliance needs, and team size.
2. Can it be integrated with existing EHR systems?
Yes. PMS can connect with EHR/EMR platforms using HL7 or FHIR standards, enabling seamless data flow between clinical and administrative systems. Integration complexity depends on your EHR provider’s APIs and security protocols.
3. What’s the difference between practice management software and hospital management software?
- PMS: Focuses on admin and financial tasks for clinics—scheduling, billing, insurance, and patient communication.
- HMS: Hospital management software covers wider hospital operations, including inpatient care, pharmacy, and surgical scheduling. PMS suits outpatient/specialty practices; HMS fits large hospitals.
4. How much does it cost to maintain the software annually?
Maintenance is typically 15–25% of the initial build cost. This covers bug fixes, updates, compliance patches, hosting, and backups. For a $100,000 system, budget $15,000–$25,000 per year.
5. Is cloud-based or on-premise better for a clinic?
For most small to mid-sized clinics, cloud-based PMS is better—lower upfront cost, easier updates, remote access, and built-in security. On-premise is preferred only when local control or offline access is essential.
6. How to ensure HIPAA compliance?
Choose a vendor experienced in healthcare regulations. Ensure the PMS has encryption, role-based access, audit logs, secure hosting, and documented breach response protocols. Regular security audits are essential.
7. Can small clinics afford custom development?
Yes, especially if starting with an MVP. Cloud-based deployment, open-source components, and phased feature rollouts can keep costs manageable while delivering the most-needed features first.
8. What’s the ROI timeline for implementing the software?
Most practices see ROI in 6–18 months through reduced admin workload, fewer billing errors, faster claims, and higher patient retention. The speed of return depends on adoption rate and operational efficiency gains.
Contact Aalpha today to build a secure, custom medical practice management software that optimizes your operations and improves patient care.



Share This Article:
Written by:
Stuti Dhruv
Stuti Dhruv is a Senior Consultant at Aalpha Information Systems, specializing in pre-sales and advising clients on the latest technology trends. With years of experience in the IT industry, she helps businesses harness the power of technology for growth and success.
Stuti Dhruv is a Senior Consultant at Aalpha Information Systems, specializing in pre-sales and advising clients on the latest technology trends. With years of experience in the IT industry, she helps businesses harness the power of technology for growth and success.