Telemedicine apps are digital platforms that enable remote delivery of healthcare services using telecommunications technology. They facilitate direct interaction between patients and healthcare providers, allowing diagnosis, consultation, treatment, and monitoring without requiring in-person visits. Telemedicine apps cover a wide spectrum of services including video consultations, remote patient monitoring, appointment scheduling, prescription management, and health education.
The scope of telemedicine apps extends beyond simple video calls. Advanced platforms integrate electronic health records (EHR), artificial intelligence (AI) for symptom checking, and connectivity with wearable devices. These apps can serve diverse healthcare domains such as primary care, mental health, chronic disease management, and even specialized fields like dermatology or cardiology.
Importance in Modern Healthcare Delivery
Telemedicine apps have transformed healthcare delivery by addressing several longstanding challenges. Geographical barriers, especially in rural or underserved areas, often limit access to timely medical care. Telemedicine bridges this gap, providing patients with convenient and often faster access to medical expertise.
Additionally, telemedicine improves healthcare system efficiency. By reducing unnecessary in-person visits, it alleviates pressure on clinics and hospitals, lowers healthcare costs, and minimizes risks of infectious disease transmission—a critical benefit during outbreaks like COVID-19.
For patients, telemedicine apps enhance engagement and self-management of health by offering continuous monitoring and easy communication channels with providers. For healthcare providers and institutions, these apps expand patient reach, improve care coordination, and enable data-driven decision-making through integrated health analytics.
Historical Context and Evolution of Telemedicine Technology
The concept of delivering healthcare remotely dates back several decades, evolving alongside advancements in communication technologies.
- Early Beginnings: The 1960s and 1970s saw the first telemedicine experiments using basic telephone and radio transmissions to connect isolated patients with specialists. NASA’s space programs played a pioneering role by developing remote monitoring systems to track astronauts’ health.
- 1990s Expansion: The rise of the internet in the 1990s catalyzed telemedicine growth, allowing more sophisticated video conferencing and data exchange. Health organizations began pilot projects connecting rural clinics to urban hospitals.
- 2000s to Early 2010s: Increasing broadband penetration and mobile device adoption accelerated telemedicine innovation. Regulatory frameworks and reimbursement models started to develop, although adoption remained limited by technological and infrastructural challenges.
- COVID-19 Pandemic Surge: The global COVID-19 pandemic in 2020 forced an unprecedented shift toward remote care. Social distancing and lockdowns necessitated rapid deployment and scaling of telemedicine apps worldwide. Regulatory agencies temporarily relaxed restrictions, expanding coverage and reimbursement. Telemedicine went from a niche service to a mainstream healthcare delivery model virtually overnight.
- Current State: Today, telemedicine apps incorporate advanced features like AI-driven diagnostics, integration with wearable health devices, and interoperability with electronic medical records. The technology continues to mature, supported by expanding regulatory clarity, investment, and patient demand.
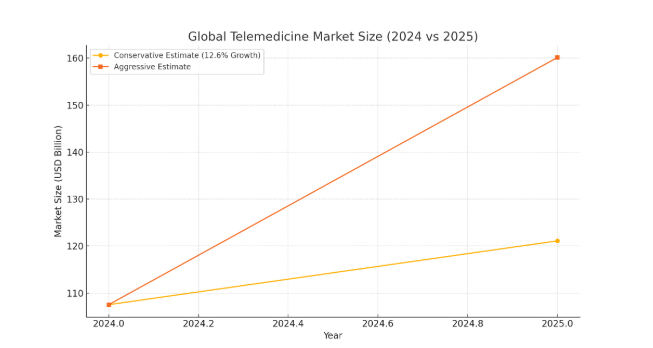
Telemedicine Market Size and Growth Projection
Global Telemedicine Market Size (2025)
As of 2025, the global telemedicine market is projected to reach approximately USD 121.10 billion, up from USD 107.52 billion in 2024, reflecting a year-over-year growth of about 12.6%. Another estimate places the 2025 market size at USD 160.13 billion, indicating a more aggressive growth trajectory. This growth is fueled by increasing demand for remote healthcare services, technological advancements, and supportive regulatory environments.
Compound Annual Growth Rate (CAGR) and Growth Drivers
The telemedicine market is expected to grow at a CAGR ranging between 17.5% and 19.9% from 2025 to 2030 . Key drivers of this growth include:
- Demographic Shifts: An aging global population and the increasing prevalence of chronic diseases necessitate accessible and continuous healthcare services.
- Technological Advancements: Improvements in broadband connectivity, mobile technology, and the integration of AI and IoT devices enhance the feasibility and effectiveness of telemedicine solutions.
- Regulatory Support: Governments worldwide are implementing policies and reimbursement models that favor telemedicine adoption, especially in the wake of the COVID-19 pandemic.
Regional Market Analysis
- North America: This region continues to dominate the telemedicine market, accounting for approximately 47.94% of the global market share in 2024 . The U.S. market alone is projected to grow from USD 94.3 billion in 2025 to USD 395.6 billion by 2034, at a CAGR of 17.3%.
- Europe: European countries are experiencing steady growth in telemedicine adoption, driven by supportive healthcare policies and increasing demand for remote healthcare services.
- Asia-Pacific: This region is witnessing rapid growth due to large populations, increasing internet penetration, and government initiatives promoting digital health. For instance, India’s Telangana state has seen telemedicine usage rise from 5.3 million users in 2022–23 to a projected 8.7 million by March 2025.
Key Industry Players and Market Share
The telemedicine market is characterized by a mix of established companies and emerging startups. As of early 2025, leading providers by market share include:
- Zoom Video Communications: 22.83%
- Amwell: 8.30%
- Doxy.me: 7.15%
- Cisco Systems: 6.63%
- Teladoc Health: 6.20%
These companies offer a range of services, from video conferencing platforms to comprehensive virtual care solutions.
Impact of COVID-19 on Market Acceleration
The COVID-19 pandemic significantly accelerated the adoption of telemedicine. Lockdowns and the need for social distancing made remote healthcare services essential. Regulatory bodies relaxed certain restrictions, allowing for broader use and reimbursement of telemedicine services. This period served as a catalyst, leading to increased investment and innovation in the sector.
Forecast for the Next 5–10 Years
Looking ahead, the telemedicine market is expected to continue its robust growth. Projections indicate that the market could reach USD 432.31 billion by 2032, maintaining a CAGR of 19.9% . Another forecast suggests the market could surpass USD 709.69 billion by 2034, growing at a CAGR of 17.99% from 2025 to 2034.
Reasons why people choose telemedicine apps
People are gradually losing their apprehension towards electronic healthcare devices. Their faith goes up, and those apps are becoming more appreciated because they are:
- Swift Responses
Individuals who have a minor health concern or are too ill to visit a specialist in person save time from not having to go to a pharmacy, fill out patient paperwork, and stay in a waiting room.
- Emergency.
These applications help reduce emergency department visits by addressing common cold-related infections, some respiratory disorders (e.g., asthma), allergies, eye and skin problems, muscle strains, wounds, bruises, and discomfort, among other things.
- It is convenient.
Telemedicine simplifies the process of obtaining required doctor’s records, such as a job or school reasons for patients who need a day or two to heal. After a physician updates the form, the patient receives a notification that the note is ready for printing or emailing.
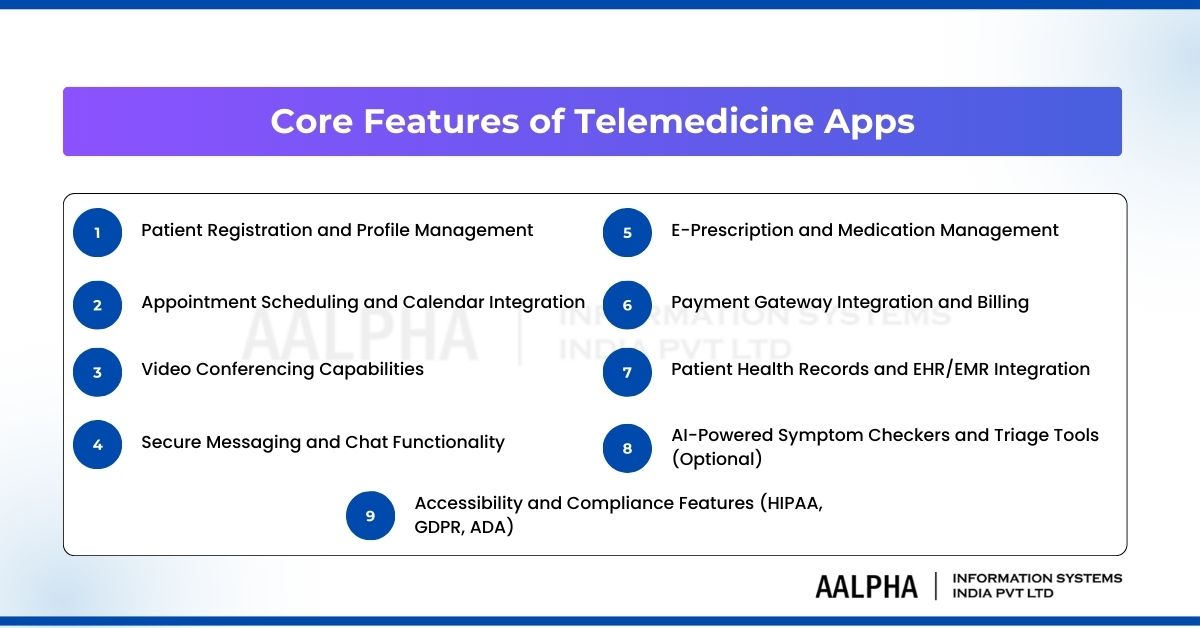
Core Features of Telemedicine Apps
The functionality of a telemedicine app must address the needs of both patients and healthcare providers, ensuring seamless, secure, and compliant delivery of virtual healthcare services. Below is a comprehensive overview of the essential features required for a fully functional, scalable, and regulation-compliant telemedicine application.
1. Patient Registration and Profile Management
The user onboarding experience is foundational. Patients should be able to register and create profiles through multiple methods—email, phone OTP verification, or third-party integrations like Google or Apple accounts.
Key capabilities include:
- Profile details: Personal information (age, gender, contact info), medical history, insurance details, and emergency contacts.
- Identity verification: Integration with digital ID verification services or KYC systems where required.
- Provider-side dashboard: Healthcare professionals should be able to view and manage patient data with role-based access controls (RBAC).
A well-structured profile management system is essential to ensure accurate diagnosis, personalized care, and proper regulatory documentation.
2. Appointment Scheduling and Calendar Integration
Doctor appointment scheduling is one of the most frequently used features in any telemedicine application. It must support:
- Real-time availability: Doctors should be able to set and update their availability in real time.
- Patient booking system: Patients can choose time slots based on specialty, provider, language, or location preferences.
- Calendar sync: Integration with Google Calendar, Outlook, and Apple Calendar enhances usability for providers and patients alike.
- Automatic reminders: SMS, email, or push notification alerts reduce no-shows and optimize provider efficiency.
Advanced platforms also include rescheduling workflows, waitlist management, and automated appointment confirmations.
3. Video Conferencing Capabilities
High-quality video consultations form the backbone of telemedicine services. Video features must prioritize:
- Low-latency performance: Platforms like WebRTC offer real-time communication with minimal lag.
- Cross-platform compatibility: The feature must work on iOS, Android, and web browsers without requiring third-party installations.
- Multi-party support: Group consultations (e.g., patient + doctor + caregiver) should be supported.
- Session recording: Optional recording for legal documentation, follow-up care, or quality control (with patient consent).
Leading services like Teladoc and MDLIVE invest heavily in customized video engines or integrate third-party APIs like Vonage, Twilio Video, or Agora for performance and scalability.
4. Secure Messaging and Chat Functionality
In-app messaging enables asynchronous communication between patients and providers.
Core features include:
- Encrypted chat: End-to-end encryption (E2EE) ensures privacy.
- Real-time chat: Typing indicators, read receipts, and online presence.
- File sharing: Ability to send lab reports, prescriptions, and diagnostic images securely.
- Asynchronous support: Providers can respond when available, offering flexibility for non-urgent interactions.
HIPAA and GDPR compliance must be enforced for all messages. Providers like TigerConnect offer prebuilt, HIPAA-compliant chat modules for healthcare apps.
5. E-Prescription and Medication Management
The e-prescription module allows doctors to issue digital prescriptions post-consultation, viewable instantly by patients and shareable with pharmacies.
Must-have functionalities:
- Prescription templates: Predefined medication suggestions for frequent conditions.
- Pharmacy integration: Linking with pharmacy APIs (e.g., SureScripts in the US) for direct transmission.
- Medication reminders: Push notifications or SMS reminders to patients for medication adherence.
- Medication history: Centralized repository for patients and providers to view historical prescriptions.
In the U.S., the DEA mandates e-prescribing for controlled substances (EPCS). Therefore, telemedicine apps must comply with this standard and obtain appropriate certifications.
6. Payment Gateway Integration and Billing
Billing infrastructure should support multiple payment methods and adhere to regional financial regulations.
Functionality to include:
- Digital payments: Support for credit/debit cards, mobile wallets (Google Pay, Apple Pay), and UPI (for India).
- Insurance claims: Integration with insurance providers for eligibility verification and claims processing.
- Invoicing: Auto-generated invoices sent post-session to the patient’s account and email.
- Subscription models: For platforms offering membership-based plans, recurring billing and plan management are essential.
PCI-DSS compliance is mandatory for any feature processing cardholder data. Tools like Stripe and Braintree offer healthcare-grade APIs for secure transaction management.
7. Patient Health Records and EHR/EMR Integration
Access to longitudinal patient health data is critical for effective remote care. A robust EHR/EMR integration module is necessary to enable continuity of care.
Features to support:
- Patient health summaries: Auto-generated or manually uploaded health records accessible to both provider and patient.
- FHIR or HL7 integration: For interoperability with existing hospital systems and insurance platforms.
- Lab reports and diagnostics: Upload, view, and annotate lab data, radiology reports, and other diagnostic documents.
- Role-based permissions: Restrict access based on the provider’s role and patient consent.
Most U.S.-based systems are now aligning with HL7 FHIR standards, which enable smoother data exchange across platforms.
8. AI-Powered Symptom Checkers and Triage Tools (Optional)
While not core to every platform, AI in healthcare is increasingly being adopted through AI-based tools to improve efficiency and decision support.
AI capabilities might include:
- Symptom checker bots: Users input symptoms and receive probable conditions or advice to consult a doctor.
- Urgency triage: Algorithms determine whether a user should visit the ER, book a virtual appointment, or follow home care instructions.
- NLP-based intake forms: Conversational interfaces that capture pre-visit data more naturally.
For example, Babylon Health employs AI triage systems that have processed millions of patient interactions, reducing waiting times and clinical burden.
These features require extensive testing and certification, especially if they’re used for decision support. Explainability, clinical validation, and ethical compliance are essential before deployment.
9. Accessibility and Compliance Features (HIPAA, GDPR, ADA)
To be legally and ethically viable, a telemedicine platform must incorporate stringent data privacy and accessibility measures.
Key compliance considerations:
- HIPAA (USA): Apps must ensure confidentiality, integrity, and availability of health data. Features like encrypted data transfer, audit logs, and secure user authentication are non-negotiable.
- GDPR (Europe): Explicit user consent, data minimization, and right to erasure must be built into the app’s design.
- ADA & WCAG: Accessibility standards for users with visual, hearing, or motor impairments. Apps should offer screen reader compatibility, closed captions for video consultations, and keyboard navigation.
Security features such as 2FA, data-at-rest encryption, user activity logging, and role-based access controls are standard across enterprise-grade platforms.
Example Apps and Real-World Implementations
Several leading telemedicine platforms exemplify how these features are implemented at scale:
- Teladoc Health: Offers a fully integrated experience with video consultations, mental health services, e-prescriptions, and chronic care management. Compliant with HIPAA and HITRUST.
- MDLIVE: Provides urgent care, dermatology, and therapy services with real-time doctor availability, robust scheduling, and secure messaging.
- Amwell: Integrates directly into hospital EHR systems using HL7/FHIR and supports complex workflows like multi-specialty coordination and post-discharge virtual visits.
- Doctor on Demand: Includes mental health support, medical consultations, and pharmacy integration with transparent pricing and insurance compatibility.
- Practo (India): Offers regional language support, online doctor consultations, and medicine delivery services tailored for the Indian market.
These platforms serve as practical benchmarks for any new product entering the market and demonstrate the scalability and modularity of feature design in telemedicine systems.
Each feature of a telemedicine app contributes directly to patient satisfaction, provider efficiency, and regulatory compliance. While the core features like video calls, appointment booking, and prescription handling are universally required, platforms that differentiate themselves often do so by embedding AI support, seamless EHR integration, and user-centric design.
Technology Stack for Telemedicine App Development
Building a reliable, compliant, and scalable telemedicine application requires selecting a robust technology stack. Each component—frontend, backend, infrastructure, communication layers, security, and DevOps—must be carefully chosen to address the demands of healthcare applications, including performance, privacy, interoperability, and maintainability.
This section explores the key technology options and frameworks typically used in modern telemedicine app development.
Frontend Technologies
The frontend of a telemedicine app must offer high performance, intuitive navigation, accessibility, and compatibility across mobile and web platforms.
1. React Native
React Native, backed by Meta (formerly Facebook), enables the development of cross-platform apps using JavaScript. It allows for near-native performance with a single codebase for iOS and Android.
- Advantages: Faster development cycles, shared codebase, active community.
- Use cases: Real-time chat, patient dashboards, appointment booking interfaces.
2. Flutter
Flutter, developed by Google, is a UI toolkit that compiles to native ARM code and renders through its own graphics engine.
- Advantages: Consistent UI across platforms, rich widgets, high performance.
- Use cases: Apps needing pixel-perfect design, video call UIs, prescription views.
3. Swift (iOS) and Kotlin (Android)
For healthcare apps requiring optimized device-specific capabilities—like Bluetooth-enabled medical device integration or AR-assisted diagnostics—native development may be preferred.
- Swift: Fast, secure, and modern programming language for iOS.
- Kotlin: Google’s preferred language for Android, offering concise syntax and full Java interoperability.
Backend Technologies
The backend supports business logic, session handling, user management, data processing, and integration with third-party APIs.
1. Node.js
A non-blocking, event-driven server runtime, Node.js is suitable for applications requiring high concurrency, such as video streaming and chat.
- Libraries: Express.js (web server), Socket.IO (real-time events).
- Pros: Scalable, JSON-native, extensive ecosystem.
2. Python/Django
Django is a high-level Python web framework suitable for rapid development and clean design.
- Benefits: Built-in admin interface, ORM, and robust security middleware.
- Use cases: Health record management, authentication, appointment logic.
3. Ruby on Rails
Known for its opinionated convention-over-configuration approach, Ruby on Rails is well-suited for MVPs or quickly evolving platforms.
- Strengths: Developer productivity, mature libraries for scheduling and billing.
- Consideration: May not match Node.js or Django for real-time scalability.
Cloud Infrastructure and Hosting
Telemedicine platforms must support dynamic scaling, global reach, and strict security standards. Major cloud providers offer healthcare-compliant services.
1. Amazon Web Services (AWS)
- Services: EC2 (compute), RDS (database), S3 (storage), CloudWatch (monitoring).
- Compliance: HIPAA-eligible services under Business Associate Addendum (BAA).
- Healthcare tools: Amazon HealthLake (FHIR-compatible health data processing).
2. Microsoft Azure
- Services: App Service, Azure Cosmos DB, Azure Active Directory.
- Advantages: Seamless integration with enterprise environments.
- Compliance: HITRUST CSF, HIPAA, GDPR, and ISO/IEC 27001.
3. Google Cloud Platform (GCP)
- Services: Compute Engine, Cloud Functions, Firestore, Cloud Healthcare API.
- Key feature: FHIR-native APIs and BigQuery integration for analytics.
All three providers offer built-in encryption, DDoS protection, automatic scaling, and regional deployment options.
Video Communication APIs
Video calling is the cornerstone of telemedicine. The video stack must support HD quality, low latency, security, and reliability.
1. WebRTC
An open-source, peer-to-peer protocol stack for real-time video, audio, and data communication.
- Pros: Free, low-latency, browser-native.
- Limitations: Requires additional infrastructure for signaling, TURN/STUN servers.
2. Twilio Video
A programmable video SDK with robust APIs and HIPAA compliance support.
- Strengths: Prebuilt UIs, detailed analytics, recording, and bandwidth optimization.
- Best for: Enterprise-grade deployments.
3. Agora
Offers highly customizable SDKs with built-in network optimization, region-based streaming, and real-time engagement features.
- Benefits: Support for large-scale consultations, adaptive video quality, cross-platform SDKs.
Security Frameworks and Data Encryption Standards
Healthcare apps are high-value targets for cyber threats and must comply with international data security regulations.
Key security practices include:
- TLS 1.2+ for data in transit.
- AES-256 encryption for data at rest.
- HMAC and JWT tokens for session security.
- Role-Based Access Control (RBAC) and multi-factor authentication (MFA).
Frameworks such as OWASP ASVS, NIST Cybersecurity Framework, and ISO/IEC 27001 provide baseline security standards.
All integrations must meet:
- HIPAA (USA)
- GDPR (EU)
- PIPEDA (Canada)
- NABH & DISHA (India, where applicable)
Integration with Medical Devices and Wearables
As remote patient monitoring (RPM) expands, telemedicine apps increasingly interface with external medical hardware.
Typical integrations:
- Bluetooth-enabled devices: Blood pressure monitors, pulse oximeters, glucometers.
- Wearables: Apple Watch, Fitbit, Samsung Health devices for tracking heart rate, activity, and sleep.
- APIs: Apple HealthKit, Google Fit, and Bluetooth Low Energy (BLE) SDKs.
Standardizing data formats and ensuring real-time transmission with low latency are key to building effective integrations. All collected data must be encrypted and stored in compliance with local health data laws.
Database Choices and Management
The choice of database architecture affects app performance, compliance, and scalability.
1. SQL (Relational Databases)
- Options: PostgreSQL, MySQL, Microsoft SQL Server.
- Use cases: Structured data like user profiles, appointment records, prescriptions.
- Advantages: ACID compliance, strong consistency, data integrity.
2. NoSQL
- Options: MongoDB (document-based), Cassandra (wide-column), Firebase Realtime Database (mobile apps).
- Use cases: Storing chat logs, logs, real-time data, semi-structured EHRs.
- Advantages: High availability, scalability, faster for large unstructured datasets.
Hybrid architectures are common—using relational databases for core data and NoSQL for chat or analytics storage.
AI/ML Integration Possibilities
Artificial Intelligence and Machine Learning can augment diagnosis, triage, and operational efficiency.
Common integrations:
- NLP engines: For chatbot intake, summarizing consultations, or EHR search (e.g., Google’s Med-PaLM).
- Image classification models: For dermatology, radiology, or pathology applications.
- Predictive analytics: Patient risk scoring, medication adherence modeling.
ML workloads can be deployed using:
- TensorFlow Serving
- PyTorch on TorchServe
- SageMaker (AWS)
- Vertex AI (GCP)
All AI components must be interpretable, traceable, and approved by relevant medical boards for clinical use.
DevOps and CI/CD for Healthcare Apps
Continuous integration and deployment pipelines reduce downtime, enforce quality standards, and enable fast iteration.
Core DevOps tools:
- CI/CD: GitHub Actions, GitLab CI, Jenkins, CircleCI.
- Infrastructure as Code (IaC): Terraform, AWS CloudFormation.
- Monitoring: Prometheus, Grafana, New Relic, Datadog.
- Error tracking: Sentry, Rollbar.
Security-focused CI/CD practices such as static code analysis (SAST), dynamic application security testing (DAST), and runtime application self-protection (RASP) are highly recommended for healthcare.
A standard CI/CD pipeline includes:
- Code linting and formatting.
- Automated testing (unit, integration, and end-to-end).
- Deployment to staging and production environments.
- Backup and rollback procedures.
The technology stack for healthcare telemedicine app development must be resilient, compliant, and optimized for both performance and user experience. Choices will vary depending on the application’s scope—whether it’s an MVP targeting a single country or a global platform with AI and device integration.
Regulatory and Compliance Considerations
Regulatory compliance is non-negotiable in telemedicine application development. Healthcare apps collect, process, and transmit sensitive patient health information (PHI), which is heavily protected by law. Failing to comply with relevant regulations can result in legal consequences, financial penalties, and reputational damage.
This section outlines the key regulatory frameworks that telemedicine platforms must adhere to, including HIPAA, GDPR, FDA software classifications, and global data protection laws. It also examines practical security frameworks, consent mechanisms, and real-world compliance failures to illustrate the stakes involved.
HIPAA Compliance and Patient Data Privacy (U.S.)
The Health Insurance Portability and Accountability Act (HIPAA) establishes strict standards for handling PHI in the United States. Any entity that stores or transmits health data—whether healthcare providers or their software vendors—is subject to HIPAA rules.
Key HIPAA Provisions:
- Privacy Rule: Defines how PHI can be used or disclosed, requiring patient consent in most cases.
- Security Rule: Mandates administrative, technical, and physical safeguards for protecting ePHI (electronic PHI).
- Breach Notification Rule: Requires prompt notification to affected individuals and HHS in the event of data breaches.
Implementation Checklist:
- Data encryption in transit (TLS 1.2+) and at rest (AES-256).
- Access controls, including role-based permissions and MFA.
- Automatic session timeouts.
- Audit trails to track access and modification to health data.
- Business Associate Agreements (BAAs) with all third-party vendors handling PHI.
Enforcement:
The U.S. Department of Health and Human Services (HHS) can impose fines ranging from $100 to $50,000 per violation, with maximum annual penalties of $1.5 million per organization.
GDPR and Cross-Border Data Considerations (EU)
The General Data Protection Regulation (GDPR) is the most comprehensive data protection law in the European Union. While not healthcare-specific, it includes stringent requirements for storing, processing, and transferring any personal data, including health data.
Applicability:
- Applies to any organization handling EU residents’ data, regardless of the company’s location.
- Covers telemedicine platforms operating globally or with European users.
Core Requirements:
- Explicit consent: Patients must actively agree to data collection and processing.
- Right to access and erasure: Patients can request their data and demand its deletion.
- Data minimization: Only necessary data should be collected.
- Data localization: Data may need to be stored within the EU or transferred under appropriate safeguards (e.g., SCCs, DPF).
Security Mandates:
- Use of pseudonymization or anonymization where feasible.
- Breach reporting within 72 hours.
- Designation of a Data Protection Officer (DPO) in some cases.
GDPR noncompliance can lead to fines of up to €20 million or 4% of global revenue, whichever is higher.
FDA Regulations on Medical Software (U.S.)
The U.S. Food and Drug Administration (FDA) oversees software considered to be “Software as a Medical Device” (SaMD).
When is FDA approval required?
FDA regulation applies to telemedicine apps that:
- Diagnose, treat, or prevent medical conditions.
- Offer clinical decision support (CDS) without a qualified healthcare provider in the loop.
- Interface directly with medical devices or sensor data.
Examples:
- A simple appointment booking app is not regulated.
- An AI-based diagnostic app for skin lesions must go through FDA clearance.
Regulatory Pathways:
- 510(k) clearance: For devices that are “substantially equivalent” to existing FDA-approved products.
- De Novo classification: For novel, low-risk medical software.
- PMA (Pre-Market Approval): For high-risk, life-supporting software.
The Digital Health Software Precertification Program, although still evolving, is designed to streamline review for trusted developers.
Security Standards: ISO 27001 and HITRUST
While HIPAA and GDPR set the legal frameworks, ISO 27001 and HITRUST CSF provide structured implementation methodologies for achieving compliance.
ISO/IEC 27001
- International standard for information security management systems (ISMS).
- Focuses on risk management, access control, incident response, and data handling policies.
- Requires formal audits for certification.
HITRUST CSF
- A comprehensive security framework tailored for healthcare.
- Combines multiple standards (HIPAA, ISO, NIST, GDPR) into one certifiable program.
- Widely adopted by U.S. healthcare providers and insurers.
Certification in either framework helps reduce liability, increase trust with partners, and simplify vendor due diligence.
Consent Management and Audit Trails
Consent is a regulatory cornerstone—whether for data collection, sharing with third parties, or for diagnostic use.
Best Practices for Consent Management:
- Present users with granular, opt-in controls (e.g., share lab results with third parties).
- Clearly describe data use cases in privacy policies.
- Log time-stamped digital consent in secure, auditable formats.
Audit Trails:
A compliant telemedicine app must maintain logs of:
- Access to PHI (who, when, what was accessed).
- Modifications or deletions to health records.
- Login/logout events and failed login attempts.
Audit trails must be tamper-proof, encrypted, and regularly reviewed for anomalies. These are critical not only for compliance, but also for internal investigations in case of data breaches.
Case Studies: Compliance Failures and Lessons Learned
1. Anthem Data Breach (2015)
- Cause: Hackers accessed nearly 80 million records due to lack of encryption and poor internal access controls.
- Penalty: $16 million settlement with HHS—the largest HIPAA fine to date.
- Lesson: Encrypt all sensitive health data and implement multi-layered access controls.
2. Google Health / DeepMind & Royal Free NHS (UK, 2017)
- Issue: Google and a UK hospital shared 1.6 million patient records without proper patient consent under GDPR.
- Consequence: Public backlash, ICO (Information Commissioner’s Office) reprimand, and loss of trust.
- Lesson: Consent must be explicit and specific, especially when sharing data with technology providers.
3. Teladoc Lawsuit (2021)
- Allegation: Failure to adequately protect user data and misrepresentation of security posture to investors.
- Impact: SEC investigation, shareholder lawsuits.
- Lesson: Transparency in data handling and real security practices matter both legally and commercially.
Compliance in telemedicine is not just a legal requirement—it’s essential to protecting patient trust, avoiding reputational damage, and enabling sustainable business operations. Regulations like HIPAA, GDPR, and FDA software oversight impose high standards, while frameworks like ISO 27001 and HITRUST offer structured paths to implementation.
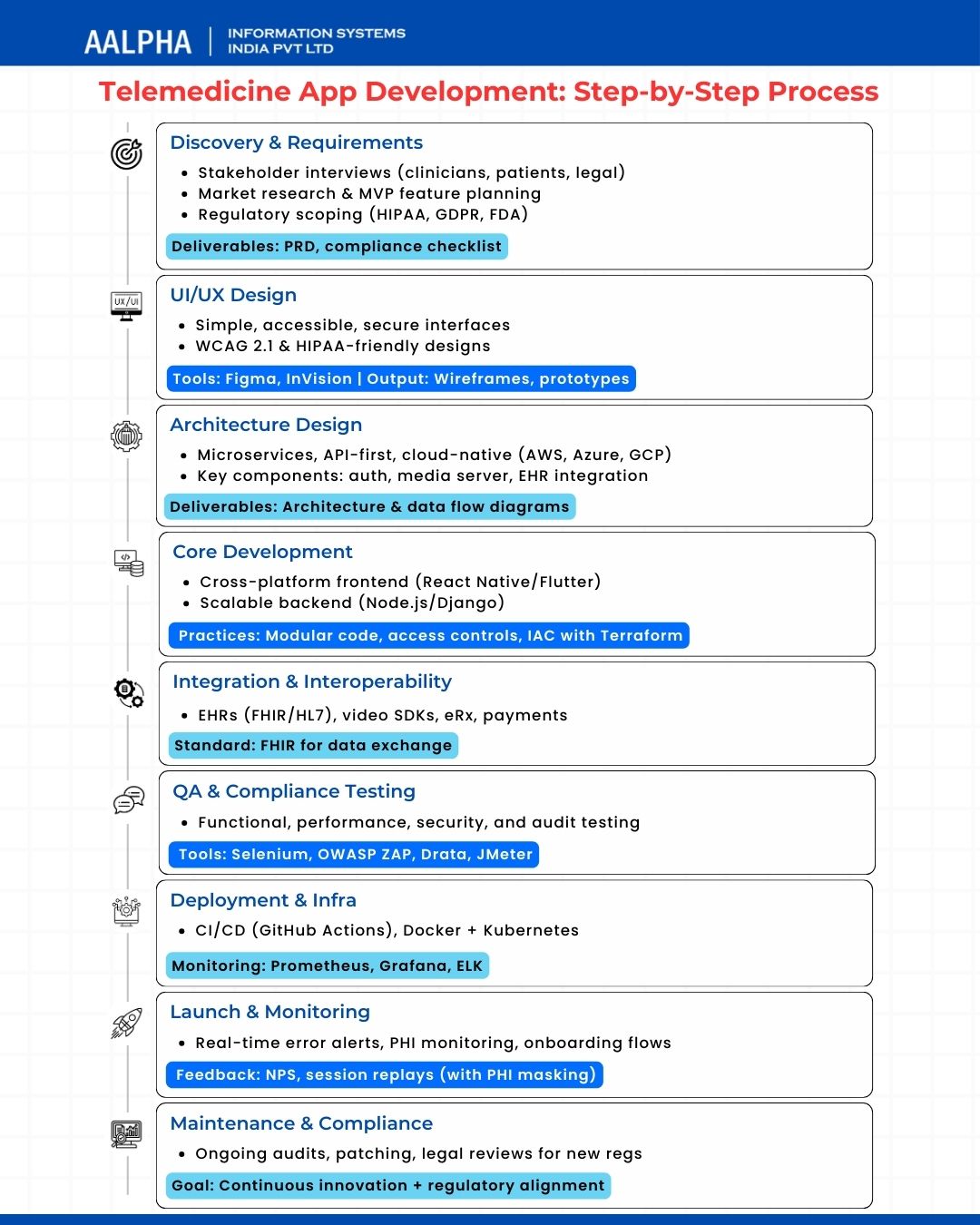
Step-by-Step Development Process for Telemedicine Apps
Building a secure, scalable, and regulation-compliant telemedicine application requires more than just coding. It involves strategic planning, user-centric design, rigorous backend architecture, testing under real-world conditions, and ongoing compliance oversight. Below is a detailed, phase-by-phase breakdown of the development process used by leading healthcare software firms and startups.
Step 1: Discovery and Requirement Analysis
Objective: Understand clinical, technical, regulatory, and user requirements before writing a single line of code.
Key Activities:
- Stakeholder interviews: Involve clinicians, patients, legal advisors, and IT staff.
- Market research: Analyze competitor features, pricing, and reviews.
- Feature prioritization: Use MoSCoW or RICE frameworks to categorize MVP vs. future enhancements.
- Regulatory scoping: Confirm applicable regulations (HIPAA, GDPR, FDA, etc.) and required audit certifications.
Deliverables:
- Product Requirements Document (PRD)
- Compliance checklist
- Initial risk analysis and threat modeling
Tip: Involve legal counsel early to avoid costly design changes during regulatory review.
Step 2: UI/UX Design and Prototyping
Objective: Design intuitive, accessible interfaces for patients and providers, with built-in compliance.
Design Priorities:
- Simplicity: Reduce cognitive load for patients (especially elderly or low-literacy users).
- Accessibility: WCAG 2.1 compliance for screen readers, keyboard navigation, contrast ratios.
- Security-first UI: Visual indicators of encrypted sessions, masked health data, session timeout alerts.
Tools:
- Figma, Adobe XD for high-fidelity mockups.
- Maze or InVision for interactive user testing.
Deliverables:
- Wireframes and clickable prototypes
- User journey maps
- Design system and reusable UI components
Example: Teladoc’s user flow uses conditional screens based on insurance type, automating eligibility checks during onboarding.
Step 3: Architecture Design
Objective: Define scalable backend architecture, service orchestration, data flow, and third-party integration logic.
Key Decisions:
- Microservices vs. Monolith: Microservices allow modular scaling (e.g., separate services for video, EHR access, billing).
- Cloud infrastructure: AWS HealthLake, Azure Health Data Services, or GCP Healthcare API.
- API-first approach: Enables mobile, web, and partner integrations using standardized REST/GraphQL APIs.
Architecture Components:
- Authentication service (OAuth 2.0 / OpenID Connect)
- Media server (WebRTC, Twilio)
- EMR/EHR gateway integration (FHIR APIs)
- Notification engine (SMS/email/reminders)
Deliverables:
- Architecture diagram
- Data flow diagrams (including PHI boundaries)
- Integration blueprint (for EHRs, pharmacy systems, lab portals)
Step 4: Core Development
Objective: Translate design and architecture into a fully functional MVP, with modular code and strict version control.
Frontend Stack:
- React Native / Flutter for cross-platform mobile development
- React.js / Angular for web portal interfaces
Backend Stack:
- Node.js / Django / Ruby on Rails for business logic
- PostgreSQL / MongoDB for data storage (based on relational or unstructured needs)
- Redis / Memcached for session and cache management
Dev Practices:
- Modular code structure with unit/integration tests
- Enforced access control and encryption at code level
- Environment isolation: dev, staging, production
Use Terraform or Pulumi for infrastructure as code, enabling replicable and auditable cloud environments.
Step 5: Integration and Interoperability
Objective: Ensure seamless connectivity to essential healthcare systems and services.
Must-Have Integrations:
- EHR/EMR: HL7, FHIR, or proprietary APIs from Epic, Cerner, or Allscripts.
- Pharmacy platforms: Surescripts, CVS, or local providers for e-prescriptions.
- Video calling: Twilio Video, Agora.io, or WebRTC-based custom SDKs.
- Payment: Stripe, PayPal Health, or insurance eligibility APIs.
FHIR (Fast Healthcare Interoperability Resources) is the emerging global standard for data exchange. Adoption of FHIR simplifies certification and international deployment.
Step 6: Quality Assurance and Compliance Testing
Objective: Validate functionality, security, and compliance through automated and manual testing.
Types of Testing:
- Functional: Validate all core features (registration, video call, eRx, billing).
- Performance: Simulate peak loads for video sessions and concurrent users.
- Security: Penetration testing, vulnerability scanning, API fuzzing.
- Compliance Audits: Simulate HIPAA and GDPR violations to test audit readiness.
Tools:
- Selenium, Appium for UI testing
- JMeter for load testing
- OWASP ZAP, Burp Suite for security validation
- Vanta, Drata, or Strike Graph for compliance readiness automation
Step 7: Deployment and Infrastructure
Objective: Deploy the application with automated pipelines, environment segregation, and high availability.
DevOps Pipeline:
- CI/CD tools: GitHub Actions, GitLab CI, Jenkins
- Containers: Docker with Kubernetes for orchestration
- Monitoring: Prometheus, Grafana, New Relic
- Logs: ELK stack (Elasticsearch, Logstash, Kibana)
Best Practices:
- Blue/green deployments for zero downtime.
- Automated rollback policies.
- WAF, CDN, and DDoS protection for traffic routing.
Consider AWS HealthLake, Azure API for FHIR, or Google Cloud Healthcare API for built-in compliance, scalability, and preconfigured healthcare modules.
Step 8: Launch and Post-Deployment Monitoring
Objective: Go live with a robust analytics layer, incident response protocols, and user onboarding workflows.
Post-Launch Checklist:
- Real-time error tracking (Sentry, Rollbar)
- PHI access alerts and anomaly detection
- User onboarding: in-app tutorials, live support, documentation
- Feedback loop: NPS, session replays (Hotjar/Smartlook with PHI masking), feature requests
A/B testing compliance features (e.g., two-step vs. biometric authentication) can help improve UX without compromising security.
Step 9: Maintenance, Upgrades, and Regulatory Updates
Objective: Keep the application secure, up-to-date, and in line with evolving health regulations.
Ongoing Tasks:
- Quarterly vulnerability scans and patching
- Annual third-party security audit
- Real-time monitoring for access and breach attempts
- Legal team reviews for regulatory changes (e.g., OCR updates to HIPAA, new EU laws)
Building a telemedicine platform is not a linear software project—it’s a continuous cycle of secure, compliant, and user-centric innovation. Following a structured development process reduces risks, accelerates time-to-market, and ensures alignment with clinical, operational, and legal expectations.
Telemedicine app development cost
The expense of telemedicine startup and the estimated time required to create a telemedicine app are often variable, depending on the team’s familiarity with related healthcare ventures, the team’s scale, and strict deadlines. However, you should keep in mind a few distinct features that typically need additional funding to ensure a high-quality outcome. A standard telemedicine application development would cost between $150,000 and $300,000+.
Breakdown of Cost Factors
1. Core Development
This includes UI/UX design, frontend and backend development, integration of video conferencing, chat, appointment scheduling, EHR/EMR systems, and payment gateways.
- MVP: $80,000–$150,000
- Full-featured product: $200,000–$400,000+
Factors influencing cost:
- Feature set complexity
- Number of supported platforms (iOS, Android, Web)
- Custom integrations with third-party systems (EHRs, labs, pharmacies)
2. Licensing and Infrastructure
Infrastructure costs are often underestimated. Compliance-grade cloud services and third-party APIs (for video, notifications, etc.) are recurring expenses.
Cost Item | Estimated Monthly Cost |
HIPAA-compliant cloud hosting (AWS/GCP/Azure) | $500–$5,000 |
Video conferencing API (e.g., Twilio, Agora) | $0.004–$0.01 per minute |
SMS/email notification services (e.g., SendGrid, Twilio SMS) | $50–$300+ |
Domain, SSL certificates, backups | $50–$200 |
3. Compliance and Legal
Ensuring data protection and regulatory adherence is not optional. It demands both legal and engineering investment.
- HIPAA/GDPR compliance audit: $10,000–$50,000
- Penetration testing and security assessments: $5,000–$30,000 annually
- Legal consultations (ongoing): $3,000–$10,000 annually
HIPAA-compliant solutions must ensure encrypted storage and transmission of PHI, secure access logging, audit trails, and breach notification protocols—all of which increase complexity and cost.
In-House vs Outsourcing Development Cost Comparison
Criteria | In-House Development | Outsourced Development (Nearshore/Offshore) |
Initial Cost | High (salaries, benefits, hiring overhead) | Lower (project-based or hourly) |
Time to Hire | 2–6 months | 1–3 weeks |
Expertise Availability | Limited to existing team | Wide access to healthcare-compliant talent |
Compliance Experience | Often lacking unless healthcare-specialized | Specialized vendors familiar with HIPAA/GDPR |
Estimated Budget | $250,000–$500,000+ | $80,000–$300,000 |
Example: A 5-person in-house team (PM, UI/UX, frontend, backend, QA) costs approximately $60,000/month in the U.S., versus $20,000–$35,000/month with a qualified outsourcing vendor from India or Eastern Europe.
Maintenance and Support Costs
Telemedicine apps are not static; they require constant updates for security, OS compatibility, and compliance changes. Maintenance usually accounts for 15–25% of the total development cost annually.
Typical Post-Launch Costs:
- Bug fixing and minor updates: $1,000–$5,000/month
- Server and API monitoring: $500–$2,000/month
- Security patches and compliance updates: $3,000–$10,000/year
- Feature enhancements: $10,000–$50,000+/year
Ensure Service Level Agreements (SLAs) include:
- Incident response time
- Recovery Time Objective (RTO) and Recovery Point Objective (RPO)
- Support availability (24/7 for clinical use cases)
ROI Expectations and Monetization Models
A well-executed telemedicine platform not only improves care access but also offers robust revenue potential.
Common Monetization Models:
- Pay-per-consultation: Patients pay a fee per video visit.
- Subscription: Monthly/annual fees for chronic care, behavioral health, or follow-up services.
- Enterprise SaaS: Licensing model for clinics, hospitals, or providers.
- Insurance reimbursement: Partnering with payers for covered virtual visits.
- White-label licensing: Sell your platform to other providers.
Example: Teladoc Health’s 2023 revenue exceeded $2.6 billion, driven by subscription plans and enterprise licensing.
ROI Timeline:
- MVP launch & feedback loop: 6–9 months
- Break-even point: 12–24 months (depending on scale and CAC/LTV ratio)
- Scalability: High, especially with asynchronous care models (e.g., AI symptom triage)
Final Budget Estimate (All-Inclusive)
Phase | Estimated Cost Range |
Discovery & Design | $10,000–$25,000 |
Development (MVP) | $80,000–$150,000 |
Compliance & Security | $20,000–$60,000 |
Hosting & Infrastructure (1 year) | $6,000–$30,000 |
Testing & QA | $10,000–$20,000 |
Maintenance (1st year) | $20,000–$50,000 |
Total (1st year estimate) | $150,000–$300,000+ |
Good: Cost to Build a Healthcare App
Future Trends and Innovations in Telemedicine Apps
Telemedicine has progressed far beyond simple video consultations. In the coming years, the integration of emerging technologies—particularly AI, IoT, 5G, blockchain, and immersive tools like AR/VR—will transform telehealth platforms into comprehensive, intelligent healthcare delivery systems. This section outlines key innovations shaping the future of telemedicine, with examples and practical implications for developers and healthcare organizations.
AI and Machine Learning in Diagnostics and Triage
Artificial intelligence is reshaping the diagnostic process within telemedicine platforms. By analyzing symptoms, patient history, and real-time biometric data, AI models assist in:
- Automated symptom triage: AI-driven tools (e.g., Infermedica, Ada Health) guide patients to appropriate care based on symptom input.
- Image and video analysis: AI in dermatology and radiology enables early detection of skin cancer, retinal disease, or musculoskeletal injuries during virtual visits.
- Voice analysis for mental health and neurological conditions: Natural language processing (NLP) and acoustic biomarkers can detect early signs of depression or Parkinson’s disease.
Example: Babylon Health’s AI triage assistant has conducted over 12 million consultations globally as of 2024, helping reduce GP workload while maintaining accuracy.
As healthcare systems face clinician shortages and growing caseloads, AI-enabled triage improves efficiency without compromising care quality.
Integration with IoT and Wearable Devices
The proliferation of medical-grade and consumer wearables is extending telemedicine beyond episodic care into continuous remote patient monitoring (RPM). Telemedicine apps are increasingly integrating with:
- Smartwatches (Apple Watch, Fitbit, Samsung Health): Monitor heart rate, oxygen saturation, and ECG.
- Connected devices (glucometers, blood pressure cuffs, smart thermometers): Enable chronic care management at home.
- IoMT (Internet of Medical Things): Hospital-at-home models now use in-home sensors for fall detection, medication adherence, and vital tracking.
By aggregating real-time biometric data, telemedicine platforms can offer early intervention, personalized alerts, and better post-discharge follow-up.
Market Insight: The global RPM market is projected to exceed $175 billion by 2027 (Fortune Business Insights, 2024), driven by IoT integration and chronic disease management needs.
Use of Blockchain for Data Security
Blockchain is emerging as a potential solution to healthcare’s persistent data security and interoperability challenges. While still nascent in production telehealth systems, its core capabilities offer future value:
- Immutable audit trails: Every transaction (access, edit, share) is recorded, ensuring transparency.
- Decentralized identity management: Patients can control access to their health records without relying on central databases.
- Smart contracts: Automate workflows like insurance claims, prescription validation, and cross-border provider licensing.
Example: Medicalchain and Solve.Care are leveraging blockchain to facilitate global telehealth consultations with secure, patient-controlled records.
Adoption will depend on regulatory alignment and scalability improvements, but blockchain’s architectural strengths align well with telehealth’s security and trust needs.
5G Impact on Telemedicine Performance
5G’s ultra-low latency and high bandwidth capabilities are transforming how telemedicine services are delivered, especially in areas previously constrained by connectivity issues.
Key Impacts:
- Seamless high-definition video consultations: Essential for fields like dermatology, ophthalmology, and neurology.
- Real-time remote surgery assistance: With sub-10ms latency, surgeons can guide procedures or operate robotic tools remotely.
- High-speed data transfer: Enables instantaneous upload of diagnostic imaging or large health datasets.
Industry Example: In 2024, China’s PLA General Hospital demonstrated a 5G-enabled remote orthopedic surgery with latency under 3ms—showcasing how real-time responsiveness enables high-stakes care remotely.
As 5G coverage expands, expect more complex, data-intensive telemedicine services to emerge across both rural and urban settings.
Virtual Reality (VR) and Augmented Reality (AR) in Telehealth
Immersive technologies like VR and AR are gaining traction in rehabilitation, behavioral therapy, and remote clinical training:
- VR-based therapy: Used for PTSD, phobias, chronic pain, and anxiety, allowing patients to undergo exposure therapy in safe, controlled environments.
- AR-assisted examinations: Providers can overlay real-time diagnostic instructions or anatomy visuals during patient interactions.
- Remote surgical collaboration: Surgeons in different locations can use AR tools to annotate and collaborate in real-time.
Example: XRHealth delivers FDA-registered VR-based teletherapy programs for cognitive rehabilitation and physical therapy, merging gaming mechanics with clinically validated protocols.
While integration into mainstream telemedicine apps is limited today, modular VR/AR toolkits are paving the way for hybrid care experiences.
Predictive Analytics and Personalized Medicine
One of the most promising frontiers in telemedicine lies in predictive healthcare—using machine learning to forecast patient risks and deliver individualized interventions.
Applications:
- Readmission risk scoring: Identifying post-discharge patients likely to require acute care within 30 days.
- Medication adherence prediction: Flagging patients at risk of non-compliance for chronic disease medications.
- Behavioral pattern analysis: Using app usage, wearable data, and contextual signals to identify deteriorating mental health or lifestyle risks.
Personalized recommendations based on genomic data, lifestyle, and clinical history can enable proactive, patient-centered care—not just episodic treatment.
Stat: According to McKinsey (2024), predictive analytics in healthcare could save over $300 billion annually in the U.S. through earlier interventions and optimized resource utilization.
Telemedicine is no longer confined to real-time video visits. The next generation of platforms will be intelligent, personalized, immersive, and continuously connected. For healthcare IT leaders and product teams, adopting these innovations requires early architectural foresight, secure integrations, and a deep understanding of clinical workflows.
Understanding these trends isn’t optional—it’s foundational for building scalable, future-proof telemedicine solutions in 2025 and beyond.
Conclusion
Telemedicine has evolved from a convenience into a strategic imperative for modern healthcare systems. As this guide has detailed, the opportunity for innovation lies not only in replicating in-person visits remotely but in fundamentally reimagining how healthcare is delivered—more accessible, data-driven, personalized, and continuous.
We’ve explored the global market trajectory, with telemedicine expected to exceed $530 billion by 2032, fueled by demographic shifts, digital transformation in healthcare, and regulatory momentum. Core features—like secure video consultations, EHR integration, e-prescriptions, and AI-assisted triage—form the foundation of a successful telemedicine platform. But emerging capabilities, such as IoT integration, predictive analytics, blockchain-based data security, and 5G performance enhancements, signal a move toward far more sophisticated, hybrid care models.
The technology stack must be carefully chosen to ensure scalability, compliance, and performance. Developers must address stringent regulatory frameworks (HIPAA, GDPR, FDA) while designing for interoperability, security, and long-term sustainability. Strategic trade-offs between in-house vs outsourced development, and between building custom features vs leveraging third-party APIs, must align with your product vision and budget.
Strategic Advice for CTOs and Product Leaders
For product leaders and CTOs, telemedicine app development in 2025 is no longer about just building and launching an MVP. It’s about:
- Designing for longitudinal care, not just episodic consultations
- Building architecture for extensibility, anticipating future AI, IoT, and wearable integrations
- Prioritizing compliance and trust, particularly in cross-border deployments
- Validating monetization models early—whether subscription, usage-based, or hybrid
- Partnering with clinicians early in the design process to ensure adoption and relevance
Final Thoughts
Investing in telemedicine app development is not simply a technical endeavor—it’s a commitment to reshaping healthcare delivery. Organizations that build robust, compliant, and patient-centric platforms today will be positioned as healthcare leaders tomorrow. For CTOs and healthcare innovators, the question is no longer whether to invest in telehealth—but how to do it right.
Want to Build a Secure, Scalable Telemedicine App?
Partner with Aalpha Information Systems—an experienced healthcare software development company trusted by global healthcare providers. From HIPAA-compliant architecture to real-time video integration and AI-powered features, we help you design, develop, and launch future-ready telemedicine platforms.
Contact us today to schedule a free consultation with our healthcare software experts.