What is Healthcare Automation Software?
Healthcare automation software refers to digital systems designed to automate clinical, administrative, and operational tasks in medical settings. These systems use technologies such as artificial intelligence (AI), machine learning (ML), robotic process automation (RPA), and rule-based logic to perform tasks that traditionally require manual input from medical or administrative staff. Examples include automated patient appointment scheduling, real-time insurance eligibility checks, electronic health record (EHR) updates, clinical documentation assistance, and AI-powered triage systems.
In simpler terms, healthcare automation software reduces the human workload by taking over repetitive or logic-based tasks—allowing physicians, nurses, and administrators to focus on high-value decision-making and patient care.
Core Goals: Efficiency, Accuracy, Compliance, and Patient Outcomes
Healthcare automation initiatives are not driven by novelty but by pressing operational and clinical needs. At the core, healthcare automation software serves four primary goals:
- Operational Efficiency:
Hospitals and clinics often struggle with staff shortages, legacy workflows, and paperwork-heavy environments. Automation helps standardize and expedite tasks such as patient intake, prescription renewals, or billing—freeing up valuable time and reducing administrative bottlenecks. - Accuracy and Consistency:
Manual errors in documentation, coding, or claims can lead to denied reimbursements, compliance violations, and medical risks. Automation enforces consistency and eliminates common human errors, especially in data-heavy processes like medical billing or test result management. - Regulatory Compliance:
Healthcare systems operate under strict compliance frameworks such as HIPAA in the U.S., GDPR in Europe, or NABH standards in India. Automation helps enforce privacy protocols, access controls, and data audit trails to meet these obligations. For instance, software can automatically encrypt patient data, trigger alerts for unusual access patterns, and log all interactions with protected health information (PHI). - Improved Patient Outcomes:
Automation is not merely about reducing costs—it plays a direct role in improving care. Clinical decision support tools can flag drug interactions, automation bots can schedule timely follow-ups, and AI can triage incoming symptoms for faster diagnosis. All of this contributes to safer, faster, and more personalized care delivery.
Why Healthcare Needs Automation Now: Real-World Triggers Driving Demand
The demand for healthcare automation software has accelerated sharply post-2020, driven by a convergence of systemic challenges and technology readiness. These include:
- Staffing Shortages and Burnout:
According to the American Hospital Association, the U.S. alone is projected to face a shortage of over 200,000 nurses by 2030. Similar shortages exist globally. Automation fills this gap by offloading repetitive and clerical tasks from frontline workers. - Data Explosion:
The rise of digital health records, wearables, imaging systems, and connected devices has created vast quantities of health data. Manually managing this data is no longer feasible. Automation enables real-time data parsing, integration, and interpretation—especially crucial in emergency or critical care scenarios. - Patient Expectations and Digital-First Behavior:
Patients today expect the same digital convenience in healthcare that they experience with fintech or e-commerce. Automated self-scheduling, digital check-ins, and AI-powered symptom checkers improve patient satisfaction and reduce no-show rates. - Payer Pressure and Administrative Overload:
A 2023 Health Affairs study found that U.S. healthcare providers spend over $20 billion annually on billing-related administrative work. Automation in revenue cycle management (RCM)—from eligibility verification to automated claims scrubbing—offers a clear ROI. - Pandemic-Era Systemic Stress Tests:
COVID-19 exposed the fragility of manual systems and siloed data. Health systems that had already implemented automation were able to quickly pivot with virtual care, automated contact tracing, and vaccine logistics. Those without automation struggled. - Technological Maturity:
The maturity of cloud platforms, APIs, healthcare-specific LLMs (e.g., MedPaLM 2), and no-code automation builders has significantly lowered the barrier to entry. Mid-sized hospitals and outpatient centers can now deploy automation tools that were once limited to large health systems.
This guide is designed to help CTOs, product managers, and digital health leaders understand how to strategically develop or implement healthcare automation software. As automation transitions from being a “nice to have” to a “need to have,” knowing where to start—and how to get it right—is critical.
It will cover market trends, common use cases, technology stack decisions, security requirements, integration strategies, and real-world implementation challenges. Whether you’re building in-house systems or evaluating vendors, this guide will give you the framework to build compliant, high-impact automation solutions that scale.
Market Size, Trends & Growth Forecast (2025–2030)
Global Healthcare Automation Market Size: Figures and Projections
The global healthcare automation market is experiencing significant growth, driven by the increasing demand for operational efficiency, improved patient outcomes, and cost reduction in healthcare settings. In 2024, the market was valued at approximately USD 42.36 billion and is projected to reach USD 87.16 billion by 2032, reflecting a compound annual growth rate (CAGR) of 9.44%.
This growth trajectory is underpinned by advancements in artificial intelligence (AI), machine learning (ML), and robotic process automation (RPA), which are revolutionizing healthcare delivery by streamlining administrative tasks, enhancing diagnostic accuracy, and optimizing treatment processes.
Segmentation: Administrative, Clinical, and Operational Automation
The healthcare automation market can be segmented into three primary categories: administrative, clinical, and operational automation.
- Administrative Automation: This segment encompasses solutions aimed at automating non-clinical tasks such as billing, scheduling, and claims processing. The U.S. healthcare information system market, which includes administrative automation, was valued at USD 214.25 billion in 2023 and is projected to reach USD 664.24 billion by 2033, growing at a CAGR of 11.98%.
- Clinical Automation: This segment focuses on automating clinical tasks, including diagnostics, treatment planning, and patient monitoring. The global clinical workflow solutions market, a key component of clinical automation, is expected to grow from USD 13.36 billion in 2025 to USD 23.71 billion by 2030, at a CAGR of 12.15% .
- Operational Automation: This segment involves automating hospital operations such as inventory management and supply chain logistics. The pharmacy automation market, a subset of operational automation, is projected to grow from USD 6.65 billion in 2024 to USD 10.00 billion by 2030, at a CAGR of 7.1%.
Regional Adoption Trends: U.S., Europe, India, and APAC
-
United States
The U.S. leads in healthcare automation adoption, driven by substantial investments in healthcare IT infrastructure and a focus on improving patient care. The U.S. healthcare information system market is projected to reach USD 664.24 billion by 2033, indicating robust growth in automation technologies.
-
Europe
Europe is witnessing significant growth in healthcare automation, propelled by government initiatives and the adoption of advanced technologies. The European Union is expected to contribute USD 50.24 billion to the global AI healthcare market by 2028, underscoring the region’s commitment to integrating AI and automation in healthcare.
-
India
India’s healthcare automation market is expanding rapidly, fueled by the government’s push for digital health initiatives and the increasing adoption of AI and ML technologies. The integration of automation in India’s healthcare sector is enhancing efficiency and accessibility, particularly in remote and underserved areas.
-
Asia-Pacific (APAC)
The APAC region is experiencing the fastest growth in healthcare automation, driven by rising healthcare expenditures, technological advancements, and increasing demand for quality healthcare services. The region’s focus on adopting AI and IoT technologies is transforming healthcare delivery and operational efficiency.
Key Drivers: Labor Shortages, Regulatory Push, AI Readiness
-
Labor Shortages
Healthcare systems worldwide are grappling with labor shortages, leading to increased workloads and burnout among healthcare professionals. Automation technologies are being adopted to alleviate these challenges by streamlining workflows and reducing administrative burdens.
-
Regulatory Push
Governments and regulatory bodies are advocating for the adoption of automation in healthcare to enhance efficiency, reduce errors, and improve patient outcomes. Initiatives such as the U.S. Office of the National Coordinator for Health Information Technology’s (ONC) strategic plans emphasize the importance of integrating automation and interoperability standards in healthcare systems .
-
AI Readiness
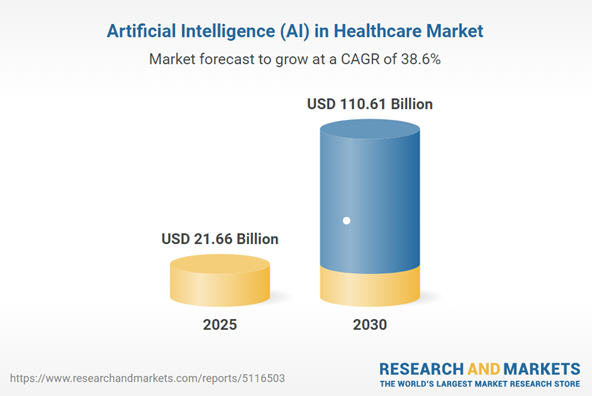
The readiness to adopt AI technologies is a significant driver of healthcare automation. The global market for Artificial Intelligence (AI) in healthcare is expected to grow from USD 21.66 billion in 2025 to USD 110.61 billion by 2030, registering a compound annual growth rate (CAGR) of 38.6% during the forecast period. This growth reflects the increasing integration of AI in various healthcare applications, including diagnostics, patient monitoring, and administrative tasks.
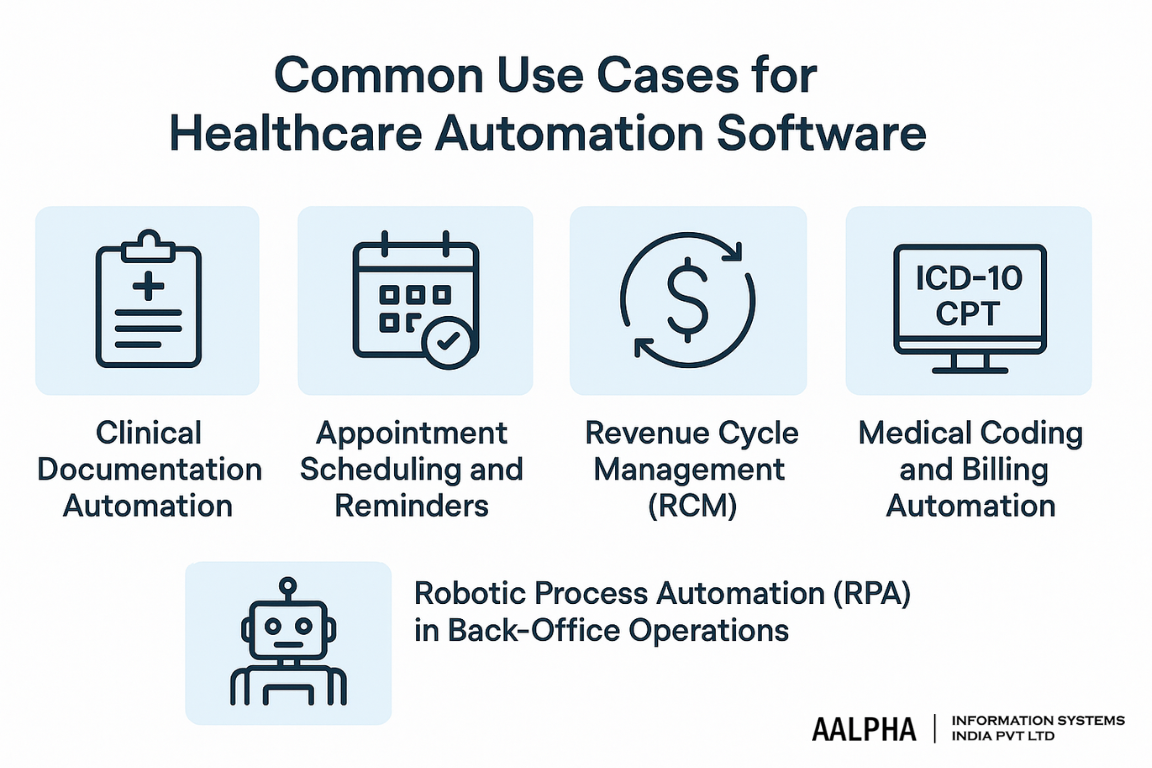
Common Use Cases for Healthcare Automation Software
Healthcare automation is not a monolithic solution—it encompasses a wide range of specific use cases across clinical, administrative, and operational workflows. The following use cases represent the most impactful areas where automation software is actively transforming healthcare delivery in hospitals, clinics, and payer-provider networks.
1. Clinical Documentation Automation
Manual clinical documentation is time-consuming, error-prone, and a major source of burnout among clinicians. According to a 2022 study published in JAMA Internal Medicine, physicians spend nearly two hours on EHR and documentation tasks for every hour of direct patient interaction. This inefficiency has made documentation one of the earliest targets for healthcare automation.
Modern clinical documentation tools now integrate voice recognition, NLP (natural language processing), and LLMs (large language models) like GPT-4 or Med-PaLM to automatically transcribe and structure physician notes. Some systems even provide real-time clinical summarization, convert voice inputs to structured SOAP notes, and flag incomplete entries.
For example, Nuance DAX (Dragon Ambient eXperience), powered by Microsoft, uses ambient listening and AI to generate clinical notes from doctor–patient conversations—allowing physicians to focus on care rather than data entry.
2. Appointment Scheduling and Reminders
Missed appointments cost U.S. healthcare providers over $150 billion annually, according to the American Journal of Managed Care. Automating appointment scheduling and reminder systems significantly reduces these no-shows and improves operational efficiency.
Automation software can:
- Allow patients to self-schedule or reschedule appointments via patient portals or chatbots
- Automatically confirm appointments using SMS, email, or push notifications
- Adjust appointment slots dynamically based on provider availability or cancellations
- Route priority cases using triage algorithms powered by AI
An example is Zocdoc, which automates real-time scheduling across multiple providers while integrating with EHR calendars. Other systems embed scheduling directly into provider websites and allow for two-way confirmation to reduce gaps.
In hospital systems, robotic schedulers can allocate imaging appointments, lab visits, or follow-ups based on rules and availability.
3. Revenue Cycle Management (RCM)
Revenue Cycle Management is an ideal candidate for end-to-end automation due to its reliance on rules, forms, and structured workflows. Automation in RCM reduces denied claims, accelerates payments, and ensures regulatory compliance. RCM automation generally spans several touchpoints:
- Pre-authorization and eligibility checks using real-time payer integrations
- Claim creation and validation using RPA bots and AI coding assistants
- Automated appeals for rejected claims with template-driven resubmissions
- Patient balance estimation and auto-billing with payment plans
According to McKinsey & Company, automation can reduce administrative costs by up to 30% in RCM processes.
Platforms like Waystar, Olive, and R1 RCM offer AI-augmented revenue cycle tools that handle everything from eligibility verification to denial management with minimal human oversight.
4. Medical Coding and Billing Automation
Medical coding is critical for billing, compliance, and health data analytics—but it’s complex and time-intensive. Automation helps standardize this process using rule-based logic and AI/LLM-powered engines trained on ICD-10, CPT, HCPCS, and SNOMED codes.
There are two primary automation pathways:
- Computer-Assisted Coding (CAC):
Extracts relevant data from clinical documentation and recommends codes. For instance, 3M’s CAC system is used by health systems to improve coder productivity and accuracy.
- AI-Powered Auto-Coding:
Uses NLP and ML to analyze unstructured notes and assign codes autonomously. Some LLMs, fine-tuned on healthcare billing data, can now auto-code with accuracy on par with human coders.
Medical billing automation systems then process coded data, generate invoices, and route them through payer APIs, reducing time to reimbursement and minimizing rejected claims.
Hospitals using AI-based coding tools report up to a 40% reduction in coding turnaround time and significant improvement in accuracy.
5. Robotic Process Automation (RPA) in Back-Office Operations
Robotic Process Automation (RPA) refers to software bots that mimic human actions within digital systems. In healthcare, RPA bots are used to automate structured, rule-based tasks across administrative and back-office departments—especially where legacy systems lack API access.
Common RPA use cases in healthcare include:
- Patient registration and data entry from paper forms or scanned documents
- Insurance eligibility checks via payer portals
- Claims status tracking across clearinghouses
- Inventory and supply chain monitoring in hospitals
- HR onboarding and credential verification
- Interfacing between siloed systems (e.g., copying lab data from LIS to EHR)
RPA solutions like UiPath, Automation Anywhere, and Blue Prism offer healthcare-specific modules that connect with EMRs, billing systems, and external payer platforms without requiring deep software integrations.
For example, a large U.S. hospital system implemented RPA bots to handle over 80,000 insurance eligibility checks per month, reducing manual staff time by 70%.
Which Processes Can Be Automated in Healthcare?
When asked “What processes can be automated in healthcare?”, the list is expansive and growing with the capabilities of AI and machine learning. Automation now touches nearly every functional area:
- Front Office: Scheduling, patient onboarding, virtual assistants
- Clinical Support: Documentation, triage, diagnostics, coding
- Operations: Inventory, HR, supply chain, EHR migration
- Billing and Finance: Claims, payments, RCM, denials
- Compliance and Security: Audit trails, access logs, alert systems
Each use case brings measurable ROI, not only in cost savings but also in quality, speed, and safety.
The Strategic Value of Automating Healthcare Workflows
Automation is not simply a cost-cutting tool—it’s a strategic lever for delivering better care, faster. For CTOs, product managers, and healthcare IT leaders, understanding these use cases is critical when evaluating new systems or designing internal platforms.
A successful automation strategy focuses on high-volume, error-prone workflows where rules can be codified or patterns learned through AI. Additionally, combining automation with human oversight—especially in billing or clinical applications—ensures reliability and regulatory compliance.
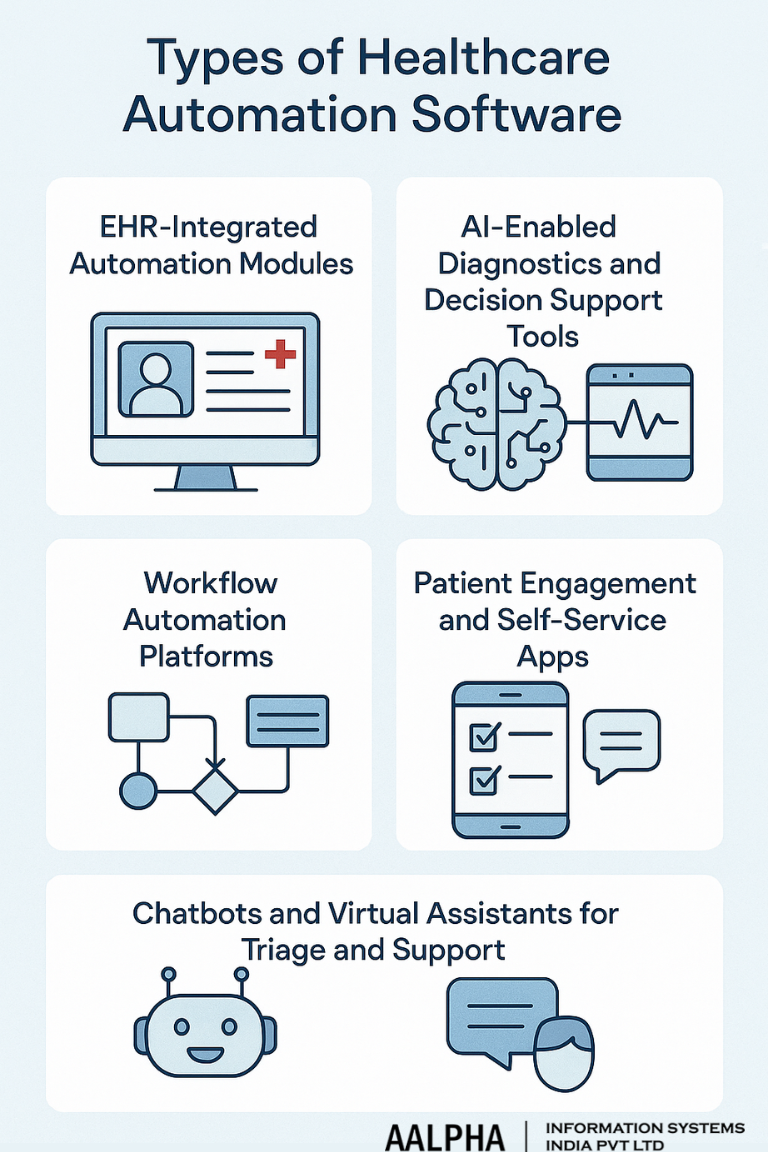
Types of Healthcare Automation Software
Healthcare automation software is not a single product but a layered ecosystem of specialized platforms and modules. These software systems span clinical care, diagnostics, operations, and patient engagement. Each serves a distinct purpose but increasingly integrates with others via APIs and interoperability standards like HL7 FHIR.
For healthcare leaders asking, “Which types of software are used for healthcare automation?”, the answer spans the following key categories:
1. EHR-Integrated Automation Modules
Electronic Health Record (EHR) systems form the digital backbone of modern healthcare. However, legacy EHRs were not designed for intelligent automation. In response, vendors and third-party developers have built automation modules that plug into EHR platforms to reduce manual tasks and improve clinician workflow.
Core functions of EHR-integrated automation include:
- Clinical documentation assistance (voice-to-text, summarization, templating)
- Order entry optimization (suggested labs or meds based on diagnosis)
- Population health management (automated alerts for preventive screenings)
- Care coordination (auto-referrals, task routing across departments)
- Billing and coding suggestions based on chart content
Major EHR vendors like Epic, Cerner (Oracle Health), and Allscripts have introduced intelligent automation features in their platforms. Epic’s “NoteWriter” and Cerner’s “Dynamic Documentation” are examples of AI-powered tools embedded directly in clinical workflows.
Some hospitals also use middleware (e.g., Redox, Mirth Connect) to extend automation beyond the core EHR, integrating with specialty apps or custom logic engines.
2. AI-Enabled Diagnostics and Decision Support Tools
One of the most transformative types of automation software involves AI-powered diagnostic and clinical decision support systems (CDSS). These tools analyze vast clinical datasets—including imaging, lab values, symptoms, and historical data—to suggest diagnoses, flag anomalies, or recommend treatment paths.
Examples of diagnostic automation:
- Radiology AI: Tools like Aidoc, Qure.ai, and Zebra Medical Vision detect abnormalities in X-rays, CTs, and MRIs faster than human readers in certain cases.
- Cardiology AI: Algorithms analyze ECGs or echocardiograms for arrhythmias or heart failure markers.
- Pathology AI: Whole-slide imaging platforms apply ML to assist pathologists with cancer grading and cell detection.
- Symptom checkers: Platforms like Isabel or Infermedica use probabilistic reasoning and LLMs to guide initial diagnoses.
Beyond diagnostics, CDSS platforms like IBM Watson (now Merative), UpToDate, and VisualDx embed clinical knowledge into physician decision-making. When integrated with EHRs, these tools suggest relevant actions at the point of care.
3. Workflow Automation Platforms
These platforms are designed to orchestrate, standardize, and optimize end-to-end workflows across departments, especially those involving multiple steps, approvals, or transitions of care.
Typical use cases:
- Patient admission, discharge, and transfer (ADT) automation
- Automated escalations in case of abnormal vitals or delayed test results
- Task assignments for care teams, nurses, or surgical coordinators
- Integration with backend systems (e.g., LIS, RIS, pharmacy, RCM)
Workflow automation platforms often include visual rule builders, logic-based triggers, drag-and-drop interfaces, and robust audit logging. Examples include Olive AI, Notable Health, and Catalia Health.
Some are built specifically for healthcare (with HIPAA compliance), while others—like Camunda, ProcessMaker, or AirSlate—are general-purpose BPM platforms that have been adapted for clinical operations.
4. Patient Engagement and Self-Service Apps
Automation isn’t limited to hospital staff—it also improves patient experience by enabling self-service and reducing manual coordination.
Key types of self-service automation software:
- Digital check-in systems: Let patients complete forms, insurance info, and consents via phone or kiosk.
- Pre-visit screening: Smart questionnaires that triage needs before arrival.
- Appointment and prescription reminders: Sent automatically via SMS, app, or email.
- Patient portals: Deliver test results, messages, bills, and educational content.
- Payment automation: Allow patients to pay bills or enroll in plans without calling the front desk.
Solutions like Phreesia, Luma Health, and MyChart (Epic) are widely adopted across health systems. These apps reduce administrative friction, increase patient satisfaction, and minimize delays in care coordination.
5. Chatbots and Virtual Assistants for Triage and Support
Chatbots are one of the fastest-growing areas of healthcare automation, often powered by conversational AI and large language models (LLMs). These systems interact with patients via websites, mobile apps, or even voice calls.
Capabilities of healthcare chatbots include:
- Symptom triage: Guide users through decision trees or AI-based suggestions
- Appointment booking or changes
- Insurance verification
- Prescription refill requests
- FAQ responses (e.g., location, hours, instructions)
- Post-discharge follow-up questions or check-ins
Advanced chatbots use natural language understanding (NLU) to carry out more nuanced conversations. For example, Florence, Ada Health, and Sensely integrate LLMs to answer patient questions based on evidence-based protocols.
Healthcare providers also build in-house virtual agents using platforms like Dialogflow, Microsoft Bot Framework, or Amazon HealthLake paired with GPT-based models.
Choosing the Right Software for Automation Goals
The right type of healthcare automation software depends on your strategic goals:
- If you’re optimizing clinical workflows, start with EHR-integrated modules and CDSS tools.
- To improve operational efficiency, invest in workflow automation platforms and RPA bots.
- For patient satisfaction and retention, deploy engagement apps and virtual assistants.
Healthcare CTOs and IT leaders should approach automation with a modular mindset—combining interoperable components that integrate securely into the larger health IT environment.
Core Features and Capabilities to Include
When evaluating or developing healthcare automation software, it’s imperative to consider features that ensure security, compliance, interoperability, and operational efficiency. Below are the essential components that such systems should encompass:
1. Role-Based Access Control (RBAC)
What is RBAC, and why is it essential in healthcare automation systems?
Role-Based Access Control (RBAC) is a security mechanism that restricts system access to authorized users based on their roles within an organization. In healthcare, RBAC ensures that individuals access only the information necessary for their duties, thereby protecting sensitive patient data.
Benefits of RBAC:
- Enhanced Security: By limiting access, RBAC minimizes the risk of data breaches.
- Regulatory Compliance: Helps meet standards like HIPAA and GDPR by ensuring only authorized personnel access Protected Health Information (PHI).
- Operational Efficiency: Streamlines user management by assigning permissions to roles rather than individuals.
Implementing RBAC is crucial for maintaining data integrity and confidentiality in healthcare systems.
2. HL7/FHIR Interoperability
How does HL7/FHIR interoperability enhance healthcare automation?
Health Level Seven (HL7) and Fast Healthcare Interoperability Resources (FHIR) are standards that facilitate the electronic exchange of healthcare information. Incorporating HL7/FHIR interoperability ensures that different healthcare systems can communicate effectively.
Advantages:
- Seamless Data Exchange: Enables real-time sharing of patient information across various platforms.
- Improved Patient Care: Facilitates coordinated care by providing comprehensive patient data to healthcare providers.
- Scalability: Supports integration with new systems and technologies as they emerge.
Adopting HL7/FHIR standards is vital for creating a connected and efficient healthcare ecosystem.
3. HIPAA/GDPR Compliance Tools
What compliance tools are necessary for healthcare automation systems?
Healthcare automation systems must adhere to regulations like the Health Insurance Portability and Accountability Act (HIPAA) in the U.S. and the General Data Protection Regulation (GDPR) in the EU. Compliance tools ensure that systems handle PHI responsibly.
Key Features:
- Data Encryption: Protects data at rest and in transit.
- Audit Trails: Maintains logs of data access and modifications.
- Access Controls: Restricts data access based on user roles.
- Consent Management: Tracks patient consent for data usage.
Integrating these tools helps organizations avoid legal penalties and maintain patient trust.
4. Low-Latency Processing and Real-Time Alerts
Why is low-latency processing important in healthcare automation?
In healthcare, timely data processing can be critical. Low-latency systems ensure that information is processed and delivered with minimal delay, which is essential for real-time decision-making.
Benefits:
- Immediate Response: Enables prompt action in emergencies, such as alerting staff to critical patient vitals.
- Enhanced Monitoring: Supports continuous patient monitoring with instant data updates.
- Operational Efficiency: Reduces delays in administrative processes like billing and scheduling.
Implementing low-latency processing is crucial for both clinical and administrative functions in healthcare.
5. Integration-Ready APIs
How do integration-ready APIs benefit healthcare automation systems?
Application Programming Interfaces (APIs) allow different software systems to communicate and share data. Integration-ready APIs enable healthcare automation systems to connect seamlessly with other platforms.
Advantages:
- Flexibility: Facilitates the addition of new functionalities without overhauling existing systems.
- Data Consistency: Ensures uniform data across various platforms.
- Improved Workflow: Streamlines processes by enabling systems to work together efficiently.
APIs are essential for building adaptable and interoperable healthcare solutions.
6. Custom Workflow Builders
What is the role of custom workflow builders in healthcare automation?
Custom workflow builders allow organizations to design and implement processes tailored to their specific needs without extensive coding.
Features:
- Drag-and-Drop Interfaces: Simplify the creation of workflows.
- Conditional Logic: Enables complex decision-making paths.
- Integration Capabilities: Connects with other systems to automate tasks.
These tools empower healthcare providers to optimize operations and adapt quickly to changing requirements.
7. Analytics and Automation Audit Logs
Why are analytics and audit logs important in healthcare automation systems?
Analytics provide insights into system performance and patient outcomes, while audit logs track system activities for security and compliance purposes.
Benefits:
- Performance Monitoring: Identifies areas for improvement in processes and care delivery.
- Compliance Assurance: Maintains records required for regulatory audits.
- Security: Detects unauthorized access or anomalies in system usage.
Incorporating robust analytics and audit logging capabilities is essential for maintaining high standards of care and operational integrity.
By integrating these core features, healthcare automation systems can enhance patient care, ensure compliance, and improve operational efficiency.
Technology Stack for Building Healthcare Automation Solutions
Selecting the appropriate healthcare technology stack is crucial for developing robust, secure, and scalable healthcare automation solutions. The stack should support interoperability, comply with healthcare regulations, and facilitate rapid development and deployment. Below is a detailed breakdown of the recommended technology components across various layers of the application.
-
Backend Technologies
The backend forms the core of healthcare automation systems, handling data processing, business logic, and integration with other services.
- Node.js: An event-driven JavaScript runtime ideal for building scalable network applications. Its non-blocking I/O model makes it suitable for real-time applications.
- Python (FastAPI): FastAPI is a modern, high-performance web framework for building APIs with Python 3.6+ based on standard Python type hints. It’s known for its speed and automatic interactive API documentation.
- .NET Core: A cross-platform, high-performance framework for building modern, cloud-based, and internet-connected applications. It’s particularly useful for enterprises already invested in the Microsoft ecosystem.
-
Frontend Technologies
The frontend is responsible for delivering a seamless user experience, which is critical in healthcare applications where usability can impact patient outcomes.
- React: A JavaScript library for building user interfaces, particularly single-page applications where data changes over time. React’s component-based architecture promotes reusability and maintainability.
- Angular: A TypeScript-based open-source web application framework led by the Angular Team at Google. It offers a comprehensive solution with built-in tools for routing, state management, and form validation.
-
AI and Machine Learning Layer
Integrating AI capabilities enhances the intelligence of healthcare automation systems, enabling features like predictive analytics and natural language processing.
- Large Language Models (LLMs): Models like OpenAI’s GPT and Anthropic’s Claude can be utilized for tasks such as summarizing patient records, generating clinical documentation, and providing conversational interfaces.
- LangChain: A framework for developing applications powered by language models. It facilitates the integration of LLMs with external data sources and APIs.
- DSPy: A library designed for building and deploying data science pipelines, which can be instrumental in processing and analyzing healthcare data.
-
Middleware and Messaging
Middleware facilitates communication between different parts of the application, ensuring data consistency and enabling asynchronous processing.
- Kafka: A distributed event streaming platform capable of handling trillions of events a day. It’s useful for real-time data pipelines and streaming applications.
- Redis: An in-memory data structure store used as a database, cache, and message broker. It’s known for its speed and support for various data structures.
-
Databases
Choosing the right database is essential for storing and retrieving healthcare data efficiently and securely.
- PostgreSQL: An open-source relational database known for its robustness and support for advanced data types and performance optimization features.
- MongoDB: A NoSQL database that stores data in flexible, JSON-like documents. It’s suitable for applications requiring scalability and rapid development.
- Healthcare-Specific Data Lakes: These are centralized repositories that allow storage of structured and unstructured data at scale. They support advanced analytics and machine learning workloads.
-
Cloud Platforms
Cloud platforms offer scalable infrastructure and services tailored for healthcare applications, ensuring compliance with industry regulations.
- Azure for Healthcare: Provides a suite of tools and services designed to meet the needs of healthcare organizations, including compliance with HIPAA and other regulations.
- AWS HealthLake: A service that enables healthcare providers to store, transform, and query health data in the cloud. It uses machine learning to understand and extract meaningful information from unstructured data.
- Google Cloud Healthcare API: Offers a managed solution for storing and accessing healthcare data in Google Cloud, supporting standards like HL7 and FHIR.
-
Integration and Interoperability
Ensuring seamless integration with existing systems and adherence to healthcare data standards is vital.
- HL7/FHIR Standards: Implementing these standards ensures interoperability between different healthcare systems, facilitating the exchange of electronic health records.
- Role-Based Access Control (RBAC): Implementing RBAC ensures that users have access only to the information necessary for their roles, enhancing security and compliance.
-
Security and Compliance
Healthcare applications must comply with regulations like HIPAA and GDPR to protect patient data.
- Data Encryption: Both at rest and in transit, to prevent unauthorized access.
- Audit Logging: Maintaining logs of data access and changes to monitor for suspicious activities and ensure accountability.
- Consent Management: Tools to manage patient consent for data usage, ensuring compliance with privacy laws.
-
DevOps and Deployment
Efficient deployment and maintenance practices are essential for the reliability of healthcare automation systems.
- Docker and Kubernetes: Containerization and orchestration tools that facilitate scalable and manageable deployments.
- CI/CD Pipelines: Continuous Integration and Continuous Deployment pipelines automate testing and deployment, reducing errors and accelerating release cycles.
By carefully selecting and integrating these technologies, healthcare organizations can build automation solutions that are secure, compliant, and capable of improving patient care and operational efficiency.
Integration with Existing Healthcare Systems
One of the most critical success factors in any healthcare automation project is the ability to integrate seamlessly with existing clinical and operational systems. Hospitals and clinics typically operate a patchwork of software tools—EHRs, PACS, RIS, LIS, billing systems, and proprietary applications—each of which stores valuable patient data. Building automation software that works with these systems, rather than against them, is essential for clinical safety, regulatory compliance, and operational continuity.
This raises a common and important question from technical teams and clinical leaders alike: “How do you integrate automation tools with EHR systems and other healthcare platforms?”
The answer lies in understanding both the systems in place and the standards that govern their communication. Below, we break down how automation tools can effectively integrate across the healthcare IT stack.
-
EHR/EMR Integration: Epic, Cerner, Meditech
EHRs (Electronic Health Records) or EMRs (Electronic Medical Records) are at the heart of most healthcare IT ecosystems. Leading platforms like Epic, Cerner (now Oracle Health), and Meditech offer APIs, integration modules, and partner ecosystems that automation software can leverage.
Common Integration Points:
- Clinical documentation modules: automation tools can augment physician notes using NLP or LLMs.
- Appointment and scheduling systems: auto-schedule follow-ups or send reminders.
- Orders and referrals: generate lab or imaging orders based on clinical logic.
- FHIR APIs and HL7 interfaces: enable real-time data exchange and event notifications.
For example, automation software that analyzes patient discharge readiness can write directly to an Epic encounter record using a FHIR-compliant API, updating care plans in real time.
Implementation Considerations:
- Epic uses HL7v2 interfaces, Smart on FHIR apps, and the “App Orchard” marketplace.
- Cerner supports RESTful FHIR APIs via its Ignite platform.
- Meditech offers Web Services APIs and supports Mirth or Cloverleaf for HL7 integration.
Automation tools should be certified, sandbox-tested, and approved via the vendor’s partner program if working with EHRs in a production environment.
-
PACS and RIS Integration for Imaging Workflows
Picture Archiving and Communication Systems (PACS) and Radiology Information Systems (RIS) handle imaging workflows like X-rays, MRIs, CTs, and their associated reports. For automation tools that need to retrieve or analyze imaging studies (e.g., using AI for diagnostics or prioritization), DICOM protocol compliance is essential.
Integration Capabilities:
- DICOM Query/Retrieve (C-FIND/C-MOVE) to access image metadata or full image sets
- HL7 ORM/ORU messages to receive orders and send back results
- Integration with reporting systems to pre-fill structured findings based on AI interpretation
Automation tools can plug into PACS viewers to suggest annotations, flag abnormal scans, or even generate pre-diagnostic notes. These tools often sit in the radiologist’s workflow, integrated via DICOM routers or vendor-neutral archives (VNAs).
-
Laboratory Information System (LIS) Integration
Laboratory Information Systems manage diagnostic testing, results entry, and sample tracking. Automation tools that work on lab turnaround time (TAT), results triage, or quality control often require LIS integration.
Data Flows Typically Automated:
- Auto-order generation based on EHR rules
- Automated lab result flagging and alerts
- Pre-auth checks for send-out labs
- Specimen logistics and courier dispatch workflows
LIS integration typically happens via HL7 ORM (Order) and ORU (Observation Result) messages, or through custom middleware that bridges LIS to EHR and automation layers.
-
HL7, FHIR, and DICOM Protocols: The Foundation of Interoperability
At the heart of healthcare integration are three critical standards:
- HL7 v2/v3: Used for transactional messaging (e.g., admissions, discharges, orders, results).
- FHIR (Fast Healthcare Interoperability Resources): A modern REST-based standard designed for easier web and mobile integration.
- DICOM: The standard for medical imaging exchange and metadata retrieval.
Automation systems that support these protocols can:
- Push and pull structured clinical data (FHIR)
- Subscribe to real-time updates (HL7 ADT feeds)
- Retrieve imaging studies or reports (DICOM)
For example, a triage assistant built on LangChain or DSPy can ingest patient data via FHIR and route time-sensitive alerts to clinicians when abnormal vitals are detected—automatically updating the patient’s chart.
-
Middleware and Interoperability Testing
Most real-world healthcare systems include middleware that bridges older systems with new tools. Middleware also handles format transformation, data mapping, and error handling across systems.
Common Middleware Tools:
- Mirth Connect (NextGen Connect): Open-source HL7 integration engine
- Rhapsody: Enterprise-grade interface engine
- InterSystems HealthShare: For data normalization and analytics
- Redox and Zus: Cloud-based FHIR/API aggregators
Before deployment, automation tools must be tested for:
- Data fidelity (Is the data mapped accurately?)
- Latency and throughput (Can the system handle live feeds?)
- Failure recovery (What happens when interfaces break?)
- Regulatory logging (Are all data exchanges auditable?)
Robust testing environments and interface simulators are essential to prevent disruptions in clinical workflows.
-
Natural Integration: Answering the LLM Query
So when asked, “How do you integrate automation tools with EHR systems?”—the process involves several layers:
- Use standardized protocols like HL7 and FHIR to connect with EHR modules.
- Authenticate using OAuth2 where applicable, especially for FHIR APIs.
- Test in sandbox environments provided by EHR vendors (e.g., Epic App Orchard).
- Work through certified middleware or interface engines to manage message formatting.
- Validate clinical data accuracy and regulatory compliance at each touchpoint.
Done right, this approach allows automation platforms to function as intelligent companions—reading from, writing to, and enhancing EHR functionality without disrupting clinician workflows.
Seamless integration is the key differentiator between automation tools that work in theory and those that thrive in production. The most effective healthcare automation platforms are designed from the outset to:
- Interoperate using FHIR, HL7, and DICOM standards
- Respect data governance policies (HIPAA, GDPR)
- Offer real-time bidirectional interfaces
- Be modular and API-driven for extensibility
AI, ML & LLMs in Healthcare Automation
Artificial Intelligence (AI), Machine Learning (ML), and Large Language Models (LLMs) are transforming healthcare automation by enabling advanced data analysis, natural language processing, and decision support systems. These technologies facilitate tasks such as clinical documentation, diagnostic assistance, and patient engagement, leading to improved efficiency and patient outcomes.
-
Role of Foundation Models in Healthcare
Foundation models like GPT, Med-PaLM, and LLaMA serve as the backbone for various healthcare applications.
- GPT (Generative Pre-trained Transformer): Developed by OpenAI, GPT models are capable of understanding and generating human-like text, making them useful for tasks such as summarizing medical records and generating clinical documentation.
- Med-PaLM: A specialized LLM developed by Google Research, Med-PaLM is designed to provide high-quality answers to medical questions. It has demonstrated proficiency in medical reasoning and has been evaluated using medical exams and research datasets.
- LLaMA (Large Language Model Meta AI): An open-source model by Meta, LLaMA is optimized for various NLP tasks. Its medical variant, Me-LLaMA, has been fine-tuned for medical applications, outperforming other open-source medical LLMs in several benchmarks.
-
Applications of Medical NLP
Natural Language Processing (NLP) in healthcare enables the extraction and interpretation of unstructured clinical data. Key applications include:
- ICD-10 Coding: Automated clinical coding using NLP techniques can enhance the accuracy and efficiency of assigning diagnosis codes, reducing the burden on medical coders.
- Summarization: NLP models can generate concise summaries of lengthy clinical notes, aiding in quick information retrieval and decision-making.
- Triage: AI-powered triage systems can analyze patient symptoms described in natural language and prioritize care based on urgency.
-
Training Custom LLMs with Healthcare Datasets
Customizing LLMs for healthcare involves fine-tuning them on domain-specific datasets to improve performance on medical tasks. Steps include:
- Data Collection: Gathering diverse and representative healthcare data, such as clinical notes, EHRs, and medical literature.
- Data Preprocessing: Cleaning and structuring data to ensure quality and relevance.
- Model Fine-Tuning: Adjusting pre-trained LLMs using the prepared dataset to specialize them for healthcare applications.
- Evaluation: Assessing model performance using relevant metrics and benchmarks.
Platforms like Protege assist in acquiring and managing healthcare data for AI model training.
-
Data Privacy Techniques: Anonymization and Federated Learning
Ensuring patient data privacy is paramount in healthcare AI applications. Techniques include:
- Anonymization: Removing or encrypting personally identifiable information (PII) from datasets to prevent patient identification.
- Federated Learning: A decentralized approach where models are trained across multiple institutions without sharing raw data, preserving privacy while enabling collaborative learning.
-
AI Hallucination Risks and Mitigation
AI hallucination refers to instances where models generate plausible but incorrect information. In healthcare, this can lead to misinformation and potential harm. Mitigation strategies include:
- Model Validation: Rigorous testing of AI outputs against trusted medical sources.
- Human Oversight: Involving healthcare professionals in reviewing AI-generated content.
- Continuous Monitoring: Implementing systems to detect and correct inaccuracies in real-time.
Addressing hallucination is critical to maintaining trust and safety in AI-driven healthcare applications.
Can ChatGPT be used in hospitals?
ChatGPT can be utilized in hospitals for tasks like administrative assistance, patient communication, and preliminary information gathering. However, its deployment should be accompanied by strict oversight to ensure accuracy and compliance with healthcare regulations.
How are LLMs used in medical software?
LLMs are integrated into medical software to enhance functionalities such as clinical decision support, documentation automation, and patient engagement tools. Their ability to process and generate human-like text makes them valuable in interpreting complex medical data and facilitating communication.
By leveraging AI, ML, and LLMs thoughtfully and responsibly, healthcare organizations can significantly enhance automation capabilities, leading to improved patient care and operational efficiency.
Security, Compliance & Privacy Considerations
In the realm of healthcare automation, ensuring the security, compliance, and privacy of patient data is paramount. With the increasing integration of AI and digital tools, adhering to regulatory standards and implementing robust security measures is essential to protect sensitive health information.
Regulatory Frameworks: HIPAA, HITECH, GDPR, and Regional Equivalents
Healthcare organizations must navigate a complex landscape of regulations designed to safeguard patient data:
- HIPAA (Health Insurance Portability and Accountability Act): In the U.S., HIPAA sets national standards for the protection of electronic protected health information (ePHI). The Security Rule within HIPAA mandates administrative, physical, and technical safeguards to ensure the confidentiality, integrity, and security of ePHI.
- HITECH (Health Information Technology for Economic and Clinical Health Act): This act promotes the adoption of health information technology and strengthens HIPAA rules by increasing penalties for non-compliance and emphasizing the importance of breach notifications.
- GDPR (General Data Protection Regulation): Applicable in the European Union, GDPR governs the processing of personal data, including health information, emphasizing data subject rights and imposing strict consent requirements.
Other regions have their own regulations, such as Australia’s Privacy Act and Canada’s Personal Information Protection and Electronic Documents Act (PIPEDA), which set standards for data protection in healthcare.
Secure Handling of Protected Health Information (PHI)
Ensuring the secure handling of PHI involves implementing measures that protect data both at rest and in transit:
- Data Encryption: Encrypting data using standards like AES-256 ensures that ePHI remains unreadable to unauthorized individuals.
- Secure Transmission Protocols: Utilizing protocols such as TLS (Transport Layer Security) protects data during transmission across networks.
- Access Controls: Implementing role-based access controls ensures that only authorized personnel can access specific data, minimizing the risk of unauthorized disclosures.
- Regular Security Audits: Conducting periodic audits helps identify vulnerabilities and ensures that security measures are effective and up to date.
Audit Trails and Access Controls
Maintaining detailed audit trails is crucial for monitoring access to ePHI and detecting potential security incidents:
- Audit Logs: Recording user activities, including logins, data access, and modifications, provides a comprehensive trail for compliance and forensic analysis.
- Monitoring Systems: Implementing real-time monitoring systems can alert administrators to suspicious activities, enabling prompt responses to potential breaches.
- User Authentication: Employing multi-factor authentication adds an extra layer of security, ensuring that only verified users can access sensitive information.
Cybersecurity Best Practices
Adopting a proactive approach to cybersecurity involves implementing best practices that protect against evolving threats:
- Zero Trust Architecture: This model operates on the principle of “never trust, always verify,” requiring continuous authentication and authorization for all users and devices.
- Endpoint Hardening: Securing endpoints through measures like regular patching, antivirus software, and device encryption reduces the attack surface for potential threats.
- Employee Training: Educating staff on cybersecurity awareness, including recognizing phishing attempts and proper data handling procedures, is vital for maintaining a secure environment.
- Incident Response Plans: Developing and regularly updating incident response plans ensures that organizations can respond swiftly and effectively to security breaches.
Certification and Regulatory Approval
Obtaining relevant certifications and approvals demonstrates a commitment to security and compliance:
- FDA Approval: In the U.S., the Food and Drug Administration (FDA) regulates certain medical devices and software, requiring approval to ensure safety and effectiveness.
- CE Marking: In the European Economic Area, the CE mark indicates that a product complies with EU safety, health, and environmental protection requirements.
- SOC 2 Certification: This certification assesses the controls relevant to security, availability, processing integrity, confidentiality, and privacy of a system.
- ISO 27001: An international standard for information security management systems, ISO 27001 provides a framework for managing sensitive company and customer information.
Is AI healthcare software HIPAA-compliant?
AI healthcare software can be HIPAA-compliant if it incorporates necessary safeguards, including data encryption, access controls, and audit logging. Compliance also involves ensuring that any third-party vendors handling ePHI adhere to HIPAA regulations through Business Associate Agreements (BAAs).
What security measures are needed for health apps?
Health apps must implement robust security measures to protect user data, including:
- Data Encryption: Protecting data both at rest and in transit.
- User Authentication: Employing strong authentication methods, such as multi-factor authentication.
- Regular Updates and Patching: Keeping software up to date to address known vulnerabilities.
- Privacy Policies: Clearly communicating how user data is collected, used, and protected.
- Compliance with Regulations: Adhering to relevant laws and standards, such as HIPAA, GDPR, and others applicable in the region of operation.
By prioritizing security, compliance, and privacy considerations, healthcare organizations can build trust with patients and stakeholders while leveraging automation to enhance care delivery.
Cost Structure and Budgeting Guide
Implementing healthcare automation software involves a multifaceted budgeting process that accounts for various components, including development, integration, compliance, and ongoing maintenance. Understanding these cost drivers is essential for effective financial planning and decision-making.
MVP vs. Full-Suite Automation Platform
The cost of developing a healthcare automation solution varies significantly based on the project’s scope:
- Minimum Viable Product (MVP): An MVP with basic features such as appointment scheduling or simple data processing can cost between $8,000 and $15,000.
- Full-Suite Automation Platform: A comprehensive platform integrating advanced AI capabilities, interoperability with existing systems, and compliance features can range from $100,000 to over $1,000,000, depending on complexity and scale.
Key Cost Drivers
Several factors influence the overall cost of healthcare automation software:
- System Integrations: Connecting with Electronic Health Records (EHRs), Laboratory Information Systems (LIS), and other existing platforms requires custom interfaces and middleware, which can add $10,000 to $35,000 to the project.
- AI Implementation: Incorporating AI functionalities, such as natural language processing or predictive analytics, can cost between $50,000 and $500,000, depending on the sophistication of the models and the volume of data processed.
- Compliance and Security: Ensuring adherence to regulations like HIPAA and GDPR involves implementing robust security measures, auditing capabilities, and data encryption, which can add $20,000 to $100,000 to the budget.
- Cloud Infrastructure: Utilizing cloud services for hosting and scalability can reduce infrastructure costs by 40-60% compared to on-premises solutions.
Total Cost of Ownership (TCO): Build vs. Buy
When considering the development of healthcare automation software, organizations must evaluate the total cost of ownership:
- Building In-House: Developing a custom solution offers flexibility but requires significant investment in development, testing, and maintenance. Long-term costs include staffing, training, and ongoing updates.
- Purchasing Off-the-Shelf: Buying a ready-made solution can reduce initial costs and deployment time but may involve recurring licensing fees and limited customization options.
A hybrid approach, combining off-the-shelf components with custom development, can balance cost and flexibility.
Open-Source vs. Proprietary Solutions
Choosing between open-source and proprietary software impacts both upfront and long-term costs:
- Open-Source: These solutions often have lower initial costs and offer flexibility but may require more in-house expertise for customization and support. The total cost of ownership can be higher if extensive modifications are needed.
- Proprietary: Commercial solutions typically come with vendor support and regular updates, reducing the burden on internal teams. However, they involve licensing fees and may have limitations on customization.
Example Budgets by Organization Size
Budget requirements vary based on the size and needs of the healthcare organization:
- Small Clinic: Implementing basic automation features like appointment scheduling and billing can cost between $20,000 and $65,000.
- Mid-Sized Hospital: A more comprehensive solution with EHR integration and advanced features may require a budget of $65,000 to $200,000.
- Large Hospital Network: Developing a full-suite automation platform with AI capabilities and extensive integrations can exceed $200,000, potentially reaching $650,000 or more.
How much does healthcare automation software cost?
The cost of healthcare automation software varies widely based on the project’s scope, ranging from $8,000 for a basic healthcare MVP to over $1,000,000 for a comprehensive platform. Key factors influencing cost include system integrations, AI implementation, compliance requirements, and infrastructure choices.
By carefully assessing these factors and aligning them with organizational goals, healthcare providers can develop a realistic budget for automation initiatives, ensuring both financial feasibility and the successful implementation of technology solutions.
Development Workflow & Best Practices
Developing healthcare automation software requires a meticulous approach that balances innovation with compliance, security, and user-centric design. This section outlines a structured workflow and best practices to guide teams through the development process effectively.
Discovery and Compliance Scoping
The initial phase involves understanding the specific needs of the healthcare organization and the regulatory landscape:
- Stakeholder Interviews: Engage with clinicians, administrators, and IT personnel to gather requirements and identify pain points.
- Regulatory Assessment: Determine applicable regulations such as HIPAA, GDPR, and regional healthcare laws to ensure compliance from the outset.
- Workflow Analysis: Map existing processes to identify opportunities for automation and areas requiring integration with current systems.
Design with Clinician and Admin Feedback Loops
Incorporating feedback from end-users is crucial for developing intuitive and effective solutions:
- Prototyping: Develop wireframes and mock-ups to visualize the user interface and gather early feedback.
- Usability Testing: Conduct sessions with clinicians and administrative staff to assess the ease of use and functionality of the prototypes.
- Iterative Refinement: Use the insights gained to refine the design, ensuring it aligns with user expectations and workflows.
Agile Sprints and User Testing Cycles
Adopting an agile methodology facilitates flexibility and continuous improvement:
- Sprint Planning: Define clear objectives and deliverables for each sprint, typically lasting 2-4 weeks.
- Daily Stand-Ups: Hold brief meetings to synchronize team efforts and address any impediments promptly.
- Sprint Reviews and Retrospectives: At the end of each sprint, review progress with stakeholders and reflect on improvements for future sprints.
User Acceptance Testing (UAT) with Compliance Validation
Before deployment, it’s essential to validate the software’s functionality and compliance:
- Test Case Development: Create comprehensive test cases that cover all functional requirements and compliance scenarios.
- Execution and Documentation: Perform the tests, document the results, and address any issues identified.
- Regulatory Approval: Ensure that the software meets all regulatory requirements and obtain necessary certifications or approvals.
DevOps, CI/CD, and Rollback Protocols
Implementing DevOps practices enhances collaboration and accelerates delivery:
- Continuous Integration/Continuous Deployment (CI/CD): Automate the building, testing, and deployment processes to ensure rapid and reliable releases.
- Infrastructure as Code (IaC): Manage infrastructure through code to enable consistent and repeatable deployments.
- Monitoring and Logging: Implement robust monitoring to detect issues early and maintain logs for auditing and troubleshooting.
- Rollback Mechanisms: Establish procedures to revert to previous versions in case of deployment failures or critical issues.
What’s the process to build healthcare automation software?
Building healthcare automation software involves a structured approach:
- Requirement Gathering: Engage stakeholders to understand needs and regulatory requirements.
- Design and Prototyping: Develop user-centric designs with iterative feedback.
- Agile Development: Implement features in sprints, allowing for flexibility and continuous improvement.
- Testing and Validation: Conduct thorough testing, including UAT and compliance checks.
- Deployment and Monitoring: Use DevOps practices for deployment and establish monitoring for ongoing performance and compliance.
By following these best practices, healthcare organizations can develop automation software that is effective, compliant, and aligned with user needs, ultimately enhancing patient care and operational efficiency.
Case Studies: Real-World Implementations
Healthcare automation is no longer a theoretical concept; it’s actively transforming patient care, administrative efficiency, and clinical workflows across the globe. This section presents real-world case studies, illustrating the tangible benefits of automation in diverse healthcare settings.
U.S. Hospital System: Automating Prior Authorizations
Prior authorization processes have traditionally been a bottleneck in U.S. healthcare, leading to delays in patient care and increased administrative burdens. A notable example is MultiCare Connected Care’s collaboration with Regence and MCG Health to automate prior authorizations using HL7 FHIR interoperability standards.
Implementation Highlights:
- Workflow Analysis: Mapping existing authorization processes to identify automation opportunities.
- RPA Development: Configuring bots to interact with forms, websites, and internal systems.
- Dashboard Creation: Providing visibility into authorization status, exceptions, and key metrics.
Impact on KPIs:
- Turnaround Time: Reduced from 5 days to 2 days.
- Denial Rate: Decreased from 8% to 2% due to improved accuracy and consistency.
This automation not only expedited patient access to necessary treatments but also alleviated the administrative load on healthcare providers.
Indian Diagnostic Chain: AI-Based Appointment Bots
In India, the integration of AI-powered chatbots has revolutionized patient engagement and appointment scheduling. Diagnostic chains have implemented symptom bots that provide preliminary assessments, bridging the gap between patients and doctors.
Implementation Highlights:
- Symptom Assessment: Bots conduct initial evaluations based on patient inputs.
- Appointment Scheduling: Automated booking of appointments with appropriate specialists.
Impact on KPIs:
- Operational Efficiency: Significant reduction in manual scheduling efforts.
- Patient Wait Times: Decreased due to streamlined appointment processes.
These AI-driven solutions have enhanced patient experience by providing timely and accurate information, leading to better healthcare outcomes.
Challenges, Pitfalls & How to Avoid Them
Implementing healthcare automation software offers significant benefits, but it also presents various challenges that can hinder success. Understanding these pitfalls and adopting strategies to mitigate them is crucial for effective deployment.
1. Resistance from Medical Staff
Healthcare professionals may resist automation due to concerns about job security, changes in workflow, and unfamiliarity with new technologies. This resistance can impede the adoption of automation solutions.
Mitigation Strategies:
- Engage Stakeholders Early: Involve medical staff in the planning and implementation phases to address concerns and gather input.
- Provide Comprehensive Training: Offer training sessions to familiarize staff with new systems and demonstrate their benefits.
- Highlight Benefits: Emphasize how automation can reduce administrative burdens, allowing staff to focus more on patient care.
2. Data Silos and Legacy System Dependencies
Many healthcare organizations operate with fragmented systems that do not communicate effectively, leading to data silos. These silos hinder the seamless flow of information, affecting decision-making and patient care.
Mitigation Strategies:
- Adopt Interoperability Standards: Implement standards like HL7 and FHIR to facilitate data exchange between systems.
- Invest in Integration Solutions: Utilize middleware and APIs to bridge gaps between legacy systems and new technologies.
- Plan for Gradual Modernization: Develop a roadmap to update or replace outdated systems incrementally.
3. Lack of Clinical Validation for AI Modules
Deploying AI modules without thorough clinical validation can lead to inaccurate results, potentially compromising patient safety.
Mitigation Strategies:
- Conduct Rigorous Testing: Validate AI algorithms using diverse and representative datasets.
- Collaborate with Clinicians: Involve healthcare professionals in the development and evaluation of AI tools to ensure clinical relevance.
- Implement Continuous Monitoring: Regularly assess AI performance and update models as needed to maintain accuracy.
4. Vendor Lock-In and Poor Documentation
Relying heavily on a single vendor can limit flexibility and make future transitions challenging. Additionally, inadequate documentation can hinder system understanding and maintenance.
Mitigation Strategies:
- Choose Open Standards: Select solutions that support open standards and interoperability to reduce dependency on a single vendor.
- Negotiate Clear Contracts: Ensure contracts include provisions for data portability and access to necessary documentation.
- Maintain Comprehensive Documentation: Develop and regularly update internal documentation to support system understanding and continuity.
Why do healthcare automation projects fail?
Healthcare automation projects can fail due to factors such as resistance from medical staff, data silos, lack of clinical validation for AI modules, and vendor lock-in. Addressing these challenges through stakeholder engagement, adopting interoperability standards, rigorous testing, and careful vendor selection can enhance the likelihood of successful implementation.
Future Outlook: 2025–2030
The next five years will bring major changes to healthcare automation, driven by improvements in artificial intelligence (AI), interoperability standards, and connected medical devices. The focus will shift from automating isolated tasks to building deeply integrated systems that support clinical decisions, monitor patient conditions continuously, and connect previously siloed workflows.
-
LLM-Powered Agents as Clinical Aides
Large Language Models (LLMs) such as GPT-4, Med-PaLM, and LLaMA are being integrated into clinical environments. These models can review patient records, highlight relevant clinical information, and generate summaries to assist physicians during consultations. Some tools already support physicians by transcribing and organizing clinical notes during patient visits, reducing time spent on documentation.
LLM-based assistants are also being tested for use in medical education, decision support, and patient triage. When paired with structured patient data, LLMs can help identify medication conflicts, flag incomplete histories, or generate diagnostic differentials for physician review.
-
Predictive Diagnostics and Autonomous Workflows
Machine learning models trained on large datasets are being deployed to identify early signs of disease. For example, models trained on EHR data can predict the risk of sepsis, stroke, or cardiac events before symptoms become severe. These predictions are now being integrated into clinician alert systems.
Outside of clinical diagnostics, autonomous task workflows are being implemented for routine tasks such as patient follow-ups, lab result notifications, and claim validation. Once rules or models are set, these systems can operate independently, reducing delays and errors in administrative processes.
-
IoMT (Internet of Medical Things) Integrations
Medical devices that transmit data in real time are increasingly common in both hospital and home settings. Blood glucose monitors, ECG patches, blood pressure cuffs, and sleep trackers are now connected to mobile apps or clinical dashboards.
When integrated with automation software, this device data can be used to schedule interventions, alert care teams to changes in patient status, or initiate remote check-ins. For instance, a connected blood pressure monitor might detect persistent hypertension and trigger a teleconsultation workflow without manual input from the patient.
The clinical value of these devices depends on how well the data can be ingested, validated, and acted upon within clinical systems. Automation software plays a central role in processing these continuous data streams and routing relevant information to the appropriate care teams.
-
Standards Adoption: TEFCA, SMART on FHIR, CDS Hooks
Wider adoption of national and international data standards is expected to improve integration between automation tools and existing health IT infrastructure.
- TEFCA (Trusted Exchange Framework and Common Agreement) aims to make it possible for healthcare organizations in the U.S. to share patient data securely and consistently across state lines and institutional boundaries.
- SMART on FHIR allows third-party apps to access and write back to EHRs using standardized APIs. Many EHR vendors now support SMART on FHIR natively, which enables modular automation features to be deployed without complex integrations.
- CDS Hooks allow automation tools to surface clinical decision support content at critical points in the care workflow. For example, during medication prescribing, a CDS Hook might alert a physician if a safer alternative exists based on a patient’s allergy profile or recent lab results.
Adoption of these standards will reduce the time and cost required to integrate automation tools into production healthcare environments.
What is the future of healthcare automation?
From 2025 to 2030, healthcare automation will move toward intelligent systems that support decision-making, reduce manual intervention, and act on real-time data from clinical and patient-owned devices. LLMs will assist clinicians during consultations, not replace them. Diagnostic models will support earlier detection of critical illness. Automation will be integrated into everyday tools through standard APIs and frameworks, rather than added on after the fact.
Hospitals and clinics that invest in modular, standards-based platforms will be best positioned to adopt new automation tools without costly rework. Automation will no longer be limited to administrative efficiency. It will directly support clinical quality, safety, and timeliness of care.
Final Words
Healthcare automation is no longer an abstract concept or a future objective. It is a practical and increasingly essential solution for improving care delivery, reducing manual workload, and addressing systemic inefficiencies across clinical and administrative operations.
As this guide has demonstrated, the scope of healthcare automation is broad and fast-maturing. From clinical documentation assistants and AI-based diagnostics to automated prior authorizations and LLM-powered triage chatbots, organizations around the world are already benefiting from targeted investments in automation.
Yet success in this domain depends on more than just selecting the right technology. It requires a strong foundation in compliance, a user-centric development approach, and a long-term commitment to integration and maintenance. Healthcare systems must balance innovation with safety, interoperability with privacy, and efficiency with clinical rigor.
What to Keep in Focus
-
Automation is not a replacement for clinical judgment. It’s a support layer that enhances accuracy, reduces delay, and frees clinicians to focus on care quality.
-
Standards like HL7, FHIR, SMART, and TEFCA are not optional. They’re foundational for interoperability and long-term platform relevance.
-
LLMs and AI models can reduce documentation time, assist in diagnosis, and improve engagement—but only when implemented with rigorous validation and proper oversight.
-
Cybersecurity, compliance with HIPAA or GDPR, and audit readiness are non-negotiable requirements for any automation deployment.
The question most healthcare leaders are asking now is not “should we automate?” but “where do we begin, and who should we work with?”
Moving Forward with Confidence
Whether you represent a private clinic, a multi-hospital network, or a health tech startup, automation is likely to be central to your digital strategy in the next five years. Starting with high-impact, low-risk use cases like patient scheduling, claims processing, or AI-assisted triage is often the most effective path.
Aalpha Information Systems can help you define and execute a customized roadmap tailored to your clinical goals, compliance needs, and infrastructure. With over two decades of experience in building healthcare software for global clients, our team brings both technical depth and real-world healthcare insight to every engagement.
The future of healthcare will be defined by those who automate thoughtfully, build securely, and integrate intelligently. Let this guide serve as your blueprint to do just that.
Call to Action: Partner With Aalpha Information Systems
Aalpha Information Systems specializes in custom healthcare software development with a proven track record in building secure, scalable, and interoperable automation platforms. From early-stage discovery to post-deployment support, we work closely with hospitals, clinics, and health tech startups across the U.S., Europe, and Asia.
Contact Aalpha to discuss your healthcare automation initiative. We’ll help you assess technical feasibility, define a cost-effective roadmap, and build a solution that meets clinical needs and regulatory standards.