A healthcare payment system is a technology-driven platform that enables healthcare providers, insurance companies, and patients to manage the financial side of medical services. It handles the end-to-end flow of payment-related activities—ranging from generating bills and verifying insurance coverage to processing transactions, tracking claims, and managing reimbursements. These systems are designed to integrate seamlessly with Electronic Health Records (EHRs), insurance portals, and payment gateways, ensuring that the financial component of healthcare delivery is accurate, secure, and compliant with relevant regulations such as HIPAA, PCI-DSS, and GDPR.
In practical terms, when a patient visits a hospital or clinic, the healthcare payment system is the backbone that supports every financial interaction. From validating insurance eligibility before treatment to generating transparent invoices and enabling quick settlement through multiple payment channels, it ensures that no part of the financial workflow is left vulnerable to delays, disputes, or errors.
TL;DR:
This guide explains how to develop a secure, compliant, and fully integrated healthcare payment system. It covers key payment models, stakeholder needs, essential features, compliance requirements (HIPAA, PCI-DSS, GDPR), technical architecture, and a step-by-step development process. It also details integration with EHR and insurance systems, cost considerations, common challenges, and future trends like AI reconciliation, blockchain claims, instant cross-border payments, and wearable-driven billing. Partnering with healthcare software development company–Aalpha Information Systems offers healthcare providers a proven team with expertise in healthcare and fintech, strong integration capabilities, and a focus on security, scalability, and long-term reliability.
Why Efficient Payment Processing Is Critical for Providers, Payers, and Patients
In today’s healthcare ecosystem, timely and accurate payment processing is not just an operational requirement—it’s a driver of financial stability, patient satisfaction, and overall trust in the healthcare system. For healthcare providers, efficient payment systems directly impact cash flow, allowing them to sustain operations, invest in better medical infrastructure, and pay staff without disruptions. Delays in claims reimbursement can cause liquidity issues, forcing hospitals and clinics to rely on credit lines or reduce operational capacity.
For insurance companies and payers, efficient payment processing minimizes administrative overhead, reduces fraudulent claims, and ensures faster turnaround times for claim settlements. It also improves relationships with provider networks, as timely payments encourage continued collaboration.
From the patient’s perspective, payment efficiency translates to greater transparency and convenience. Patients expect clear, itemized bills, easy-to-understand insurance coverage explanations, and multiple payment options—from traditional card payments to mobile wallets and digital banking. A slow or opaque payment process not only causes frustration but can also erode trust, potentially leading patients to switch providers.
Common Challenges in Current Healthcare Payment Workflows
Despite advances in digital health technology, many healthcare payment workflows remain fragmented and inefficient. One of the most persistent issues is claim denials due to incorrect coding, missing documentation, or mismatched patient information between healthcare providers and insurance databases. These errors create lengthy back-and-forth exchanges, delaying payments for weeks or even months.
Another challenge is lack of system interoperability. Many hospitals, clinics, and insurers use incompatible software systems, making it difficult to exchange billing and claims data in real time. This leads to duplicate entries, manual reconciliation work, and higher operational costs.
Security concerns are also significant. Healthcare payment systems handle sensitive personal and financial data, making them a target for cyberattacks. Without robust encryption, tokenization, and fraud detection mechanisms, both patients and providers face financial risks.
Additionally, healthcare payment workflows can be overly complex for patients, especially when multiple insurers, co-pay structures, and out-of-pocket expenses are involved. Patients often receive multiple bills for the same episode of care—one from the hospital, another from the physician group, and yet another from diagnostic labs—creating confusion and payment delays.
Ultimately, the need for a unified, secure, and intelligent healthcare payment system has never been greater. The right system can streamline billing, reduce administrative burdens, ensure compliance with regulations, and improve the financial experience for every stakeholder involved.
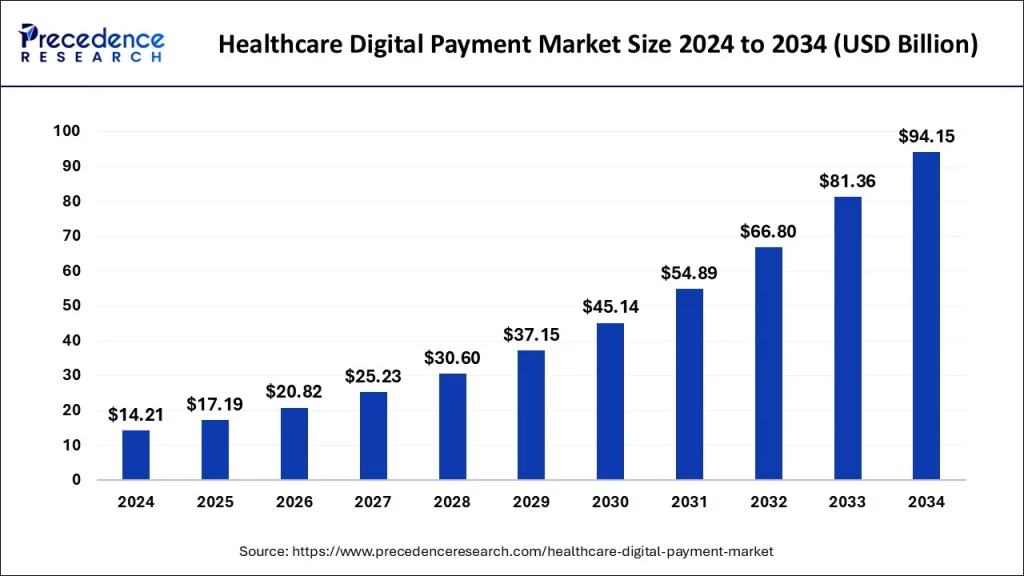
Did you know? The global digital payment market in healthcare was valued at USD 14.21 billion in 2024. It is projected to grow from USD 17.19 billion in 2025 to around USD 94.15 billion by 2034, registering a compound annual growth rate (CAGR) of 20.82% during the forecast period.
Image source: precedenceresearch
Overview of Healthcare Payment Models
Healthcare payment models define how providers are reimbursed for the services they deliver. Each model shapes the incentives, efficiency, and overall patient experience in healthcare delivery. In recent years, the industry has been shifting from purely volume-based reimbursement to models that reward quality, cost control, and patient outcomes. Below is an in-depth look at the most widely used models, along with emerging alternatives that are transforming the financial side of healthcare.
-
Fee-for-Service (FFS)
Definition and Process
Fee-for-Service (FFS) is the traditional healthcare payment model in which providers are reimbursed for each service performed. This includes consultations, diagnostic tests, procedures, and follow-up visits. Under this model, the more services delivered, the more revenue a provider generates. Payments are typically calculated based on standardized billing codes, such as CPT (Current Procedural Terminology) codes in the United States.
Advantages
- Clear and straightforward for both providers and insurers.
- Encourages comprehensive service delivery, ensuring that all possible interventions are available to the patient.
- Predictable billing for specific procedures.
Challenges
- Incentivizes volume over quality, potentially leading to overutilization of services.
- Increases healthcare costs without necessarily improving outcomes.
- Patients may face higher out-of-pocket expenses due to multiple billable items.
Example in Practice
A patient with knee pain visits a clinic and receives a consultation, X-ray, and physiotherapy recommendation. Each step—consultation, imaging, and therapy—is billed separately under FFS.
-
Value-Based Care (VBC)
Definition and Process
Value-Based Care shifts the focus from the quantity of services delivered to the quality and outcomes achieved. Providers are rewarded for meeting predefined performance metrics, such as improved patient recovery rates, reduced hospital readmissions, or better chronic disease management. Payments often come through shared savings programs or performance bonuses.
Advantages
- Encourages preventive care and long-term patient health improvement.
- Reduces unnecessary procedures and tests.
- Aligns provider incentives with patient outcomes rather than service volume.
Challenges
- Requires robust data analytics to measure performance accurately.
- Providers face financial risk if targets are not met.
- Complex to implement in multi-provider care environments.
Example in Practice
An accountable care organization (ACO) manages diabetic patients. If they reduce hospitalizations and improve HbA1c control rates while keeping costs down, they receive a portion of the cost savings from the payer.
-
Capitation and Bundled Payments
Capitation
Under capitation, providers receive a fixed amount per patient per month (PMPM), regardless of how many services the patient uses. This amount is agreed upon in advance between the provider and payer. The provider assumes full financial responsibility for patient care within the agreed scope.
Advantages
- Predictable revenue for providers.
- Incentivizes cost control and preventive care.
- Reduces billing complexity.
Challenges
- Risk of under-treatment if providers limit services to stay within budget.
- Difficult to manage in populations with unpredictable healthcare needs.
Bundled Payments
Bundled payments involve a single, pre-determined payment for all services related to a specific treatment or condition over a defined period. For example, a bundled payment for joint replacement surgery would cover pre-surgery evaluations, the surgery itself, post-operative care, and rehabilitation.
Advantages
- Promotes care coordination among providers.
- Encourages efficiency in managing episodes of care.
- Offers cost predictability for payers and patients.
Challenges
- Requires accurate cost forecasting and risk sharing agreements.
- Complicated for multi-condition patients who need overlapping services.
-
Direct-to-Consumer (DTC) Payments
Definition and Process
Direct-to-Consumer payments occur when patients pay providers directly without involving insurance companies. This can be through out-of-pocket payments, health savings accounts (HSAs), or direct primary care arrangements. It is common in elective procedures, urgent care visits, and telemedicine services not covered by insurance.
Advantages
- Eliminates administrative complexity tied to insurance billing.
- Gives providers faster access to revenue without waiting for claims processing.
- Offers patients more control over healthcare choices.
Challenges
- May limit access for patients who cannot afford upfront payments.
- Less predictable revenue compared to insured services.
Example in Practice
A patient books a telemedicine consultation with a dermatologist and pays a flat fee via an online payment gateway without filing an insurance claim.
Emerging Models: Subscription-Based Healthcare Payments
Definition and Process
Subscription-based healthcare, often seen in direct primary care (DPC) or concierge medicine, involves patients paying a recurring monthly or annual fee for unlimited or enhanced access to healthcare services. This model removes per-service billing entirely, creating a more predictable and relationship-focused provider-patient dynamic.
Advantages
- Predictable revenue stream for providers.
- Encourages continuous, preventive care.
- Enhances patient experience with longer consultations and personalized attention.
Challenges
- May not be financially viable for patients with infrequent healthcare needs.
- Limited scalability for large health systems without significant restructuring.
Example in Practice
A patient pays $75 per month for a DPC plan, which covers unlimited primary care visits, basic lab tests, and 24/7 virtual consultations.
The healthcare industry is moving toward hybrid payment models that combine elements of the above approaches to balance financial stability with quality care incentives. For example, a health system may use a base capitation payment structure supplemented with performance bonuses tied to value-based care metrics. Understanding these models is crucial when designing a healthcare payment system, as the platform must be flexible enough to support multiple reimbursement frameworks while maintaining compliance and operational efficiency.
Key Stakeholders in Healthcare Payments
A healthcare payment system exists at the intersection of multiple stakeholders, each with unique priorities, workflows, and challenges. Understanding their roles is essential to building a payment platform that works seamlessly across the entire ecosystem. While their objectives may differ, all share a common goal: ensuring that medical services are compensated fairly, promptly, and transparently.
-
Hospitals, Clinics, and Private Practices
Healthcare providers are at the center of payment systems because they deliver the services that trigger financial transactions. This group includes large hospital networks, specialized clinics, and small private practices. Their needs often focus on streamlining billing processes, reducing claim denials, and improving revenue cycle management.
For example, a busy orthopedic clinic might struggle with delayed insurance reimbursements that disrupt cash flow. Could an automated payment system integrated with the clinic’s EHR ensure faster claims submission and fewer errors? Absolutely—it could validate patient insurance in real time, auto-populate billing codes, and flag incomplete documentation before claims are sent.
In addition to revenue collection, providers must also maintain compliance with regulations like HIPAA and PCI-DSS. A well-designed system should therefore support secure payment processing, accurate patient invoicing, and transparent financial reporting, without overburdening administrative staff.
-
Insurance Companies and Third-Party Payers
Insurance companies and other third-party payers, such as government programs and employer-sponsored health plans, play a critical role in healthcare payments by funding or reimbursing a significant portion of care costs. Their priorities include reducing fraudulent claims, improving claim adjudication speed, and ensuring policy compliance.
Consider a scenario where a patient receives surgery at a hospital. How can the insurer quickly confirm coverage, calculate the exact reimbursement amount, and issue payment without weeks of back-and-forth? The right payment system integrates directly with insurance databases, verifying benefits instantly and generating clear breakdowns for both providers and patients.
These systems also help payers analyze claim trends, identify high-cost care patterns, and develop value-based contracts with providers. By automating eligibility checks and using AI to detect anomalies, insurers can not only save money but also improve provider satisfaction.
-
Patients and Caregivers
Patients and their caregivers are the ultimate beneficiaries of healthcare services, but they often face the most frustration when payment processes are unclear or delayed. They expect transparent billing, flexible payment options, and easy-to-access statements.
Imagine receiving three separate bills for the same hospital stay—from the facility, the attending physician, and the lab. Wouldn’t it be easier if all charges were consolidated into a single statement, with clear explanations of insurance coverage and out-of-pocket costs? Modern healthcare payment systems can provide exactly that, along with online portals or mobile apps that let patients pay instantly, set up installment plans, and track their payment history.
From a patient’s perspective, speed and clarity are key. If they can verify what’s covered by insurance before treatment, understand why they’re being billed a certain amount, and pay through their preferred method—whether that’s a credit card, bank transfer, or mobile wallet—they’re far more likely to have a positive experience.
-
Regulatory Authorities and Payment Processors
Regulatory bodies ensure that healthcare payment systems comply with data privacy, security, and financial transaction laws. In the U.S., this includes HIPAA for patient data security and PCI-DSS for payment card transactions. In Europe, GDPR governs how personal data is stored and processed.
But how do these rules translate into system design? Compliance means using encryption to secure sensitive information, maintaining audit trails for all transactions, and implementing multi-factor authentication for system access. Failure to meet these standards can result in heavy fines and reputational damage.
Payment processors, on the other hand, are the behind-the-scenes infrastructure that moves money between patients, insurers, and providers. They must ensure fast, secure, and reliable transactions—whether through traditional banks, fintech solutions, or integrated healthcare payment gateways. The choice of payment processor can significantly impact transaction fees, settlement times, and fraud protection capabilities.
Healthcare payments involve a tightly interconnected network: providers delivering care, insurers funding it, patients paying their share, and regulators ensuring everyone follows the rules. A truly effective healthcare payment system must cater to all these stakeholders, bridging their needs with technology that makes payments faster, safer, and easier for everyone involved.
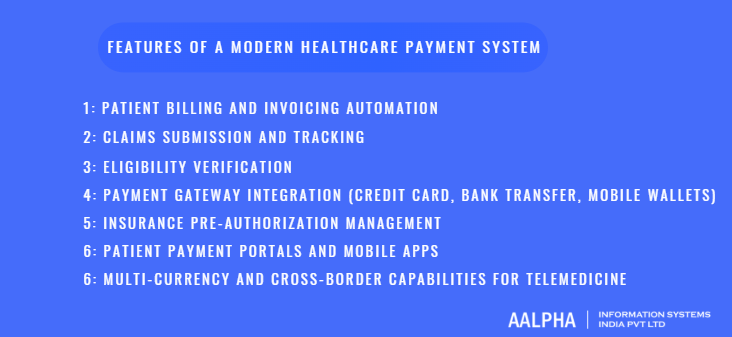
Core Features of a Modern Healthcare Payment System
A modern healthcare payment system is more than just a billing tool—it’s a fully integrated financial engine that supports the needs of providers, patients, insurers, and regulators simultaneously. To be effective, it must automate repetitive tasks, reduce human error, comply with industry regulations, and deliver a seamless payment experience. Below is a detailed breakdown of the core features every advanced healthcare payment system should include, along with real-world examples of how they improve operational efficiency and patient satisfaction.
-
Patient Billing and Invoicing Automation
Manual billing processes are slow, error-prone, and resource-intensive. An automated billing and invoicing module generates accurate bills based on patient records, treatment codes, and insurance coverage—without requiring manual data entry for each transaction.
Imagine a patient undergoing a series of physiotherapy sessions. Instead of manually creating individual invoices for each visit, the system can automatically generate recurring bills, apply pre-set discounts, and send them via email or patient portals.
Key capabilities include:
- Auto-generation of itemized bills based on CPT or ICD codes.
- Batch billing for repeat treatments or follow-up care.
- Integration with EHR to pull treatment data instantly.
- Automated reminders for overdue invoices.
Automation not only speeds up billing cycles but also reduces disputes, as itemized statements help patients understand exactly what they’re paying for.
-
Claims Submission and Tracking
In a typical healthcare setting, delays in claims submission and errors in coding can cost providers significant revenue. A modern payment system integrates directly with insurance clearinghouses, allowing claims to be submitted electronically and tracked in real time.
For instance, if a patient’s surgery is coded incorrectly, the system can flag the error before submission, preventing a claim denial that could take weeks to resolve.
Key capabilities include:
- Electronic claim submission (EDI integration).
- Automated claim status updates.
- Error detection and correction before submission.
- Historical claim tracking for analytics.
By giving providers visibility into where a claim is in the approval process, the system eliminates guesswork and improves cash flow predictability.
-
Eligibility Verification
Verifying a patient’s insurance eligibility before treatment is critical to preventing billing disputes. A robust payment system can perform real-time eligibility checks, confirming coverage details, deductibles, and co-pay requirements before care is delivered.
Consider a scenario where a patient books an MRI appointment. Wouldn’t it save time if the clinic could instantly verify that the scan is covered and inform the patient of any out-of-pocket costs? Eligibility verification does exactly that.
Key capabilities include:
- Real-time integration with insurance provider databases.
- Verification of coverage limits and exclusions.
- Automatic updates when patient benefits change.
- Integration with appointment scheduling systems.
This feature not only reduces claim rejections but also builds patient trust by setting clear financial expectations upfront.
-
Payment Gateway Integration (Credit Card, Bank Transfer, Mobile Wallets)
Patients today expect the same level of convenience in healthcare payments as they do in retail or e-commerce. A modern payment system must support multiple payment methods—including credit/debit cards, ACH bank transfers, mobile wallets (e.g., Apple Pay, Google Pay), and even emerging fintech options like Buy Now, Pay Later (BNPL).
If a patient receives a digital invoice after a telehealth consultation, why should they have to visit the clinic to pay? With a secure payment gateway integrated into the system, they can settle their bill instantly through their preferred channel.
Key capabilities include:
- PCI-DSS-compliant card processing.
- Tokenization for secure storage of payment details.
- Automated payment reconciliation with the provider’s accounting system.
- Support for one-time and recurring payments.
By offering flexible payment options, providers can reduce overdue accounts and improve overall patient satisfaction.
-
Insurance Pre-Authorization Management
Many high-cost procedures require insurance pre-authorization before they can be performed. Handling this manually can lead to delays in care, frustrated patients, and administrative bottlenecks. A modern payment system automates pre-authorization requests, tracks approvals, and alerts staff when follow-ups are needed.
For example, a cardiologist scheduling a stent procedure can trigger an automated pre-authorization request from within the system, complete with all required documentation. This not only speeds up approval but also ensures compliance with payer requirements.
Key capabilities include:
- Auto-generation of pre-authorization requests.
- Document uploads for supporting medical evidence.
- Real-time status tracking of authorization requests.
- Integration with clinical workflow systems.
This automation ensures patients receive timely care while providers avoid revenue losses due to missing or delayed approvals.
-
Patient Payment Portals and Mobile Apps
In an era where self-service is the norm, a patient-facing portal or mobile app is essential. These tools allow patients to view bills, make payments, set up payment plans, download receipts, and communicate with billing staff—all without calling the clinic.
If a patient wants to pay for a lab test at midnight or split a bill into installments, the patient portal makes it possible. The result is higher payment completion rates and fewer overdue accounts.
Key capabilities include:
- Secure login with MFA for patient accounts.
- Bill viewing and payment history.
- Customizable payment plans with automatic reminders.
- Integration with telehealth platforms for unified billing.
This level of accessibility also improves transparency, reducing patient anxiety over surprise bills.
-
Multi-Currency and Cross-Border Capabilities for Telemedicine
As telemedicine expands globally, providers increasingly serve patients across borders. A modern healthcare payment system must handle multi-currency transactions, cross-border compliance, and fluctuating exchange rates.
Imagine a U.S.-based telehealth provider treating a patient in Europe. The system should be able to issue an invoice in euros, process payment through a local gateway, and still reconcile it in the provider’s base currency.
Key capabilities include:
- Support for multiple currencies and real-time exchange rate updates.
- Compliance with regional financial regulations.
- Integration with international payment processors.
- Automatic currency conversion reporting.
By accommodating global patients, providers can expand their reach without creating financial friction.
A truly modern healthcare payment system is modular yet integrated—each feature works independently but also connects with other modules to create a seamless financial workflow. From automated billing to real-time insurance checks and cross-border payment handling, these features enable providers to focus on patient care rather than administrative burdens.
When all of these capabilities are combined in a single platform, the result is faster payments, fewer errors, higher patient satisfaction, and better financial stability for healthcare organizations of all sizes.
Compliance and Security Requirements
Compliance and security are not optional add-ons for healthcare payment systems—they are foundational requirements. Because these platforms handle both protected health information (PHI) and sensitive financial data, they must be designed to meet the highest standards of privacy, integrity, and availability. Regulatory frameworks vary by region, but the underlying goal is the same: protect patient trust and ensure data is handled ethically and securely.
This section examines the major compliance obligations and security measures that every healthcare payment system must address, along with practical examples of how they are implemented.
-
HIPAA (U.S.) Compliance for Patient Financial Data
In the United States, the Health Insurance Portability and Accountability Act (HIPAA) governs the privacy and security of protected health information. While HIPAA is often associated with clinical data, it also covers patient financial records if they are linked to health services. This means a billing statement that includes treatment details is subject to the same protections as a patient’s medical chart.
Core HIPAA Requirements for Payment Systems:
- Privacy Rule: Ensure that patient financial data tied to medical care is only shared with authorized individuals or entities.
- Security Rule: Implement safeguards for electronic PHI (ePHI), including encryption, secure transmission protocols, and access controls.
- Breach Notification Rule: Establish procedures to notify affected parties and authorities in the event of a data breach.
Example in Practice:
If a hospital’s payment portal displays a patient’s outstanding balance for a surgery along with the diagnosis code, that information must be encrypted in transit (using TLS) and at rest (using AES-256 encryption). Access should be limited to authorized staff with role-based permissions.
Key HIPAA Implementation Measures:
- Use of secure APIs for EHR and billing system integration.
- Detailed audit trails logging who accessed financial records and when.
- Regular HIPAA compliance audits and staff training.
-
PCI-DSS Standards for Secure Payment Transactions
While HIPAA covers the healthcare aspect, Payment Card Industry Data Security Standard (PCI-DSS) governs credit and debit card transactions. Any healthcare payment system that processes card payments—whether through a POS terminal in a hospital lobby or an online patient portal—must comply with PCI-DSS.
Core PCI-DSS Requirements:
- Do not store full card numbers, CVVs, or magnetic stripe data after authorization.
- Use encryption and tokenization to protect cardholder data.
- Maintain secure networks with firewalls and intrusion detection systems.
- Conduct regular vulnerability scans and penetration testing.
Example in Practice:
If a patient pays for a telehealth consultation with a credit card, the payment gateway should tokenize the card details immediately, replacing sensitive information with a secure token. The provider’s system never stores the raw card number, reducing risk in case of a data breach.
Best Practices for PCI-DSS Compliance in Healthcare:
- Partner with PCI-compliant payment processors.
- Segment payment systems from clinical networks to reduce attack surface.
- Provide secure payment links in digital invoices to avoid email-based fraud.
-
GDPR (Europe) for Data Privacy in Cross-Border Healthcare Services
For healthcare providers serving patients in the European Union, the General Data Protection Regulation (GDPR) sets strict rules on data privacy and cross-border transfers. Even if a provider is based outside the EU, they must comply with GDPR when processing the personal data of EU residents.
Key GDPR Principles for Payment Systems:
- Lawful Basis for Processing: Providers must have a valid reason for collecting and processing patient payment data, typically “performance of a contract” or “legitimate interest.”
- Data Minimization: Collect only the information necessary for payment processing.
- Right to Access and Erasure: Patients can request access to their payment records or have them deleted.
- Cross-Border Transfer Safeguards: Data sent outside the EU must be protected by mechanisms such as Standard Contractual Clauses (SCCs).
Example in Practice:
A London-based telemedicine provider offering consultations to patients in Germany must ensure that payment data processed on U.S.-based servers is protected under GDPR-approved transfer agreements.
Best Practices for GDPR Compliance:
- Maintain transparent privacy policies explaining how payment data is used.
- Offer patients clear consent options for storing payment information.
- Implement pseudonymization to reduce the risk of data exposure.
-
Anti-Fraud Mechanisms and Secure Authentication
Fraud in healthcare payments is a costly and persistent threat, ranging from stolen payment credentials to fraudulent claims. A modern payment system must proactively detect and prevent these activities through a combination of AI-driven monitoring and secure authentication methods.
Key Anti-Fraud Measures:
- AI-Based Fraud Detection: Machine learning algorithms can flag unusual billing patterns, such as a sudden spike in high-cost claims from a single provider.
- Transaction Monitoring: Real-time analysis of payment activity to spot anomalies, such as mismatched patient and payer locations.
- IP Whitelisting and Geofencing: Limiting access to payment systems from approved locations only.
Secure Authentication Methods:
- Multi-Factor Authentication (MFA): Require users to confirm their identity using a combination of passwords, one-time codes, or biometrics.
- Biometric Login: Use fingerprint or facial recognition for patient portal access, especially for high-value transactions.
- Role-Based Access Control (RBAC): Limit sensitive actions (e.g., refund approvals) to authorized staff only.
Example in Practice:
If a patient logs into their payment portal from an unfamiliar device in another country, the system can require MFA verification before allowing bill payments or access to financial records.
Integrating Compliance into System Design
The most secure healthcare payment systems are built with compliance by design, not as an afterthought. This means:
- Embedding encryption, tokenization, and access controls into the architecture from day one.
- Choosing cloud hosting providers with HIPAA, PCI-DSS, and GDPR certifications.
- Conducting regular third-party audits and penetration tests.
- Training all staff involved in billing, claims, and payment processing on security best practices.
Compliance and security requirements are not simply regulatory hurdles—they are trust-building mechanisms. When patients, providers, and insurers know their data is handled with care, they are more likely to adopt digital payment solutions confidently. A payment system that meets HIPAA, PCI-DSS, and GDPR standards while using advanced anti-fraud measures doesn’t just protect against legal risks—it strengthens the entire healthcare payment ecosystem.
Technical Architecture of a Healthcare Payment System
A well-designed healthcare payment system must balance security, scalability, and interoperability while delivering a seamless user experience. Its architecture is not just about choosing the right technology—it’s about creating a robust ecosystem that integrates clinical, financial, and regulatory workflows into a single platform.
The following breakdown examines the core components of an enterprise-grade healthcare payment system, from patient-facing interfaces to AI-powered fraud detection.
-
Front-End Patient and Provider Interfaces
The front end is the user-facing layer where patients, providers, and billing staff interact with the system. It must be intuitive, responsive, and secure—capable of delivering real-time updates on transactions, claims, and payment status.
Patient Interface Features:
- Responsive Web Portals and Mobile Apps: Patients should be able to view bills, make payments, set up recurring installments, and track claim statuses from any device.
- Multi-Channel Access: Support for web, mobile, and even kiosk interfaces in hospitals or clinics.
- Payment History and Receipts: Easily accessible transaction logs for patient reference.
- Language and Accessibility Options: Localization for multiple languages, screen reader support, and ADA-compliant design.
Provider Interface Features:
- Dashboard View of Outstanding Payments: Consolidated reporting for pending invoices, denied claims, and payment trends.
- Claim Submission and Tracking Tools: Allow providers to generate, review, and send claims electronically.
- Authorization and Eligibility Tools: Real-time insurance checks and pre-authorization requests.
- Role-Based Access Control (RBAC): Ensures that front-office staff, billing teams, and administrators have tailored access.
Example in Practice:
A patient logs in to their portal to pay for an MRI, while the provider dashboard shows the payment in real time and auto-updates revenue cycle reports. This eliminates manual reconciliations and improves transparency for both parties.
-
Back-End Billing Engine and Payment Gateway Connectors
The back end is the operational core, processing all transactions, claim submissions, and reconciliations. It must be highly reliable, fault-tolerant, and compliant with healthcare and payment regulations.
Billing Engine Functions:
- Automated Bill Generation: Pulls data from EHR systems to create itemized invoices.
- Claims Processing Pipeline: Formats, validates, and sends claims to insurers electronically.
- Adjustment and Reconciliation Logic: Handles partial payments, insurance adjustments, and write-offs.
- Real-Time Revenue Cycle Tracking: Tracks payment flow from service delivery to final settlement.
Payment Gateway Connectors:
- Multi-Provider Integration: Supports multiple payment processors (Stripe, PayPal, Authorize.net, Square, healthcare-specific gateways).
- Tokenization and Encryption: Ensures PCI-DSS compliance by securing cardholder data.
- Multi-Currency Support: Enables cross-border transactions for telehealth providers.
- Settlement and Refund Automation: Processes refunds directly from the dashboard with audit tracking.
Example in Practice:
If a telehealth consultation is billed in euros but paid via a U.S. card, the back end automatically converts the currency, processes payment through a PCI-DSS-compliant gateway, and reconciles the amount in the provider’s base currency.
-
API Integrations with EHR/EMR Systems
A healthcare payment system is most effective when fully integrated with Electronic Health Record (EHR) and Electronic Medical Record (EMR) systems. APIs (Application Programming Interfaces) facilitate seamless data exchange, reducing duplicate entries and administrative overhead.
Core API Integration Use Cases:
- Automatic Billing Data Retrieval: Pulls CPT/ICD codes and treatment details directly from EHR to generate invoices.
- Insurance Verification: Real-time eligibility checks through payer APIs.
- Claim Status Updates: Syncs with payer systems to reflect approval, rejection, or pending status.
- Payment Posting to EHR: Updates patient financial records in the EHR without manual input.
Example in Practice:
When a patient is discharged, the EHR sends all encounter data to the payment system via API. The payment system auto-generates the bill, submits insurance claims, and syncs the payment status back to the EHR—completely eliminating manual data transfer.
-
Cloud Hosting vs. On-Premises Deployment
The choice between cloud-based and on-premises deployment affects scalability, compliance, and maintenance costs.
Cloud Hosting Advantages:
- Scalability: Easily handle increased transaction loads during peak times.
- Lower Upfront Costs: No need for in-house server infrastructure.
- Disaster Recovery: Built-in redundancy and failover capabilities.
- Automatic Updates: Security patches and feature upgrades are handled by the provider.
Cloud Hosting Considerations:
- Must select HIPAA, GDPR, and PCI-DSS-compliant cloud vendors (AWS, Azure, GCP).
- Data residency laws may require local hosting for certain patient records.
On-Premises Advantages:
- Full Control: Direct access to hardware and security configurations.
- Local Compliance Needs: Easier to meet data residency requirements in certain jurisdictions.
On-Premises Considerations:
- Higher capital and operational expenses.
- Requires in-house IT team for maintenance, backups, and upgrades.
Hybrid Approach:
Some providers use a hybrid architecture—critical patient data stored on-premises while payment processing occurs in the cloud for scalability.
-
Use of AI for Fraud Detection and Predictive Payment Analytics
AI plays a growing role in securing healthcare payment systems and optimizing revenue cycles.
Fraud Detection Applications:
- Pattern Recognition: Machine learning models can detect anomalies in billing, such as duplicate claims or abnormally high charges for specific procedures.
- Transaction Risk Scoring: Each payment is assigned a fraud likelihood score in real time.
- Behavioral Analytics: Identifies suspicious login or payment activity by comparing against typical user behavior.
Predictive Payment Analytics Applications:
- Cash Flow Forecasting: Predicts incoming revenue based on historical claim approval rates and payment patterns.
- Patient Payment Likelihood: Identifies which patients are most likely to default on bills, enabling proactive outreach.
- Claim Denial Prediction: Uses past rejection patterns to flag high-risk claims before submission.
Example in Practice:
If AI detects that a provider’s claim approval rate for a specific procedure drops significantly, it can alert billing staff to investigate coding errors or policy changes before more claims are denied.
An optimal technical architecture for a healthcare payment system connects intuitive front ends, a powerful back-end billing engine, EHR-integrated APIs, and secure hosting—all reinforced by AI-powered analytics and fraud prevention.
When these elements are designed to work in harmony, the result is a system that:
- Processes payments faster.
- Reduces claim denials.
- Improves patient and provider satisfaction.
- Meets compliance requirements without adding administrative burden.
A well-architected system isn’t just a payment tool—it’s a strategic asset that strengthens financial stability, operational efficiency, and trust across the healthcare ecosystem.
Developing a Healthcare Payment System : Step-by-Step Guide
Building a healthcare payment system is a complex but highly structured process. Every phase—from requirement gathering to post-launch optimization—needs to be executed with precision to ensure the platform is secure, compliant, and efficient. The goal is to create a system that not only processes payments but also streamlines workflows, integrates with clinical systems, and enhances the financial experience for both providers and patients.
-
Requirement Gathering and Stakeholder Analysis
The first step is understanding exactly what the system must do. This involves mapping out who will use it, what challenges they face, and what success will look like. The process should start with in-depth discussions with hospitals, clinics, insurance companies, billing staff, patients, and regulators to ensure that all voices are heard. By identifying specific pain points—such as frequent claim denials, payment delays, or lack of patient transparency—you can design a solution that addresses real needs rather than assumed ones.
During this phase, the development team should document both functional requirements (the actual tasks the system must perform) and non-functional requirements (speed, scalability, uptime). Some of the most important activities here include:
- Stakeholder Identification: List every category of user—providers, payers, patients, regulatory bodies, and technical partners like payment processors.
- Workflow Mapping: Document the current billing, claim submission, and payment processes, including where breakdowns occur.
- Volume Assessment: Estimate daily, weekly, and monthly transactions to determine system load requirements.
- Integration Needs: Identify essential third-party integrations, such as EHRs, insurance databases, or accounting software.
Example: A multi-specialty clinic may report that its biggest issue is the time lag between patient discharge and claim submission. Knowing this, you can prioritize automated claim generation in the early development stages.
-
Regulatory Compliance Planning
In healthcare payments, compliance isn’t optional—it’s a foundational design principle. Building with compliance in mind from the start prevents costly reengineering later and ensures the system can be trusted by providers, patients, and payers alike. Compliance planning begins with a thorough review of applicable regulations based on the regions where the system will operate.
This step involves defining exactly how data will be protected and where it will be stored. For instance, in the U.S., HIPAA requires encryption for PHI, while PCI-DSS governs card payment security, and GDPR dictates strict rules for EU patient data. Key planning activities include:
- Data Flow Mapping: Identify where patient and payment data is collected, stored, transmitted, and accessed.
- Security Controls: Plan for encryption (AES-256 for stored data, TLS 1.2+ for transmission), tokenization, and access controls.
- Compliance Auditing: Schedule periodic security and compliance reviews after launch.
- Certified Vendors: Choose cloud or payment providers with HIPAA, PCI-DSS, and GDPR certifications.
Example: A telehealth provider serving both U.S. and EU patients must plan for GDPR-approved data transfer mechanisms while ensuring HIPAA encryption standards. This dual-compliance requirement affects everything from hosting provider selection to API security design.
-
System Design and Architecture Blueprint
Once requirements and compliance parameters are clear, it’s time to design the technical blueprint. The architecture must be modular, allowing different parts—like billing, claims, or payment gateways—to be updated independently without disrupting the whole system. Scalability and fault tolerance are critical, especially for high-volume providers or those expanding internationally.
In designing the architecture, pay attention to:
- Front-End Interfaces: Patient portals, provider dashboards, mobile apps, and in-clinic kiosks for bill payment.
- Back-End Billing Engine: Automated invoice generation, claim submission workflows, and reconciliation logic.
- API Integration Layer: Secure connections to EHRs, insurance systems, and payment processors.
- Security Layer: Built-in encryption, intrusion detection, and multi-factor authentication.
Example: A hybrid architecture may store sensitive patient data on-premises for compliance reasons but process payments via a HIPAA-compliant cloud platform for scalability and performance.
-
Feature Development and API Integrations
With the blueprint in place, development begins. Using an agile approach ensures that features are delivered in iterations, tested, and refined based on real feedback. The core features to prioritize include:
- Automated Patient Billing: Generate itemized invoices linked directly to clinical records.
- Claims Submission and Tracking: Integrated with clearinghouses for real-time status updates.
- Eligibility Verification: Instant insurance checks before treatment is provided.
- Payment Gateway Integration: Support for credit/debit cards, ACH, mobile wallets, and BNPL options.
- Insurance Pre-Authorization: Automated workflows for high-cost procedures.
- Multi-Currency and Cross-Border Support: Essential for telehealth providers serving global patients.
Example: A physiotherapy clinic could integrate with its EHR to auto-fill billing codes after each session, submit claims electronically, and allow patients to pay outstanding balances via mobile app—all without manual intervention.
-
Testing (Unit, Integration, Security, UAT)
In healthcare fintech, testing must be both comprehensive and continuous. Even small bugs can lead to claim rejections, delayed payments, or compliance violations. Testing is not a one-time task—it should occur at every stage of development.
Key testing activities include:
- Unit Testing: Validate each feature or module individually (e.g., invoice calculation logic).
- Integration Testing: Ensure smooth data exchange between the payment system, EHR, and insurer APIs.
- Security Testing: Conduct penetration tests, vulnerability scans, and encryption validation.
- User Acceptance Testing (UAT): Have real users—providers, billing teams, and patients—test the system in real-world scenarios.
Example: A hospital might run UAT by processing a week’s worth of sample patient bills and claims, verifying that every transaction matches expected outcomes before fully switching to the new system.
-
Deployment and Data Migration
Deployment is when the system moves from development into active use. In healthcare finance, a sudden “big bang” switch can be risky, so most organizations adopt a phased or pilot rollout.
Key deployment activities:
- Pilot Rollout: Implement in one department or clinic to identify issues before full launch.
- Data Migration: Transfer billing records, patient balances, and claims history with full encryption.
- Parallel Running: Operate old and new systems side-by-side to compare results and spot discrepancies.
Example: A multi-location clinic might deploy the payment system first in its outpatient department, refine workflows, then extend to inpatient services and satellite branches.
-
Post-Launch Monitoring and Optimization
Post-launch monitoring ensures the system stays compliant, secure, and efficient. This phase is about continuous improvement, informed by performance metrics and user feedback.
Monitoring Activities:
- Performance Tracking: Measure transaction processing times, claim approval rates, and patient payment completion rates.
- Security Audits: Conduct periodic penetration tests and compliance checks.
- Error Resolution: Use automated alerts for failed transactions, rejected claims, or API connection issues.
Optimization Opportunities:
- AI-Powered Analytics: Implement predictive models for cash flow forecasting and denial prevention.
- Patient Self-Service Enhancements: Add BNPL options, subscription payment plans, or automated reminders.
- API Expansion: Integrate with more payer networks for faster claim turnaround.
Example: If monitoring shows a spike in claim denials for one insurer, the billing team can adjust coding practices or update integration rules before revenue impact escalates.
Integration with Insurance and EHR Systems
A healthcare payment system delivers its full potential only when it operates as part of a connected ecosystem. Standalone payment platforms may process transactions efficiently, but without integration with insurance systems and Electronic Health Records (EHR), they risk creating manual workarounds, data inconsistencies, and patient frustration. The goal of integration is to ensure that financial workflows are directly linked to clinical and administrative processes, eliminating duplication and reducing delays.
In this section, we explore three core integration capabilities: linking payments with claims management systems, enabling real-time eligibility and benefits verification, and automating patient statements directly from EHR records.
-
Linking Payments with Claims Management Systems
For most healthcare providers, a large portion of revenue comes from insurance reimbursements. This means that claims management and payment processing must be tightly interconnected. Without integration, billing staff might need to manually update claim statuses, reconcile payments, and chase down underpaid claims—work that is both time-consuming and error-prone.
How integration works:
The payment system connects directly to a claims management platform or insurer API, allowing automatic updates as claims move through submission, review, approval, or denial. When a payment is received, the system can automatically match it to the relevant claim and mark it as settled.
Benefits of integration include:
- Faster Reconciliation: Payments are automatically linked to claims, eliminating manual cross-checking.
- Reduced Errors: Automatic matching prevents posting payments to the wrong account.
- Improved Cash Flow: Shortens the time from claim submission to payment settlement.
Example in practice:
A hospital submits a claim for a knee replacement surgery. The claims system shows the insurer has approved 90% of the billed amount. The payment system records this approval in real time, posts the reimbursement, and instantly generates a bill for the patient’s remaining balance—all without staff intervention.
-
Real-Time Eligibility and Benefits Verification
Eligibility verification is one of the most important—and often most overlooked—steps in preventing payment disputes. If a provider delivers a service that isn’t covered under a patient’s plan, the claim may be denied, resulting in lost revenue and patient dissatisfaction.
How real-time verification works:
Through integration with payer APIs, the payment system can instantly check a patient’s insurance coverage, deductible status, co-pay requirements, and benefit limits before a service is rendered. This check can be done at the time of appointment scheduling or during patient check-in.
Advantages of real-time verification:
- Fewer Denials: Coverage is confirmed before treatment, reducing denied claims.
- Upfront Cost Transparency: Patients know in advance what their insurance will cover and what they’ll owe.
- Operational Efficiency: Eliminates the need for follow-up calls to insurers.
Example in practice:
A patient schedules an MRI. Before confirming the appointment, the clinic’s payment system checks the insurer’s database, confirms the MRI is covered, and informs the patient they will have a $200 co-pay. This transparency reduces payment disputes and speeds up billing.
-
Automating Patient Statements Directly from EHR Records
In many healthcare organizations, billing teams manually extract treatment details from EHR systems to prepare patient statements. This manual transfer introduces delays and increases the risk of errors, such as missing services or incorrect coding.
How automation works:
The payment system integrates with the EHR through secure APIs, pulling relevant encounter data—such as diagnosis codes, procedure codes, and treatment dates—directly into the billing module. This allows the system to generate itemized patient statements automatically, without human intervention.
Benefits of EHR-driven automation:
- Speed: Statements are generated and delivered as soon as services are recorded in the EHR.
- Accuracy: Eliminates transcription errors by pulling data directly from the source.
- Consistency: Ensures that the medical and financial records match exactly.
Example in practice:
A patient completes a series of physiotherapy sessions. As soon as the therapist logs the final session in the EHR, the payment system pulls the record, calculates the patient’s balance after insurance coverage, and sends an itemized bill to the patient portal within minutes.
When payment systems are deeply integrated with insurance and EHR platforms, financial transactions become part of the natural clinical workflow. This means fewer administrative tasks for staff, faster reimbursements, greater billing accuracy, and a smoother patient experience.
Such integration also positions healthcare providers to adopt value-based care models and advanced analytics. With synchronized clinical and financial data, providers can track the true cost of care, identify inefficiencies, and make informed decisions about service delivery.
In short, integration is not just a technical upgrade—it’s a strategic enabler that transforms payment systems from isolated tools into essential components of a unified healthcare ecosystem.
Cost of Developing a Healthcare Payment System
The cost of developing a healthcare payment system can vary significantly depending on system complexity, regulatory requirements, technology stack, and development approach. Building such a system is not just about writing code—it involves designing secure financial workflows, ensuring regulatory compliance, integrating with external healthcare and payment platforms, and maintaining the solution over time.
Understanding the key cost drivers is essential for budgeting and for deciding whether to build in-house or outsource the project. Below, we break down the major factors influencing cost, compare in-house vs. outsourced development, and explore ongoing operational expenses.
Factors Affecting Cost
The total development cost is shaped by a combination of technical, operational, and compliance-related factors. The more advanced the system’s features, integrations, and security requirements, the higher the cost will be.
Key cost drivers include:
- System Complexity:
A basic payment platform with standard billing, payment gateway integration, and invoice generation will cost far less than a fully integrated healthcare payment ecosystem that includes real-time insurance verification, multi-currency support, AI-powered fraud detection, and predictive analytics.
- Regulatory Compliance Requirements:
Building for compliance with HIPAA, PCI-DSS, and GDPR increases cost because developers must implement advanced encryption, tokenization, access controls, and secure hosting environments. Regular third-party audits and penetration testing also add to the budget.
- Integration Scope:
Connecting to multiple EHR/EMR systems, insurance provider APIs, and payment processors requires extensive development work and thorough testing. Each integration may have unique protocols, data formats, and compliance implications, increasing complexity.
- User Experience (UX) and Accessibility:
Designing patient-friendly portals, ADA-compliant interfaces, and multilingual support requires additional design and development resources.
- Scalability and Redundancy:
A high-availability architecture with load balancing, failover capabilities, and disaster recovery infrastructure adds upfront infrastructure and engineering costs.
Example in practice:
A small clinic payment system with basic credit card payments might cost $80,000–$100,000 to develop, while a hospital network’s multi-integration, compliance-heavy platform could easily exceed $500,000 in initial build costs.
In-House vs. Outsourced Development Cost Comparison
Choosing between in-house development and outsourcing has major cost implications. Each option has advantages and trade-offs in terms of control, expertise, and speed to market.
In-House Development:
- Pros:
- Complete control over design and architecture.
- Direct collaboration between development and operational teams.
- Easier to maintain proprietary control over intellectual property.
- Complete control over design and architecture.
- Cons:
- Requires hiring full-time developers, compliance experts, and DevOps engineers.
- Longer ramp-up time due to team formation and onboarding.
- Higher ongoing payroll costs.
- Requires hiring full-time developers, compliance experts, and DevOps engineers.
Estimated Cost:
- Salaries for a typical in-house team (project manager, UI/UX designer, backend developer, frontend developer, QA engineer, security specialist) can exceed $500,000 annually in the U.S. market.
Outsourced Development:
- Pros:
- Access to specialized expertise in healthcare compliance and payment integrations.
- Faster development timelines with pre-established processes and toolsets.
- Lower labor costs if outsourcing to regions with competitive rates.
- Access to specialized expertise in healthcare compliance and payment integrations.
- Cons:
- Potential communication and time zone challenges.
- Requires careful vendor selection to ensure HIPAA and PCI-DSS compliance.
- Potential communication and time zone challenges.
Estimated Cost:
- Outsourcing to a specialized healthcare software firm can cost $150,000–$300,000 for a compliant, integrated payment system, depending on scope and complexity.
Example in practice:
A mid-sized telehealth company outsourced development to a vendor with existing EHR and payment integration experience, reducing project delivery time from 12 months to 7 months while saving nearly 40% on labor costs compared to in-house hiring.
Ongoing Maintenance and Support Costs
Once the healthcare payment system is live, ongoing costs must be factored into the budget. Maintenance is essential to keep the platform secure, compliant, and compatible with evolving payer APIs, EHR systems, and payment gateway updates.
Typical ongoing costs include:
- Compliance Audits and Security Updates:
- Annual or biannual HIPAA, PCI-DSS, and GDPR compliance reviews.
- Continuous security patching and vulnerability scanning.
- Annual or biannual HIPAA, PCI-DSS, and GDPR compliance reviews.
- API and Integration Updates:
- Regular adjustments to keep pace with insurer API changes, EHR upgrades, or new payment processor requirements.
- Regular adjustments to keep pace with insurer API changes, EHR upgrades, or new payment processor requirements.
- Infrastructure Costs:
- Cloud hosting fees (AWS, Azure, or GCP HIPAA-compliant environments).
- Backup, disaster recovery, and redundancy services.
- Cloud hosting fees (AWS, Azure, or GCP HIPAA-compliant environments).
- Technical Support and Helpdesk:
- Ongoing availability of technical staff to resolve bugs, handle user requests, and manage upgrades.
- Ongoing availability of technical staff to resolve bugs, handle user requests, and manage upgrades.
- Feature Enhancements:
- Adding new capabilities such as AI-driven analytics, patient BNPL options, or additional currency/payment method support.
- Adding new capabilities such as AI-driven analytics, patient BNPL options, or additional currency/payment method support.
Estimated Annual Maintenance Budget:
- For small-to-mid-sized systems: $50,000–$100,000/year.
- For enterprise-scale systems with multiple integrations: $150,000–$250,000/year.
Example in practice:
A regional hospital group allocates 20% of its initial development budget annually for system updates, compliance audits, and feature expansion to keep pace with insurance policy changes and patient payment expectations.
The development cost of a healthcare payment system is highly variable—ranging from $80,000 for basic implementations to over $500,000 for enterprise-grade, fully integrated, compliance-heavy platforms. The decision between in-house and outsourced development will depend on available talent, budget, and desired speed to market. Importantly, post-launch maintenance is a recurring investment, not a one-time expense, and should be factored into long-term planning.
Organizations that plan comprehensively—considering complexity, compliance, integration scope, and total cost of ownership—will be better positioned to build a payment system that is both financially viable and operationally sustainable.
Common Challenges and How to Overcome Them
Even the most advanced healthcare payment systems face operational and technical challenges. These obstacles can disrupt cash flow, delay reimbursements, increase administrative workloads, and negatively impact patient satisfaction. Recognizing these challenges early—and building strategies to overcome them—is critical for healthcare organizations looking to maximize the efficiency and ROI of their payment systems.
-
Regulatory Hurdles
Regulatory compliance is one of the most persistent challenges in healthcare payments. With frameworks like HIPAA in the U.S., PCI-DSS for payment security, and GDPR in Europe, payment systems must be designed to handle sensitive medical and financial data with the highest security standards. Non-compliance can lead to costly fines, reputational damage, and even legal action.
Regulations can also change over time. For example, updates to HIPAA’s Privacy Rule or new payment card security requirements can force system modifications post-launch. For organizations operating in multiple jurisdictions, managing compliance with differing laws becomes even more complex.
Overcoming this challenge involves:
- Compliance by Design: Embed encryption, access controls, and audit trails from the earliest development stages.
- Regular Audits: Schedule quarterly or biannual compliance reviews to ensure ongoing adherence.
- Vendor Vetting: Work only with cloud hosts, payment processors, and API providers that hold HIPAA, PCI-DSS, and GDPR certifications.
Example in practice:
A telehealth provider working across the U.S. and EU uses a hybrid architecture—storing EU patient data on GDPR-compliant EU servers while processing U.S. payments through HIPAA-certified U.S. gateways—to meet regional regulations without sacrificing performance.
-
Delayed Claim Reimbursements
Slow insurance claim reimbursements can severely impact cash flow for healthcare providers. Delays often stem from claim denials, incomplete documentation, or manual submission processes. Even minor coding errors can result in weeks or months of payment delays, forcing providers to dedicate staff to resubmitting claims and following up with insurers.
Overcoming this challenge involves:
- Automated Claim Validation: Integrate with claims management systems to check for coding errors or missing data before submission.
- Real-Time Eligibility Verification: Confirm patient coverage before treatment to avoid claim rejections.
- Claim Tracking Dashboards: Provide billing teams with live updates on claim statuses, enabling faster follow-ups.
Example in practice:
A hospital integrated its payment system with a clearinghouse that automatically validates CPT and ICD codes. This reduced claim rejection rates by 30% and improved average reimbursement times by two weeks.
-
Data Integration Issues
Data silos are a common problem in healthcare. When payment systems don’t integrate smoothly with EHRs, insurance databases, and payment gateways, staff are forced to manually transfer data between platforms—leading to duplication, delays, and errors. Lack of interoperability also makes it difficult to get a complete financial picture for reporting and decision-making.
Overcoming this challenge involves:
- Standards-Based APIs: Use HL7 and FHIR protocols for smooth EHR integration.
- Single Source of Truth: Centralize financial and clinical data to ensure consistency across platforms.
- Regular Integration Testing: Continuously verify that all connected systems are exchanging data accurately.
Example in practice:
A multi-specialty clinic adopted a centralized payment and billing platform that used FHIR APIs to sync with its EHR in real time. As soon as a provider entered a procedure in the EHR, the payment system generated the invoice and submitted the insurance claim automatically.
-
High Transaction Failure Rates
Payment failures—whether due to technical errors, network downtime, or security issues—can frustrate patients and delay revenue collection. Failures are particularly damaging in healthcare because patients may require urgent services and expect payment processes to work flawlessly. High transaction failure rates can also lead to repeated charges, refunds, and increased support costs.
Overcoming this challenge involves:
- Multiple Payment Gateways: Integrate with more than one processor to enable automatic failover if one service goes down.
- Real-Time Transaction Monitoring: Identify and resolve issues such as declined payments or API errors immediately.
- Network Redundancy: Use load balancers and backup servers to maintain uptime.
- Tokenization and PCI Compliance: Reduce security-related transaction failures caused by blocked or suspicious payments.
Example in practice:
A large hospital system implemented dual payment gateways—one for credit/debit cards and another for mobile wallets. If the primary processor failed, transactions were automatically routed through the secondary gateway, keeping payment success rates above 99.5%.
Healthcare payment systems operate in a highly regulated, high-stakes environment. Regulatory compliance, delayed reimbursements, integration gaps, and payment failures can quickly erode trust and financial stability. However, by designing with compliance in mind, automating claims workflows, using standards-based integrations, and building fault-tolerant payment infrastructures, providers can overcome these challenges effectively.
The organizations that invest in proactive solutions—rather than reactive fixes—are better positioned to deliver a payment experience that is fast, secure, and reliable, while maintaining the financial health of their practice or network.
Why Choose Aalpha for Healthcare Payment System Development
Selecting the right development partner is critical when building a healthcare payment system, as the platform must meet strict compliance standards, integrate seamlessly with existing healthcare infrastructure, and perform reliably under high transaction volumes. Aalpha Information Systems has a proven track record of delivering secure, high-performance payment solutions for healthcare providers, insurers, and healthtech companies across multiple regions.
Specialized Healthcare and Fintech Expertise
Aalpha operates at the intersection of healthcare and financial technology, bringing domain-specific knowledge in HIPAA, PCI-DSS, and GDPR compliance. This expertise allows us to design systems that meet clinical data security requirements while also supporting advanced financial workflows such as claims processing, multi-currency transactions, and real-time payment reconciliation.
Full-Stack Development Capability
Our team covers the entire lifecycle—from requirements gathering and compliance planning to system design, development, and post-launch optimization. Whether building patient-facing portals, provider dashboards, or back-end billing engines, we ensure every component works cohesively and can adapt to future enhancements like AI-powered reconciliation or blockchain-based claims validation.
Proven Integration Skills
We have extensive experience integrating payment systems with EHR/EMR platforms, insurance APIs, and third-party payment gateways. This ensures that clinical and financial data flow in real time, reducing manual entry, minimizing errors, and improving claim approval rates.
Focus on Security and Scalability
Every Aalpha-built platform includes encryption, tokenization, role-based access controls, and secure API management. Our architectures are designed for scalability, allowing the system to handle growth in transaction volumes and integration demands without compromising performance.
Transparent Delivery and Support
Aalpha provides clear development roadmaps, regular progress updates, and post-deployment support packages. This includes compliance audits, performance monitoring, and feature upgrades to keep the system aligned with industry changes and evolving regulations.
By choosing Aalpha, healthcare organizations gain a technology partner capable of delivering a payment system that is secure, compliant, and engineered for operational reliability—ready to support both current needs and future innovations in healthcare finance.
Future Trends in Healthcare Payment Systems
Healthcare payment systems are moving toward greater automation, accuracy, and interoperability. Advances in artificial intelligence, distributed ledger technology, global payment infrastructure, and connected health devices are creating new ways for providers, payers, and patients to complete financial transactions with less friction and greater precision. The trends outlined below represent developments that are already in motion and likely to have significant operational impact in the coming years.
-
AI-Powered Payment Reconciliation
Payment reconciliation is a recurring challenge in healthcare finance. Matching incoming payments from patients and insurers to the correct invoices and claims can be slow and prone to error when handled manually.
Artificial intelligence can handle this process in real time by cross-referencing payment details, claim data, and service records. Machine learning models identify underpayments, overpayments, and mismatches, then generate alerts for staff review or automatically post the correct entries.
Key advantages:
- Faster processing: Minutes instead of days to reconcile large volumes of payments.
- Higher accuracy: Reduction in posting errors and missed transactions.
- Forecasting capability: Models can predict payment timelines based on payer history.
Example: A regional hospital group uses AI reconciliation to automatically identify short-paid claims and send follow-up requests to insurers, recovering revenue that would otherwise be overlooked.
-
Blockchain-Based Claims Processing
Claims processing often involves multiple intermediaries, slow review cycles, and inconsistent records. Blockchain technology offers a shared, tamper-resistant ledger that all participants—providers, payers, and auditors—can access.
Smart contracts can be programmed to verify patient eligibility, confirm that billed services match authorized procedures, and trigger payment once criteria are met. Because every transaction is time-stamped and immutable, disputes over claim changes are greatly reduced.
Key advantages:
- Single source of truth for claim status and payment history.
- Automated claim validation through smart contracts.
- Reduced administrative costs from fewer disputes and manual checks.
Example: An insurance consortium pilots a blockchain-based claims network with partner hospitals, cutting average settlement time from 30 days to under a week.
-
Real-Time Cross-Border Payments for Telehealth
As telehealth expands internationally, cross-border transactions are becoming routine. Traditional bank transfers for medical services can take days, with high fees and unfavorable currency conversions.
Modern payment rails—using fintech platforms, blockchain settlement layers, or ISO 20022 messaging—enable near-instant transfers in multiple currencies. Invoices can be generated in a patient’s local currency, with conversion and settlement handled automatically.
Key advantages:
- Immediate settlement instead of multi-day delays.
- Lower transaction costs compared to legacy bank transfers.
- Transparent currency conversion and fee structures.
Example: A U.S. telehealth provider serving patients in Europe uses a multi-currency payment gateway to collect euros and pounds in real time, automatically reconciling transactions into its U.S. accounting system.
-
Integration with Wearable Health Devices for Automated Billing
Connected health devices such as smartwatches, heart monitors, and continuous glucose meters generate large volumes of patient data. When integrated with payment systems, these devices can trigger automated billing based on predefined clinical events or service thresholds.
For example, if wearable data indicates a change that requires a teleconsultation, the payment system can automatically create an invoice, send it to the payer or patient, and process the payment once the service is delivered.
Key advantages:
- Accurate, usage-based billing linked to actual health events.
- Reduced manual input for recurring monitoring programs.
- Timely care delivery linked directly to payment readiness.
Example: A subscription-based cardiac monitoring service connects its payment system to patients’ wearable ECG devices. When irregular heart activity is detected, the system schedules a consultation and bills the patient’s plan automatically.
These trends—AI-driven reconciliation, blockchain-enabled claims, instant cross-border settlements, and wearable-triggered billing—are shifting healthcare payments toward real-time, data-driven, and verifiable transactions. Organizations that adopt these technologies early will be better positioned to handle growing transaction volumes, reduce administrative overhead, and improve the payment experience for all parties.
Conclusion
A healthcare payment system built to handle high transaction volumes, strict compliance requirements, and complex integration needs is a core operational asset. For many organizations, the challenge lies not in understanding the need but in executing a build that meets regulatory, technical, and user expectations without unnecessary delays or cost overruns.
Aalpha Information Systems brings specialized experience in developing payment platforms that meet HIPAA, PCI-DSS, and GDPR standards, integrate with leading EHR and insurance systems, and support multi-channel payment processing. Projects are delivered with a focus on secure architecture, efficient workflows, and adaptability to future requirements such as AI-driven reconciliation or blockchain-based claims.
By working with a development partner that understands both healthcare and fintech environments, organizations can reduce implementation risk, meet compliance obligations from day one, and operate on infrastructure built for accuracy, security, and scale.
FAQs – Healthcare Payment System Development
How long does it take to build a healthcare payment system?
A basic platform with billing and payment gateway integration can take 4–6 months. Mid-tier systems with EHR integration and claims processing may take 7–10 months. Enterprise-level builds with AI, blockchain, and multi-currency support can take 12–18 months, including compliance testing.
Can a payment system be integrated into my existing EHR?
Yes. Most modern EHRs support integration via FHIR or HL7 APIs, allowing automatic transfer of service, patient, and billing data. For older EHRs, middleware may be needed, adding time and cost.
What security measures are required for HIPAA compliance?
HIPAA requires:
- Encryption: AES-256 for stored data, TLS 1.2+ for data in transit.
- Access Control: Role-based permissions and multi-factor authentication.
- Audit Logs: Tracking all access and changes to ePHI.
How do I choose the right payment gateway for healthcare transactions?
Select a PCI-DSS compliant gateway that supports multiple payment methods, integrates with your system, and offers fraud prevention tools. Consider fees, settlement times, and availability in your operating regions.
Is blockchain useful for healthcare billing?
Yes, for claims validation and fraud prevention. Blockchain creates an immutable record of transactions, and smart contracts can automate claim approvals and payments, reducing disputes and delays.
Can small clinics afford to build a payment system?
Yes. Clinics can start with a smaller cloud-based system, integrating essential features like billing and payment processing, then expand to claims and EHR integration over time to spread costs.
Build a secure, compliant, and efficient healthcare payment system with Aalpha’s proven expertise. Contact us today to discuss your project requirements and get a tailored development plan.