Healthcare workforce management has evolved from a largely administrative task into one of the most strategic capabilities in modern hospitals, clinics, and health systems. As care delivery becomes more complex and patient expectations rise, healthcare leaders are asking how they can staff efficiently, maintain compliance, prevent burnout, and still deliver safe, timely, high-quality care. Workforce management software answers this by bringing structure, automation, and real-time intelligence to one of the most resource-intensive components of healthcare operations: managing people. In environments where staff shortages, unpredictable patient volumes, and regulatory scrutiny are constant realities, workforce technology is emerging as a foundational pillar of clinical governance, financial sustainability, and operational excellence.
Why healthcare workforce management is becoming mission-critical
Health systems operate under unique constraints where staffing decisions directly influence patient outcomes. The workforce represents the largest cost center for most hospitals, often exceeding 50 percent of operating expenses, yet it also defines the quality of care delivered at the bedside. Poor workforce planning can lead to delayed interventions, medication errors, increased wait times, and breaches of mandated staffing ratios. On the other hand, effective workforce management strengthens care continuity, ensures appropriate clinical coverage, and allows administrators to align labor supply with patient demand. The shift toward value-based care models has further increased scrutiny on staffing patterns, making it essential for organizations to adopt technology that provides transparency, forecasting, and decision support.
The staffing crisis: nurse shortages, clinician burnout, overtime escalation
Healthcare systems worldwide face persistent staffing gaps driven by aging populations, growing chronic disease burdens, and retirement among experienced clinicians. The World Health Organization projects a global shortfall of more than 10 million health workers by 2030, a trend already visible in daily hospital operations. These shortages force remaining staff to shoulder additional workloads, often resulting in mandatory overtime, frequent shift changes, and chronic fatigue. Burnout among nurses and physicians has surged, with studies in outlets such as JAMA Network Open documenting links between excessive workloads and compromised patient safety. Hospitals increasingly rely on travel nurses or agency contractors to fill critical gaps, inflating labor costs. Workforce management software helps organizations confront this crisis by enabling more equitable scheduling, identifying staffing deficits early, and reducing unnecessary overtime through intelligent allocation of available staff.
Rising demand for scheduling automation and real-time staffing intelligence
Traditional scheduling methods — spreadsheets, whiteboards, phone calls, and messaging apps — cannot keep pace with today’s dynamic staffing environment. Patient census levels fluctuate by hour, emergency cases appear unexpectedly, and clinical skill requirements shift based on acuity levels. As leaders seek operational resilience, organizations are adopting automated scheduling engines that apply predefined rules, labor laws, credential restrictions, and fatigue thresholds to produce optimized staffing rosters. Real-time dashboards help supervisors monitor attendance, manage call-outs, and redeploy staff where they are needed most. Hospitals increasingly ask how to forecast tomorrow’s staffing needs, predict absenteeism, or simulate the impact of a surge in patient admissions. Intelligent workforce systems answer these questions by combining historical data, live patient volumes, staffing ratios, and analytics to deliver fast, data-driven decisions.
How workforce technologies impact patient safety, compliance, and operational cost
Healthcare organizations operate under strict regulatory frameworks that govern staffing levels, nurse-to-patient ratios, overtime policies, and credential validity. Non-compliance can result in penalties, accreditation risks, and compromised patient safety. Workforce management platforms provide automated rule enforcement by preventing schedules that violate clinical labor laws or place unqualified staff in specialized units. They support clinical safety by ensuring that the right skill mix is present at the bedside and that staff workloads are balanced across shifts. From a financial perspective, automation reduces unnecessary overtime, enhances float pool utilization, and minimizes reliance on costly temporary staff. Analytics dashboards give administrators visibility into labor spending patterns, enabling proactive cost control and better resource planning. These improvements help hospitals maintain both regulatory compliance and financial stability.
How software improves continuity of care and clinical outcomes
Continuity of care is strengthened when the workforce is aligned, prepared, and consistently available. Workforce management software ensures that staffing levels match patient needs at all times, reducing delays in care and supporting safer clinical handovers. By documenting qualifications, tracking licensure, and maintaining up-to-date competence profiles, the system ensures that staff assigned to units possess the appropriate clinical expertise. Automation minimizes last-minute scheduling disruptions, empowering nurses and physicians to focus on patient care rather than administrative coordination. Research consistently shows that adequately staffed units experience lower rates of adverse events, hospital-acquired conditions, and readmissions. As hospitals move toward predictive operations, workforce management systems help integrate staffing decisions into broader clinical and operational strategies, improving outcomes across the continuum of care.
What Is Healthcare Workforce Management Software?
Healthcare workforce management software is a purpose-built digital system that helps hospitals, clinics, and long-term care organizations manage staffing, scheduling, resource allocation, attendance, and compliance with precision. Unlike generic workforce tools, healthcare-focused platforms are engineered around the realities of clinical care: fluctuating patient volumes, skill-dependent task assignments, strict regulatory requirements, and the need to align staffing levels with patient acuity at all times. As health systems scale and clinical complexity increases, these platforms provide the operational backbone that connects clinicians, administrators, HR teams, and department supervisors in a single, unified workflow. They transform what was once a manual, reactive process into a data-driven capability that supports safe, efficient, and continuous care delivery.
Definition and core purpose
At its core, healthcare workforce management software is a platform designed to plan, schedule, track, and optimize the activities of a healthcare organization’s staff. It centralizes shift planning, credential management, attendance tracking, communication, and labor analytics into an integrated system used by various stakeholders across the hospital. The platform’s primary purpose is to ensure the right staff member is in the right place at the right time while also maintaining regulatory compliance and minimizing operational waste. It supports strategic and daily decision-making through predictive insights, real-time analytics, and automated workflows that reduce manual effort and improve accuracy. By leveraging structured rules, workforce data, and intelligent algorithms, the software helps healthcare organizations maintain staffing stability while promoting staff well-being and patient safety.
How workforce management differs in healthcare vs general industries
Workforce management in healthcare is fundamentally more complex than in industries such as retail, hospitality, or manufacturing. Healthcare staffing is governed by strict clinical, legal, and safety requirements that influence every scheduling decision. Unlike general sectors where a shift can often be filled by any available worker, clinical environments require a specific skill mix, credential validity, and experience level based on patient conditions. Nurse-to-patient ratios must be maintained, specialized units require staff with dedicated certifications, and operational demand can vary dramatically within hours based on emergencies or case surges. Additionally, the consequences of improper staffing extend beyond productivity loss; they directly affect patient outcomes, safety events, and clinical compliance. General workforce management systems prioritize efficiency, whereas healthcare workforce systems must balance efficiency with clinical appropriateness, regulatory accuracy, and patient-care integrity. This distinction shapes every aspect of system design, from scheduling logic to audit trails.
Essential outcomes: productivity, shift visibility, cost control, staffing quality
The primary outcomes of healthcare workforce management software revolve around operational excellence, cost management, and improved clinical staffing quality. Productivity increases when staff schedules are optimized based on real workloads, reducing idle time, excessive overtime, and last-minute shift changes. Shift visibility improves through centralized dashboards that show who is available, who is on leave, and which units require reinforcement. This visibility helps supervisors allocate staff across departments, avoid coverage gaps, and redeploy float pools effectively. Cost control is achieved when the system reduces unplanned overtime, monitors labor spending in real time, and decreases dependency on expensive agency staff. Staffing quality improves as the platform ensures that only qualified, credentialed professionals are assigned to units that match their competencies. Additional benefits include reduced burnout, clearer communication, and higher staff satisfaction due to predictable schedules and fewer conflicts.
Key users: HR teams, nursing supervisors, department heads, hospital admin
Healthcare workforce management platforms support diverse users, each interacting with the system to fulfill specific responsibilities. HR teams use it to manage attendance, leave balances, payroll integration, credential verification, and employee records. Nursing supervisors rely on it to assign staff to patient units, handle last-minute absences, approve shift swaps, and maintain compliance with staffing rules. Department heads use the system to monitor resource availability, analyze productivity metrics, and request additional staffing when needed. Hospital administrators depend on the platform to analyze labor costs, evaluate staffing efficiency, plan budgets, and understand workforce trends at a strategic level. Frontline clinicians interact with the mobile interface to view schedules, request leave, swap shifts, and receive urgent notifications. Together, these stakeholders ensure that staffing decisions reflect operational priorities and patient-care requirements across the organization.
Standard system architecture: modules, data infrastructure, interoperability needs
Healthcare workforce management software typically follows a modular architecture, allowing organizations to adopt core functionalities and extend capabilities as needed. Common modules include scheduling engines, attendance tracking, credentialing, labor analytics, payroll integration, and mobile communication interfaces. The backend architecture usually involves a secure relational or hybrid database where staff profiles, shift data, labor rules, and compliance documents are stored. Modern systems rely on cloud-native infrastructures to ensure scalability, redundancy, and real-time data access. Interoperability is essential in healthcare, where workforce tools must exchange data with EHR systems, HRMS platforms, payroll providers, telehealth applications, and hospital information systems. Standards such as HL7, FHIR, and secure REST APIs enable reliable data flow between platforms, ensuring staffing decisions are informed by real clinical and operational metrics. Audit logs, access controls, and encryption layers support healthcare-grade privacy and security requirements. This architecture allows the software to operate as a unified, reliable command center for managing the clinical workforce.
Why Healthcare Organizations Need Workforce Management Tools
Modern healthcare systems operate in a high-stakes environment where staffing decisions directly influence clinical outcomes, operational stability, and financial performance. Hospitals and clinics face the dual pressure of increasing patient volumes and a shrinking talent pool, all while compliance expectations and care standards continue to tighten. Traditional manual methods of scheduling and workforce coordination are no longer capable of supporting the complexity of today’s clinical workflows. Workforce management tools address these challenges by providing automation, real-time intelligence, and structured processes that enable healthcare leaders to deploy staff efficiently and safely. They allow organizations to align the workforce with demand, balance workloads, and maintain the continuity of care essential to a functioning clinical ecosystem.
-
Solving understaffing and overstaffing
Understaffing is one of the most persistent problems in healthcare, frequently resulting in delayed care, increased patient wait times, and avoidable safety events. When units are short-staffed, clinicians struggle to maintain quality standards, often juggling too many tasks at once. Workforce management tools help prevent this by forecasting demand using historical census data, acuity trends, and patterns in patient flow. These systems identify staffing gaps early, enabling supervisors to redeploy float pool nurses or request additional support before the situation escalates. Overstaffing presents an opposite but equally problematic challenge, driving unnecessary labor costs without improving patient outcomes. Automated scheduling engines detect redundancies by mapping actual patient volumes against planned shifts, ensuring labor allocation aligns with real operational needs. This balance helps hospitals maintain safe coverage levels while controlling labor expenditure.
-
Reducing clinician burnout, absenteeism, and turnover
The healthcare sector faces high rates of burnout and turnover, particularly among nurses, emergency physicians, and frontline clinical staff. Long hours, frequent night shifts, excessive workload, and unpredictable scheduling contribute to exhaustion and emotional fatigue. Workforce management software combats this by creating fair, transparent schedules that distribute workload evenly and respect rest requirements. Automated rule enforcement ensures no individual clinician is assigned an unsafe number of consecutive shifts or high-acuity workloads without adequate recovery time. Real-time attendance and absence tracking allow supervisors to identify early signs of fatigue, such as frequent call-outs or patterns of lateness. When staff feel supported by predictable schedules and equitable workload distribution, absenteeism declines and retention improves. Studies in Health Affairs and The Lancet have shown that organizations with structured scheduling and clear workload policies experience lower burnout and reduced turnover, resulting in more stable clinical teams.
-
Optimizing skill mix, shift coverage, and float pool utilization
Healthcare staffing is not simply about filling a shift; it requires precision in matching the right skill sets to the unique needs of each patient care unit. A general medical ward has different expertise requirements compared to an ICU, emergency department, maternity ward, or oncology unit. Workforce management tools maintain a full competency profile for each staff member, allowing scheduling engines to ensure only qualified individuals are assigned to specialized roles. This ensures compliance with clinical standards and reduces the risk of care delays or safety issues caused by deploying inexperienced personnel. Float pools, often underutilized due to poor visibility of real-time needs, become strategic assets. The system helps supervisors identify units requiring immediate reinforcement and assigns float staff where they can add the most value. Efficient float pool utilization also helps reduce unnecessary external agency hires, which can be expensive and disruptive to care continuity.
-
Meeting compliance: labor laws, clinical staffing ratios, credential requirements
Compliance in healthcare is non-negotiable. Nurse-to-patient ratios, labor law restrictions, mandatory breaks, and overtime ceilings are enforced at the state, national, and institutional levels. Violations can lead to legal penalties, accreditation risks, union disputes, and compromised patient safety. Workforce management systems embed these rules into automated scheduling logic, preventing supervisors from creating shifts that violate these constraints. The system also tracks licensing, certifications, and credential expirations, ensuring that only fully compliant personnel are deployed. Automated alerts notify administrators before key certifications lapse, reducing the risk of unqualified staff being assigned to regulated units. This compliance infrastructure protects organizations from regulatory exposure while maintaining high standards of clinical governance.
-
Reducing operational costs through AI-driven scheduling
Labor is the largest expense for most hospitals, often accounting for more than half of total operating costs. Inefficient scheduling, excessive overtime, and reliance on agency staff can quickly inflate budgets. AI-enhanced workforce management systems use predictive analytics to optimize staffing levels by analyzing trends in patient admissions, seasonal fluctuations, and unit-level workload patterns. These models generate optimized rosters that minimize unnecessary overtime and reduce the need for last-minute temp workers. Cost dashboards give administrators real-time visibility into labor spending and highlight units operating above budget thresholds. Predictive forecasting helps leadership plan staffing strategies months in advance, aligning financial planning with clinical demand. Over time, these optimizations support sustainable cost management without compromising care quality.
-
Ensuring consistent patient care quality and safety
Appropriate staffing is directly linked to patient outcomes. Research shows that understaffed units have higher rates of medication errors, pressure injuries, falls, and hospital-acquired infections. Workforce management systems support consistent care quality by ensuring that each shift has the correct number of clinicians and the right composition of experience and skill. When emergencies arise, supervisors can quickly locate qualified personnel through real-time staff availability dashboards. Automated communication tools deliver urgent notifications and mobilize backup teams within minutes. Ensuring predictable and safe staffing levels also improves clinician concentration, decision-making accuracy, and overall care coordination. Strong workforce management helps create a stable clinical environment that reduces variability in care delivery and maintains patient trust.
-
Replacing spreadsheets, WhatsApp scheduling, and manual workflows
Many hospitals still rely on spreadsheets, emails, WhatsApp groups, and whiteboards to manage shift schedules. These methods are error-prone, time-consuming, and incapable of supporting real-time decision-making. They often result in duplication, conflicting updates, and significant administrative overhead. Workforce management tools eliminate these inefficiencies by centralizing all scheduling, attendance, and communication workflows into a secure, unified platform. Staff can access schedules on mobile apps, request swaps, and receive updates instantly, reducing confusion and preventing miscommunication. Supervisors gain automated rule enforcement, streamlined approvals, and full visibility into staffing status. By replacing fragmented manual processes, organizations free up administrative time, reduce scheduling disputes, and operate with greater agility and accuracy.
Core Features of Healthcare Workforce Management Software
Healthcare workforce management systems are engineered to handle the full spectrum of staffing, scheduling, compliance, communication, and operational needs of hospitals and clinical organizations. They function as the central cockpit from which administrators, nursing supervisors, HR teams, and department heads gain precise control over their workforce. The features described below represent the backbone of a modern, scalable, and clinically aligned workforce platform. Collectively, these capabilities streamline daily operations, improve clinical safety, and give decision-makers the intelligence required to run a resilient healthcare workforce.
Staff Scheduling and Shift Planning
Scheduling is the core function of workforce management, and healthcare requires exceptional precision due to clinical skills, staffing ratio laws, patient acuity variations, and 24×7 operations. Modern platforms automate these tasks with intelligent engines that handle complex rules and real-time changes.
-
Automated shift allocation
Automated scheduling engines use predefined rules, labor laws, operational constraints, and availability preferences to build optimized rosters. Instead of supervisors manually assembling shifts through spreadsheets or WhatsApp messages, the system analyzes staffing needs, clinician competencies, and prior workloads to create schedules that are balanced and compliant. It reduces manual errors, eliminates scheduling bias, and saves hours of administrative time each week. Automation also allows for scenario simulation, where administrators can quickly model outcomes such as holiday staffing, sudden census increases, or staffing shortages.
-
Rotation rules, fatigue management, skill mix requirements
Healthcare staffing requires strict rotation management to prevent overburdening staff with consecutive nights, extended shifts, or high-intensity unit assignments. Fatigue is linked to safety events, medication errors, and impaired judgment, making it a critical parameter. Workforce systems enforce fatigue thresholds by automatically blocking shift assignments that violate rest-hour requirements or consecutive shift limits. Skill mix enforcement ensures each unit receives the correct balance of registered nurses, specialists, assistants, and technicians. The software matches staff capabilities with unit requirements, ensuring that specialized units like ICU, NICU, or emergency departments are staffed only with qualified personnel.
-
Nurse staffing ratios and acuity-based scheduling
Mandatory nurse-to-patient ratios in regions such as California, Australia, and parts of Europe require precise control. Workforce management tools embed these ratios into rules that automatically prevent schedules from falling below legal thresholds. Beyond ratios, modern systems incorporate patient acuity data to determine staffing levels. For example, a unit with multiple high-acuity patients may require additional nurses even if census numbers remain constant. Integration with EHRs allows patient acuity scores to influence scheduling in near real time. This supports equitable workloads, reduces stress on clinicians, and ensures patient safety.
Time and Attendance Tracking
Time and attendance modules ensure accurate logging of hours worked, reduce time fraud, and automate payroll inputs. Healthcare’s complex shift structures and round-the-clock operations require flexible tools that support multiple entry methods.
-
Biometric check-in, geo-fencing, location tagging
Biometric authentication using fingerprint, facial recognition, or palm scanning prevents buddy punching and ensures reliable attendance data. Geo-fencing, particularly for home-health and community-care staff, enables check-ins only when the individual is physically present at the approved care location. Location tagging helps supervisors verify time accuracy and ensure safe deployment of field workers.
-
Integration with mobile devices and kiosks
Many hospitals deploy mobile check-ins via smartphones, allowing clinicians to clock in and out through secure apps. Kiosks or wall-mounted tablets serve shared areas like nurse stations, enabling quick access even during shift rush hours. The system syncs attendance data across devices, ensuring consistency and reliability.
-
Overtime calculation and absence tracking
Automated calculation of overtime, double time, and holiday premiums ensures payroll accuracy. The platform tracks leaves, sickness, and unscheduled absences in real time, helping supervisors respond quickly to fill critical gaps. Absence trends also provide insight into early signs of burnout or chronic fatigue among staff.
Credentialing and Compliance Management
Compliance is central to healthcare operations. Workforce systems act as a real-time source of truth for clinical qualifications, certifications, and labor law adherence.
-
License verification, certifications, CME tracking
Hospitals must ensure staff carry valid licenses and clinical certifications at all times. The platform stores all credential documents, validates expiration dates, and allows supervisors to assign shifts based on verified competencies. For physicians and specialists, the system tracks Continuing Medical Education (CME) requirements and renewal cycles.
-
Automated reminders for expirations
Automated notifications alert clinicians and HR teams when licenses or certifications are nearing expiration. This reduces administrative burden and avoids compliance breaches where staff may be mistakenly assigned to specialized units without valid credentials.
-
Regulatory compliance reporting
Compliance dashboards provide evidence for audits, accreditation reviews, and regulatory inspections. The system generates reports on staffing ratios, overtime trends, break compliance, and credential validity, supporting accountability and reducing legal exposure.
Labor Analytics and Forecasting
Workforce analytics transform raw data into actionable intelligence, helping hospitals plan effectively.
-
Hourly, daily, weekly workload forecasts
Forecasting models analyze historical patient census, typical seasonal demand patterns, appointment logs, and service-line data to predict staffing needs. These insights allow supervisors to adjust shifts proactively instead of reacting to last-minute crises.
-
Predictive analytics using patient census and acuity trends
Advanced analytics integrate EHR data to track patient acuity, admission trends, and discharge patterns. By understanding when demand surges are likely, hospitals can mobilize staff early, reducing operational disruptions. For example, predictive data might indicate an expected rise in emergency department visits during winter months, enabling more precise labor planning.
-
Department-level productivity insights
Analytics tools help administrators compare metrics across departments — such as hours per patient day, overtime spending, absenteeism, and productivity benchmarks. This supports cost control, identifies high-performing units, and highlights areas requiring additional staffing or process refinement.
Mobile Workforce Tools
Mobile functionality gives clinicians and staff immediate access to schedules, notifications, and communication tools.
-
Shift swap requests
Clinicians can request shift swaps directly through mobile apps. The system ensures swaps comply with credential rules and labor regulations before presenting them for supervisor approval, reducing manual coordination and minimizing errors.
-
Real-time push notifications
Schedules, updates, unit changes, emergency staffing requests, and corporate announcements are instantly communicated. Real-time notifications reduce delays and ensure critical messages reach the right people.
-
Team broadcast, emergency staffing alerts
Supervisors can send broadcast messages during crises, such as unexpected surges in patient volume. Emergency staffing alerts mobilize float pools or on-call teams within minutes, improving response time and patient care readiness.
Payroll and HR System Integrations
Integration with payroll and HR systems eliminates manual data entry and improves accuracy.
-
Payroll exports and validations
Attendance data flows directly into payroll software, reducing reconciliation time. The system highlights inconsistencies such as missing punch-ins or unexplained overtime, ensuring accurate processing.
-
Syncing PTO, overtime, allowances
Paid time off (PTO), shift differentials, bonuses, overtime premiums, and night allowances sync automatically. This ensures the financial implications of staffing decisions are always reflected accurately.
-
ERP and HRMS connectors
The platform integrates with ERP solutions (SAP, Oracle), HRMS systems (Workday, BambooHR), and even custom tools used by large healthcare chains. This centralized integration strengthens data consistency across the organization.
Telehealth Workforce Scheduling
As telemedicine becomes mainstream, organizations must schedule virtual care staff alongside on-site clinicians.
-
Managing remote doctors, virtual care shifts
Telehealth requires precise coordination across time zones, specialties, and availability windows. Workforce tools allow virtual physicians, counselors, and specialists to be scheduled seamlessly with full visibility into workload and appointment volume.
-
Managing skill match and availability for teleconsults
The system ensures the appropriate specialist is available for specific teleconsultation types. For example, a diabetes educator may be needed for chronic care follow-ups, while a dermatologist handles image-based assessments. This matching improves patient satisfaction and clinical efficiency.
Security, Privacy, and Access Control
Healthcare data is sensitive, and workforce systems must meet rigorous security standards.
-
HIPAA, GDPR, SOC-2 alignment
Compliance with global privacy frameworks protects patient-related workforce data and limits access to sensitive staff information. Security controls ensure data confidentiality, integrity, and availability.
-
Role-based permissions
Access rights are assigned based on job roles. HR teams view credential documents; supervisors see scheduling dashboards; clinicians access only their own schedules. This minimizes risk and prevents unauthorized data access.
-
Secure audit trails
Every action — schedule updates, credential changes, approvals, overrides — is recorded in tamper-proof logs. Audit trails are essential for forensic investigations, compliance audits, and internal reviews.
Advanced AI Capabilities in Workforce Management
Artificial intelligence is transforming workforce management from a reactive administrative function into a proactive, intelligence-driven discipline. Healthcare organizations now deal with fluctuating patient volumes, unpredictable absences, tight staffing ratios, and growing clinical complexity. Traditional scheduling systems can no longer keep pace with these dynamic demands. AI enhances workforce management by forecasting staffing needs, automating scheduling decisions, detecting fatigue and burnout patterns, and offering real-time decision support powered by large language models (LLMs) and retrieval-augmented generation (RAG). These capabilities create a workforce ecosystem that is not only efficient, but continuously learning from hospital operations to improve accuracy, resilience, and care quality.
-
AI-based predictive scheduling
Predictive scheduling is one of the most impactful AI capabilities in healthcare workforce management. AI models analyze years of historical data — patient census levels, admission trends, seasonal surges, discharge patterns, emergency spikes, and even environmental factors such as flu season — to forecast staffing needs days, weeks, or months in advance. Instead of relying on manual guesswork, organizations gain visibility into exactly how many nurses, technicians, or physicians will be needed for upcoming shifts. Predictive scheduling aligns staffing supply with forecasted demand, reducing last-minute scrambles and eliminating operational blind spots. When integrated with patient acuity scores from EHR systems, the model accurately determines whether additional high-skill clinicians are required, enabling safer workloads and better clinical outcomes. This predictive intelligence also minimizes overstaffing, helping organizations maintain financial discipline without compromising care.
-
LLM-powered workforce copilots for supervisors
Large language models are emerging as powerful copilots for hospital staffing supervisors. Instead of navigating multiple dashboards, reports, and approval workflows, supervisors can ask the system direct, conversational questions such as: “Which units are at risk of understaffing tonight?” or “Show me all ICU nurses with trauma certification available tomorrow morning.” The LLM interprets these requests, retrieves relevant data from workforce systems, and presents actionable insights within seconds. Copilots assist with schedule reviews, policy clarifications, and compliance checks. They can also draft staffing memos, explain scheduling decisions, and summarize weekly workforce performance. By reducing administrative complexity, LLM copilots allow supervisory teams to focus on strategic staff management, leadership communication, and supporting frontline clinicians.
-
Intelligent float pool allocation using ML
Float pools are often essential for handling surges in patient volume, emergency scenarios, or sudden call-outs, yet many hospitals struggle to deploy float staff efficiently. Machine learning models analyze real-time demand signals such as census spikes, acuity shifts, and attendance patterns to determine where float staff can have the greatest impact. Instead of deploying float nurses reactively or on a first-come basis, the system uses predictive logic to assign them where their skills match the most urgent needs. ML-driven float pool allocation improves utilization, reduces operational bottlenecks, and ensures specialized units receive timely reinforcement. Over time, the model learns from historical patterns to refine its allocation strategies and predict which departments will need float support before shortages occur.
-
Natural language interfaces for scheduling tasks
Natural language interfaces make staffing management more intuitive, especially in high-pressure clinical environments. Supervisors can issue commands such as: “Schedule two additional RNs for the emergency department evening shift,” or “Approve all pending shift swaps for Ward B.” The AI parses these instructions, checks constraints, validates compliance rules, and executes scheduling changes without requiring manual navigation through screens and forms. Clinicians can also benefit from natural language interactions via mobile apps, enabling them to request time off, swap shifts, or check upcoming assignments using simple conversational prompts. This reduces friction, enhances user experience, and ensures timely staffing responses.
-
NLP to identify burnout risk and absence patterns
Natural language processing provides powerful insights into workforce well-being by analyzing patterns that may indicate burnout or chronic fatigue. The system examines attendance records, lateness trends, overtime frequency, sick leave clusters, and staff communication sentiment (where permitted) to detect early warning signs. If a staff member shows repeated last-minute call-outs or consistently logs excessive overtime, the system might flag them as at risk for burnout. Supervisors receive proactive alerts recommending interventions such as schedule adjustments, additional rest days, or well-being check-ins. This analytical capability supports a healthier workforce, reduces turnover, and strengthens long-term staffing stability.
-
RAG-powered decision support for staffing policy updates
Retrieval-augmented generation enhances decision-making by combining LLM reasoning with real institutional data. RAG allows healthcare leaders to ask sophisticated operational questions such as: “How will implementing a two-hour break rule affect weekend staffing patterns?” or “What were the outcomes the last time we increased ICU staffing ratios?” The system retrieves relevant data — past schedules, policy documents, patient safety metrics, and performance reports — and synthesizes them into accurate, context-rich insights. Instead of relying solely on managerial judgment, decision-makers gain access to historical evidence and predictive modeling, supporting more consistent and transparent staffing policy decisions. RAG also helps administrators understand regulatory changes by summarizing labor laws or credentialing requirements and linking them to existing internal practices.
-
Scenario simulation: “What if census increases by 15 percent?”
AI-powered scenario modeling allows administrators to test staffing decisions before applying them. Hospitals can simulate events such as a sudden 15 percent increase in patient census, a holiday-weekend staffing dip, or the introduction of a new clinical service line. The system calculates how these scenarios would affect staffing needs, overtime costs, float pool availability, and labor compliance. It can highlight units most vulnerable to shortages and propose optimal staffing adjustments. Scenario simulation is particularly valuable in emergency planning, pandemic response, seasonal surges, and multi-site hospital operations. By providing clear projections, the system empowers leaders to prepare early and allocate resources more strategically.
-
AI-driven workforce optimization engines
Workforce optimization engines combine forecasting, machine learning, and real-time analytics to create the most efficient staffing model possible. They evaluate variables such as skill mix, shift preferences, labor laws, cost constraints, overtime limits, department policies, and patient acuity. The engine then generates recommended schedules that minimize cost while maximizing safety and compliance. As the system ingests new data — call-outs, census changes, emergency cases — it re-optimizes schedules instantly. Advanced optimization engines can also recommend long-term strategies, such as adjusting staff hiring levels, expanding the float pool, or redistributing full-time and part-time positions based on projected demand. These engines essentially act as the decision-making core of the workforce system, orchestrating thousands of daily variables to maintain operational stability.
Compliance and Regulatory Requirements in Workforce Management
Healthcare workforce management operates under some of the most stringent regulatory requirements across any industry. A hospital’s ability to deliver safe and effective care is inseparable from how it manages staffing levels, clinician qualifications, labor law compliance, and documentation frameworks mandated by accreditation bodies. Unlike general enterprise environments, where scheduling errors may lead to productivity loss or minor operational inefficiencies, workforce-related non-compliance in healthcare can directly compromise patient safety, expose organizations to litigation, threaten accreditation status, and deteriorate care quality. As a result, workforce management software must be designed to enforce these requirements automatically, eliminating human error and bringing consistency to staffing decisions across all departments. The sections below outline the key regulatory domains healthcare organizations must satisfy and how workforce systems support ongoing compliance.
-
Nurse staffing ratio laws
Nurse staffing ratio laws mandate the minimum number of nurses required per patient in specific clinical settings. These regulations vary across regions; for example, California enforces explicit ratios such as 1:2 for ICU and 1:4 for medical-surgical units, while other jurisdictions define staffing requirements through acuity-based frameworks. Understaffing is not merely a policy issue; research demonstrates that higher nurse workloads correlate with increased mortality, adverse events, and extended hospital stays. Workforce management systems embed ratio rules directly into scheduling engines, preventing supervisors from finalizing rosters that violate legal thresholds. When census or acuity increases, the system flags non-compliant assignments and recommends corrective action. Real-time census integration allows the software to automatically adjust staffing projections, making it easier for hospitals to remain compliant during fluctuating patient volumes or emergency surges.
-
Labor law constraints: breaks, overtime, rest hours
Labor laws govern multiple elements of workforce management, including mandatory breaks, maximum shift durations, consecutive working hour limitations, and rules surrounding overtime pay. In healthcare, these regulations protect staff from fatigue-induced errors and ensure safe work environments. Workforce systems track each clinician’s hours in real time, blocking schedule assignments that would infringe on rest-hour requirements or exceed legally allowed overtime. Automatic alerts notify supervisors when a clinician is nearing overtime thresholds or when a schedule would violate break mandates. This proactive monitoring is essential during high-pressure periods such as night shifts or emergency department surges. By aligning scheduling practices with statutory labor protections, workforce platforms minimize legal exposure and support healthier staffing models.
-
HIPAA requirements for workforce data
Workforce management platforms contain sensitive information about clinicians, including personal identifiers, license details, work history, and potentially clinical assignment data that may be connected to patient activity. Under the Health Insurance Portability and Accountability Act (HIPAA), healthcare institutions must safeguard this information with strict access controls, encryption, and secure data governance practices. Workforce software enforces role-based permissions, ensuring that only authorized individuals can view or modify workforce data. Every action taken within the system is logged through audit trails to maintain accountability. Data in transit and at rest must be encrypted to prevent unauthorized exposure, especially when accessed via mobile apps or remote work environments. HIPAA-aligned workforce systems help organizations maintain data confidentiality, integrity, and availability while enabling operational efficiency.
-
Clinical credentialing and licensure
Credentialing and licensure are essential pillars of workforce compliance. Hospitals must ensure that every clinician is qualified, trained, and certified to perform their designated duties. This includes tracking nursing licenses, physician board certifications, Advanced Cardiac Life Support (ACLS) training, pediatric certifications, and specialized unit competencies such as neonatal or trauma care. Manual tracking introduces significant risk, especially in large organizations with thousands of staff. Workforce management platforms automate this process by storing digital credentials, verifying expiration dates, and issuing alerts well before renewals are due. When a certification expires, the system automatically restricts the clinician from being assigned to units requiring that competency. This prevents compliance breaches and protects the hospital from deploying unqualified staff in critical areas. As hospitals expand advanced practice roles to address staffing gaps, credentials such as those earned through AGACNP online programs increase the importance of accurate licensure and role-based assignment within workforce management systems.
-
JCI and NABH workforce documentation standards
Accreditation frameworks such as Joint Commission International (JCI) and the National Accreditation Board for Hospitals & Healthcare Providers (NABH) require comprehensive workforce documentation and evidence of safe staffing practices. These standards include maintaining competency records, documenting training programs, tracking performance evaluations, ensuring adherence to staffing plans, and auditing compliance with staffing policies. Workforce management systems streamline these requirements by serving as a centralized repository for staff qualifications, training logs, appraisal history, and scheduling data. The software generates audit-ready reports that demonstrate compliance during accreditation assessments. By linking staffing decisions to documented evidence, the platform strengthens hospital governance and supports smooth accreditation renewal cycles.
-
Union rules and contract requirements
In many regions, labor unions play a significant role in shaping healthcare workforce policies. Collective bargaining agreements define rules around shift assignments, overtime distribution, seniority-based prioritization, floating policies, workload expectations, and dispute resolution procedures. Workforce software must incorporate all applicable union rules into the scheduling engine to ensure compliance with contractual obligations. For example, if a union contract mandates that overtime must be offered first to staff with the most seniority before agency workers can be deployed, the system must enforce this sequence automatically. When unions impose limits on floating staff between departments, the platform must reflect these constraints to avoid grievances. By operationalizing union agreements within the software, organizations reduce conflict, maintain trust with labor groups, and avoid penalties stemming from contractual violations.
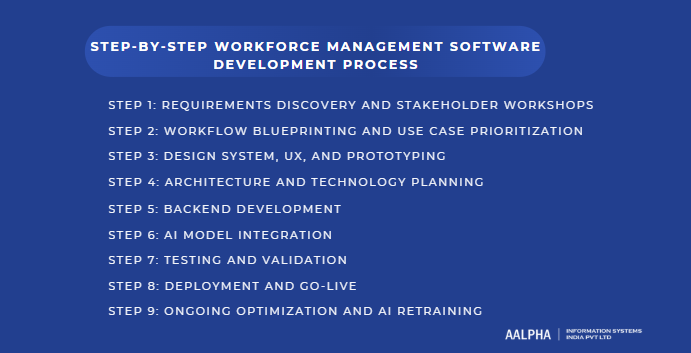
Step-by-Step Workforce Management Software Development Process
Building healthcare workforce management software requires a methodical, evidence-based development approach that accounts for clinical complexity, compliance obligations, and diverse user needs. Unlike general HR or scheduling platforms, healthcare systems must incorporate patient acuity, clinical competency rules, legal staffing ratios, multi-department coordination, and real-time operational decision-making. The process outlined below provides a comprehensive framework that aligns technical execution with strategic clinical priorities to ensure the final product is safe, reliable, scalable, and aligned with hospital workflows.
Step 1: Requirements Discovery and Stakeholder Workshops
The development process begins with structured discovery sessions aimed at understanding operational pain points, compliance gaps, staff needs, and departmental workflows. Healthcare organizations have highly specialized environments — ICU, emergency departments, surgical units, telehealth teams, and administrative offices each operate under different demands. Stakeholder workshops allow development teams to map these nuances before building the product.
- Pain point mapping for HR, nursing, admin
HR teams face challenges such as manual attendance tracking, inefficient payroll reconciliation, and credential management complexity. Nursing supervisors struggle with last-minute shift changes, understaffing, skill mix imbalances, and compliance with mandatory staffing ratios. Administrators require real-time visibility into labor costs, staffing adequacy, and departmental performance. Developers must document each pain point, categorize it by priority and business impact, and determine how software can automate or improve these workflows. This mapping ensures the system addresses real operational bottlenecks rather than simply replicating outdated methods in digital form.
Step 2: Workflow Blueprinting and Use Case Prioritization
Once pain points are mapped, teams create detailed workflow blueprints that illustrate how staffing, scheduling, credentialing, communication, and reporting processes currently operate. These blueprints highlight inefficiencies and help design the future-state workflows that the software will support.
- End-to-end staffing workflows
End-to-end workflows typically include forecasting staffing demand, creating schedules, managing attendance, handling call-outs, reallocating float staff, approving overtime, tracking credentials, communicating shift changes, and generating compliance reports. Each process is broken down step by step to define user roles, required data inputs, dependencies, and system triggers. Developers then prioritize use cases by grouping them into “must-have,” “should-have,” and “future enhancements,” ensuring critical clinical workflows are addressed in early development cycles. This prioritization prevents scope creep and enables hospitals to adopt the platform in phases without overwhelming users.
Step 3: Design System, UX, and Prototyping
Healthcare workforce management software must be intuitive and accessible, especially for busy clinicians and supervisors operating under pressure. The design system focuses on clarity, efficiency, and minimal cognitive load.
- Supervisor dashboards
Dashboards for supervisors serve as real-time control centers showing staffing levels, overtime risks, absence alerts, credential expirations, and unit-level workload. Designers create prototypes that prioritize color-coded indicators, intuitive navigation, and customizable widgets. Supervisors should be able to view staffing adequacy for every shift, identify shortages instantly, and act within a few clicks. Early prototyping helps validate information hierarchy and ensures critical insights surface without overwhelming the user.
- Nurse mobile app journeys
Nurses and frontline clinicians rely heavily on mobile access. Prototypes for nurse-facing apps must enable staff to check upcoming shifts, request time off, swap shifts, clock in, and receive notifications with minimal steps. Journeys are designed to accommodate real-world clinical constraints, including glove use, limited time between tasks, or situations where mobile access must be extremely fast. Wireframes are tested with real nurses to validate usability and refine interaction flows.
Step 4: Architecture and Technology Planning
After the design system is validated, the technical architecture is defined to support scalability, interoperability, and compliance.
- APIs, database, microservices
The architecture typically consists of:
- Microservices for scheduling, attendance, credentialing, AI models, notifications, and reporting.
- A secure SQL or hybrid database storing staff profiles, shift data, attendance logs, compliance documents, and operational metrics.
- REST or GraphQL APIs enabling integration with EHR systems, HRMS platforms, payroll providers, telehealth systems, and biometric devices.
- Event-driven pipelines for real-time attendance updates and alert processing.
The architecture must support role-based access, audit logs, encryption, and redundancy to meet healthcare regulations.
Step 5: Backend Development
Backend development transforms the architectural blueprint into functional modules.
- Scheduling engine, attendance engine, compliance logic
- Scheduling engine: Incorporates staffing ratios, skill mix requirements, fatigue rules, and individual preferences. It must generate optimized rosters and re-optimize during real-time disruptions.
- Attendance engine: Handles biometric check-ins, geo-fencing, mobile clock-ins, overtime calculation, and absence tracking. It syncs with kiosks, RFID systems, and staff mobile apps.
- Compliance logic: Embeds labor laws, break requirements, credential constraints, and union rules. It blocks illegal schedules and flags violations.
Backend modules must be thoroughly tested to prevent clinical safety risks from incorrect logic or algorithm errors.
Step 6: AI Model Integration
AI capabilities elevate workforce management from reactive scheduling to proactive decision support.
- Census forecasting models
These models use historical admissions, seasonal trends, emergency patterns, and EHR acuity scores to predict hourly, daily, and weekly staffing needs. Forecasting helps supervisors prepare for surges, avoid understaffing, and allocate resources efficiently.
- Auto-scheduling ML models
Machine learning models generate optimized schedules by evaluating skill mix, clinician availability, cost parameters, union rules, and fatigue indicators. Over time, they learn patterns such as typical call-out periods or peak workload times, improving scheduling accuracy. AI integration requires close collaboration between data scientists, clinicians, and HR teams to ensure predictions align with clinical realities.
Step 7: Testing and Validation
Testing is critical because even small software errors can disrupt clinical operations or trigger compliance violations.
- Load testing, shift conflict validation
Load testing ensures the platform performs under peak usage conditions, such as shift changes or large hospitals with thousands of staff logging in simultaneously. Conflict validation checks for errors in the scheduling engine, such as double assignments, illegal overtime, invalid credentials, or ratio violations. This prevents scheduling errors from reaching production environments.
- HIPAA security audits
Security testing includes penetration tests, vulnerability scans, and compliance audits aligned with HIPAA, GDPR, and SOC-2 requirements. Encryption validation, access control checks, and secure logging are evaluated. These audits ensure patient-adjacent workforce data is protected at all layers.
Step 8: Deployment and Go-Live
Deployment must be planned meticulously to protect clinical operations and minimize disruption.
- Pilot rollout in one department
Launching the system in a single unit (such as ICU or emergency) allows teams to validate functionality, gather feedback, identify edge cases, and refine workflows. Pilot results help fine-tune scheduling rules and ensure the software aligns with real-world clinical practices.
- User onboarding
Training sessions, quick-start guides, mobile tutorials, and in-app walkthroughs help users adapt to the new system. Supervisors require advanced training on dashboards and reporting, while clinicians need guidance on mobile features such as clock-ins or shift swaps. Smooth onboarding accelerates adoption and reduces resistance to change.
Step 9: Ongoing Optimization and AI Retraining
After launch, continuous improvement is essential to maintain accuracy and efficiency.
- Monitoring workforce utilization improvements
Analytics dashboards track metrics such as overtime reduction, decrease in understaffed shifts, improved float pool utilization, and increased schedule predictability. AI models are retrained periodically with updated data to refine forecasting, reduce bias, and enhance performance. Feedback loops from supervisors and clinicians ensure the system evolves as workflows, regulations, or staffing strategies change. This ongoing optimization keeps the platform aligned with organizational needs and ensures sustained impact on clinical operations.
Integrations Required for Healthcare Workforce Systems
Integrations form the backbone of any modern healthcare workforce management platform. Hospitals and clinics rely on a wide array of digital systems — from EHRs and HRMS platforms to telehealth systems and attendance hardware — each generating operational data essential for accurate scheduling, compliance, and real-time decision-making. Without robust interoperability, workforce software becomes a siloed tool, unable to reflect patient acuity, clinician competencies, or staffing demands in real time. Integrations allow the workforce system to become a central node in the hospital’s broader digital ecosystem, ensuring staffing decisions are informed by live clinical and administrative information. The following sections detail the most critical integrations required for efficient, reliable, and scalable workforce management in healthcare organizations.
-
EHR Systems
Integration with electronic health record (EHR) systems is one of the most important requirements for workforce management. EHR platforms such as Epic, Cerner, and Meditech store essential data about patient census, acuity levels, admission rates, discharge trends, and clinical workflows. This information directly influences staffing needs across units.
A census-integrated workforce system automatically adjusts staffing forecasts based on expected admission surges or anticipated discharges. For example, if the emergency department experiences a spike in patient volume, the system can alert supervisors, recommend float pool redeployment, or trigger auto-scheduling adjustments. Acuity integration ensures that staffing ratios aren’t solely based on patient numbers but also reflect the complexity of care required. This results in safer clinical workloads and more accurate schedule planning.
EHR integrations typically rely on HL7 or FHIR APIs, ensuring real-time, secure data exchange. By connecting with EHRs, the workforce management platform becomes a dynamic scheduling engine that continuously adapts to patient care demands.
-
Payroll Systems
Workforce data directly affects payroll accuracy, making payroll integration essential for seamless financial operations. Payroll solutions like ADP, Workday, and UKG process complex compensation inputs including overtime, shift differentials, night premiums, holiday pay, and bonuses. While many growing companies start by searching for the best payroll software for small business to handle basic needs, they eventually require systems like ADP, Workday, and UKG to process complex compensation inputs including overtime, shift differentials, night premiums, holiday pay, and bonuses.
A tightly integrated system eliminates the need for manual reconciliation or duplicate data entry. When attendance logs, overtime calculations, and leave balances flow automatically into payroll software, hospitals reduce administrative errors and prevent payment disputes. Validations built into the integration help detect anomalies — such as missing clock-ins or unexpected overtime — before payroll is executed.
Payroll integration improves transparency and accuracy while reducing administrative burdens, allowing HR and finance teams to focus on strategic activities instead of manual corrections.
-
HR Platforms
Human resource management systems (HRMS) such as BambooHR, SAP SuccessFactors, Zoho People, or Oracle HCM hold critical workforce data including job roles, employment types, leave balances, performance evaluations, and demographic information. Workforce management platforms rely on this information to ensure accurate scheduling and compliance.
Integrating with HRMS platforms enables the scheduling engine to access real-time data about:
- Active vs inactive employees
- Contract types (full-time, part-time, per diem)
- Approved leave or PTO
- Qualifications and role-based access
- Seniority levels and union-related rules
This integration prevents conflicts such as assigning inactive staff, violating seniority rules, or scheduling clinicians currently on approved leave. Synchronizing HR data with attendance and scheduling modules ensures that the workforce system reflects the organization’s latest personnel structure, reducing errors and improving operational stability.
-
Staff Communication Apps
Effective communication is essential in healthcare, particularly during emergencies, unexpected call-outs, or rapid census changes. Workforce platforms often integrate with communication apps including Microsoft Teams, Slack, Vocera, Spok, or proprietary hospital messaging platforms.
Communication integrations enable real-time alerts such as:
- Urgent staffing requests
- Emergency shift coverage notifications
- Broadcast messages to entire units
- Policy updates or safety announcements
- Reminders for credential renewals or training sessions
These integrations help unify communication across departments, reducing delays and ensuring frontline teams receive updates immediately. For mobile workforce users, push notifications and SMS alerts enable rapid response and improve overall staffing agility.
-
Telehealth Platforms
Telehealth has become a permanent component of patient care, requiring workforce management tools to integrate with virtual care platforms such as Teladoc, Amwell, Doxy.me, or custom hospital telemedicine systems.
Telehealth integration supports:
- Scheduling remote physicians, therapists, and specialists
- Managing time zones and virtual session availability
- Tracking teleconsultation volumes
- Ensuring credential alignment with telehealth service types
- Balancing workloads across onsite and remote staff
By connecting workforce tools with telehealth platforms, hospitals ensure optimal coverage for video consultations, remote monitoring services, chronic disease follow-ups, and mental health sessions. This integration becomes especially important for multisite hospitals or health systems with distributed virtual care teams.
-
Attendance Hardware (RFID, Biometrics, Tablets)
Attendance and time tracking in healthcare often involve physical hardware due to the need for secure, verifiable logging. Integrating workforce systems with biometric scanners, RFID badges, smart cards, or wall-mounted tablets ensures accurate, real-time attendance data.
Key aspects include:
- RFID and smart cards: Quick swipes for high-traffic shift changes.
- Biometric devices: Fingerprint or facial recognition to prevent buddy punching and ensure identity accuracy.
- Tablets and kiosks: Stationed at nurse stations, clinician lounges, and department entrances for rapid check-in and check-out.
Attendance hardware integration feeds real-time time logs into the workforce system, supporting overtime calculation, absence alerts, shift reconciliation, and payroll synchronization. It eliminates discrepancies and strengthens compliance with break rules and shift-hour laws.
-
Hospital Command Center Systems
Large hospitals increasingly operate centralized command centers that monitor real-time clinical and operational activity, including bed availability, patient flow, emergency response, and staffing levels. Workforce management software must integrate with these systems to ensure that staffing decisions align with operational realities.
Command center integrations provide:
- Real-time staffing adequacy indicators
- Alerts for surge events or mass casualties
- Early warnings for units approaching staffing thresholds
- Unified dashboards combining staffing, patient flow, and resource data
- Support for predictive surge planning
For example, if the command center detects a sudden influx of emergency cases, the workforce system can automatically trigger staffing adjustments or emergency broadcast alerts. These integrations enable a coordinated, system-wide response that improves operational resilience and enhances patient safety.
Cost of Building Healthcare Workforce Management Software
Estimating the cost of building healthcare workforce management software requires more than a simple “price per feature” view. You are dealing with a complex system that must support high user concurrency, strict regulatory compliance, integrations with EHR/HR/payroll systems, and increasingly AI-driven decision support. Costs are influenced by product scope, region of the development team, depth of integrations, data security requirements, and how aggressively you invest in AI capabilities from day one. Below is a structured breakdown that you can use to frame realistic budgets and have serious conversations with vendors or internal stakeholders.
Cost breakdown by development stage
A typical custom build can be divided into several stages, each with its own cost profile:
- Discovery, analysis, and product definition
This includes stakeholder interviews, requirements workshops, workflow mapping, and the initial product specification. For a mid-sized hospital or multi-facility system, this phase often costs USD 15,000–40,000, depending on how many departments are included and how detailed the documentation needs to be. - UX/UI design and prototyping
You need separate journeys for supervisors, HR teams, administrators, and frontline staff using mobile devices. High-fidelity prototypes for scheduling dashboards, analytics screens, and nurse apps typically cost in the range of USD 20,000–60,000 for a serious product. - Core backend and frontend development
This is usually the largest chunk. It covers scheduling logic, attendance tracking, credentialing, notifications, role-based access, web admin portals, and mobile apps. For an initial product with solid architecture and clean code, expect USD 120,000–300,000 depending on complexity and region. - Integrations
Connecting to EHR, HR, payroll, attendance hardware, and telehealth systems has its own cost line. Even a minimal integration set can easily add USD 30,000–100,000, especially when you are working with multiple external vendors and standards. - Testing, security hardening, and compliance validation
This includes functional QA, performance testing, penetration testing, and validation against HIPAA and regional labor regulations. For a healthcare-grade system, plan USD 25,000–80,000 for a serious testing effort. - Deployment, training, and change management
Rolling out to one or more facilities, training supervisors and staff, and supporting the first few months of production use can add USD 15,000–50,000, depending on the scale and level of on-site vs remote support. - Ongoing maintenance and feature enhancements
Annual maintenance (bug fixes, small enhancements, infrastructure costs) typically runs 15–25 percent of initial build cost per year.
Regional cost comparison (US vs Europe vs India)
Development costs vary significantly by geography. For the same product scope:
- US-based teams generally charge USD 120–200 per hour for senior engineers and architects. A full build with integrations and basic AI can easily reach USD 400,000–900,000.
- Western Europe and UK typically fall in the USD 90–160 per hour range, leading to total build costs in a similar band, often USD 300,000–750,000.
- Nearshore Eastern Europe / LATAM may offer USD 50–90 per hour, which can reduce total costs to USD 200,000–500,000 for a full-featured implementation.
- India and similar offshore hubs can often deliver strong healthcare-grade systems at USD 30–60 per hour, with total project costs for an enterprise-ready solution in the USD 150,000–350,000 band, depending on scope and AI depth.
Hybrid models are common: product leadership and domain specialists in the US or Europe combined with delivery teams in India to balance quality and cost.
Cost difference between MVP and full enterprise platform
You should distinguish between a focused MVP and a full enterprise-grade platform.
MVP scope often includes:
- Basic shift scheduling and staff profiles
- Time and attendance tracking (software-based, limited hardware integration)
- Simple mobile access to schedules
- One or two key integrations (for example, HR + payroll only)
- Basic analytics (overtime, coverage, simple reports)
A serious healthcare MVP is rarely “cheap.” Realistic ranges:
- India / offshore-heavy model: USD 80,000–150,000
- Hybrid / nearshore: USD 150,000–250,000
- Pure US / Western Europe: USD 250,000–400,000
Full enterprise platform typically adds:
- Advanced scheduling logic with ratios, union rules, skill mix, and fatigue constraints
- Deep EHR integration with census and acuity data
- Multiple integrations (EHR, HR, payroll, telehealth, hardware)
- Robust analytics and dashboards with departmental benchmarking
- AI capabilities for predictive staffing and optimization
- Enterprise-grade security, full audit, and multi-hospital rollouts
Budgets for this level are often 2–4 times the MVP cost, especially once you include multi-year enhancements and rollouts to many sites.
AI feature development cost impact
AI is no longer optional if you want a competitive, future-proof workforce platform, but it does introduce additional budget lines.
Key AI-related cost drivers include:
- Data engineering: cleaning and preparing historical workforce, census, and acuity data.
- Model development: forecasting models for census, absenteeism, and workload; optimization models for scheduling.
- LLM-based copilots: integrating hosted LLMs, building secure prompts and guardrails, and connecting them to workforce data.
- Continuous retraining and monitoring: calibrating models as patterns change.
When evaluating the cost of implementing AI in healthcare, a realistic setup that includes predictive scheduling, ML-based float pool optimization, and an entry-level LLM copilot generally adds USD 40,000–150,000 beyond the core software development budget. The range depends on whether you rely on existing AI services or pursue deep customization, experimentation, and model tuning.
If AI will be executed as a phase-two enhancement, the investment can be spread out. Still, the system should be architected from the beginning with data pipelines and model integration points so you avoid redesign costs later.
Integration cost, compliance cost, and support cost
Integrations are one of the most underestimated parts of the budget. Each additional system (Epic, Cerner, ADP, Workday, BambooHR, RFID hardware, telehealth platforms) brings:
- API discovery and coordination with external vendors
- Data mapping and transformation
- Error handling, monitoring, and security reviews
Realistically, each major integration can cost USD 10,000–40,000, sometimes more if the vendor has complex requirements or limited API maturity.
Compliance and security also carry direct and indirect costs:
- Architecture reviews and threat modeling
- Encryption setup, key management, and audit logging
- External penetration tests and HIPAA / GDPR readiness assessments
You should plan at least USD 20,000–60,000 specifically tied to security and compliance, with ongoing annual costs for audits and certifications.
Support and maintenance:
- Fixing bugs, updating dependencies, and OS/DB patches
- Handling change requests from HR, nursing, and IT
- Monitoring AI model performance and retraining schedules
A practical rule of thumb is 15–25 percent of initial build cost per year as a support and enhancement budget.
Example budgets and timelines
To make this concrete, here are simplified scenarios:
Scenario 1: Single-hospital MVP, offshore-heavy build
- Scope: Core scheduling, attendance, mobile access, HR + payroll integration, basic reporting
- Budget: USD 100,000–150,000
- Timeline: 6–8 months to production for one hospital
- AI: Possibly basic forecasting as a later phase
Scenario 2: Multi-hospital enterprise platform with AI and integrations
- Scope: Advanced scheduling, ratios, union rules, float pool, multi-hospital support, EHR + HR + payroll + hardware integrations, predictive scheduling, optimization engine, security hardening
- Budget:
- Offshore / hybrid: USD 250,000–500,000
- Pure US/Europe: USD 500,000–900,000+
- Timeline:
- 9–14 months for initial deployment
- Additional 6–12 months for rollouts to multiple sites and advanced AI features
Scenario 3: Incremental build with AI-first approach
- Phase 1: MVP with clean architecture and limited EHR/HR integration
- Phase 2: Add AI forecasting, auto-scheduling, and LLM copilot
- Combined budget over 18–24 months: typically USD 200,000–600,000 depending on region and ambition.
For any serious healthcare organization, the right question is not “What is the absolute lowest cost?” but “What budget and timeline are realistic for a clinically safe, compliant, and extensible workforce platform that will serve our hospital for the next 5–10 years?”
Common Challenges in Healthcare Workforce Management Software
Developing and operating healthcare workforce management software involves navigating a variety of complex challenges that stem from the unique nature of clinical work. Hospitals run 24×7, manage constantly changing patient volumes, and depend on staff with highly specialized skills. Compliance requirements, union rules, multi-department needs, and unpredictable emergencies add further complexity. Even well-designed workforce systems must overcome these operational realities to deliver meaningful impact. The challenges outlined below represent the core obstacles that healthcare organizations face when implementing or scaling workforce management platforms, and understanding them is essential for designing resilient, intuitive, and clinically safe solutions.
-
High variability in shifts and departments
One of the biggest operational challenges arises from the immense variability in staffing needs across different hospital units. A surgical ICU may require continuous coverage from specialized nurses, respiratory therapists, and intensivists, while a general medical ward may deal with lower-acuity patients but higher census fluctuations. Emergency departments experience extreme unpredictability due to trauma cases, seasonal illnesses, and sudden patient surges. These variations make it difficult to build a “one-size-fits-all” scheduling framework. Workforce management software must support unit-specific templates, skill mix rules, floating constraints, and dynamic reallocation of staff. Without this flexibility, the system risks creating unsafe or impractical schedules that do not align with real clinical workflows.
-
Resistance to technology adoption
Healthcare environments often experience resistance to new technology, especially in workforce-related workflows that directly impact clinicians’ daily routines. Nurses and physicians may prefer familiar methods such as whiteboards, WhatsApp groups, or informal verbal coordination. Supervisors may worry that automation will reduce their control over scheduling decisions or increase scrutiny of their staffing practices. Older staff may feel uncomfortable navigating digital dashboards or mobile apps. If the platform is unintuitive or lacks strong onboarding, adoption falters. Overcoming resistance requires a combination of user-centered design, step-by-step training, change management, and demonstrating quick wins — such as reduced scheduling conflicts or easier shift swaps. Without proactive adoption strategies, even the most capable software can struggle to deliver value.
-
Complex compliance logic
Healthcare staffing is governed by a dense network of labor laws, nurse-to-patient ratio mandates, union agreements, credentialing requirements, break rules, and fatigue thresholds. Implementing these rules in software requires precise logic, rigorous testing, and ongoing updates as policies evolve. Compliance rules vary not only by country or state, but often by department, shift type, or specialty. For example, ICU staffing may require different ratios and credentials than maternity wards or behavioral health units. Embedding these constraints while keeping the scheduling engine responsive and efficient is a major technical challenge. Any gaps in compliance logic risk exposing the hospital to regulatory penalties, legal disputes, or unsafe staffing conditions. Continuous review and alignment with HR, legal teams, and nursing leadership are essential to maintaining accurate rule sets.
-
Avoiding schedule conflicts and fatigue violations
Scheduling conflicts are common in healthcare because staff often work rotating shifts, switch units, or cover multiple roles. Overlapping assignments, double bookings, or insufficient rest hours can easily occur without intelligent automation. Fatigue-induced errors are linked to medication mistakes, reduced cognitive performance, and higher patient risk. Workforce platforms must enforce mandatory rest hours, cap consecutive night shifts, and prevent staff from being scheduled back-to-back across units. Real-time validation is required to flag conflicts the moment they occur rather than after schedules have been published. Ensuring that these safeguards do not slow down the scheduling workflow is another major design challenge. A balance must be struck between strict rule enforcement and the operational need for flexibility during emergencies.
-
Ensuring real-time attendance accuracy
Accurate attendance data is crucial because it drives payroll, overtime calculations, labor cost forecasting, and schedule compliance. In busy hospital environments, staff may forget to clock in, use the wrong device, or move between departments without updating their status. Technical issues with biometric devices, time kiosks, or mobile check-ins can further complicate data accuracy. In multi-facility systems, inconsistent device setups or network constraints can lead to data delays. Workforce systems need robust error detection, fallback check-in methods, automated verification rules, and reconciliation capabilities to ensure attendance records reflect reality. Without reliable attendance data, scheduling adjustments, labor analytics, and compliance reporting lose credibility.
-
Managing communication overload
Healthcare teams receive a continuous stream of messages — shift updates, emergency alerts, patient-related communications, policy updates, and task assignments. Poorly designed workforce platforms risk adding to this communication overload rather than reducing it. Too many notifications can cause alert fatigue, where clinicians start ignoring messages, leading to missed shift changes or delayed responses. Conversely, insufficient communication can result in confusion, inadequate coverage, or missed compliance deadlines. Workforce systems must implement intelligent alerting logic, grouping non-urgent messages, prioritizing critical notifications, and delivering updates through channels appropriate to the user’s role and urgency level. Mobile interfaces should show clear summaries and allow staff to act quickly without being overwhelmed.
How to Choose a Healthcare Workforce Management Software Development Partner
Selecting the right healthcare software development partner is one of the most consequential decisions in building a healthcare workforce management platform. This is not a standard HR application. It must integrate with EHRs, operate under strict regulatory constraints, support clinical-grade reliability, and scale across departments with very different workflows. A capable partner must combine deep healthcare domain understanding with technical sophistication, data security maturity, and proven delivery governance. The following criteria provide a structured framework to evaluate vendors and engineering teams.
-
Expertise in healthcare domain and compliance
Workforce management in healthcare is inseparable from clinical realities. The development partner should demonstrate a strong understanding of patient acuity, staffing ratio laws, credentialing workflows, union contracts, and the operational differences between ICUs, emergency departments, operating rooms, and general wards. They must also be comfortable working within regulatory frameworks such as HIPAA, GDPR, NABH, and JCI.
Technical compliance experience matters just as much as legal literacy. The partner should have prior experience implementing:
- HIPAA-compliant architectures
- Audit logging
- Secure identity and access management
- Encryption standards
- Policies for PHI and staff-sensitive data
Teams lacking healthcare exposure often misjudge compliance complexity, resulting in delays, rework, or unsafe product decisions. A partner with clinical domain depth accelerates development and reduces the risk of structural mistakes in the product.
-
Experience in HRMS and workforce systems
Although this is a healthcare system, it also functions as an advanced HR, scheduling, and operational intelligence engine. The partner should have prior experience building systems in these categories:
- HRMS and staff management platforms
- Time and attendance systems
- Complex shift scheduling engines
- Payroll integrations
- Competency or credential tracking modules
Experience with these domains ensures the team understands critical features such as shift rotation logic, overtime rules, attendance reconciliation, and workforce analytics. Healthcare adds complexity, but the core HR workflows must already be second nature to the development partner. This avoids reinventing the wheel and ensures the project focuses on healthcare-specific intelligence rather than generic HR plumbing.
-
AI, ML, and predictive analytics capability
Modern workforce management increasingly depends on AI-driven features such as predictive staffing, census forecasting, float pool optimization, and LLM-based copilots for supervisors. A development partner must demonstrate hands-on experience with:
- Time series forecasting models
- Machine learning–driven optimization algorithms
- Large language model integration
- RAG-powered decision support
- Real-time data pipelines for model inference
- AI compliance frameworks
Healthcare organizations can no longer rely solely on static rules. Choosing a partner with established AI engineering practices ensures your platform can evolve with the industry and remain competitive over the long term.
-
Interoperability readiness: HL7, FHIR, and EHR connectors
Interoperability is fundamental. Workforce management software must exchange data with EHRs, HRMS systems, payroll platforms, attendance devices, and telehealth tools. The development partner should be fluent in:
- HL7 v2 and FHIR
- RESTful APIs used by Epic, Cerner, and Meditech
- Payroll APIs (ADP, Workday, UKG)
- HRMS APIs (SAP SuccessFactors, BambooHR, Oracle HCM)
- Device integrations (RFID, biometrics, tablets)
They should also be capable of designing an architecture that can absorb new integrations as the health system evolves. Without interoperability maturity, the workforce platform becomes a siloed tool rather than the operational nerve center it must be.
-
Proven enterprise delivery track record
Healthcare organizations need stable, scalable, and long-lived software — not prototypes or short-term builds. A strong partner will demonstrate:
- Experience with multi-phase, multi-year delivery
- Success working with hospitals, clinics, or regulated enterprises
- Governance frameworks for risk management, documentation, and quality control
- Ability to support deployments across multiple facilities
- Mature DevOps, CI/CD, and monitoring capabilities
A delivery partner should be able to present case studies or references demonstrating how they navigated complex requirements, adapted to real-world constraints, and delivered production-ready platforms that continued to evolve post-launch.
What makes Aalpha a strong partner
Aalpha Information Systems presents a credible fit for healthcare workforce management projects because of three foundational competencies:
- Cross-disciplinary expertise across healthcare, HR, and AI engineering
Aalpha has substantial experience across healthcare IT, HRMS development, and enterprise workforce systems. This combination is essential because healthcare workforce management sits at the intersection of all three. Their teams are familiar with clinical workflows, regulatory requirements, and the architectural demands of systems that must run 24×7 in mission-critical environments. - Strong capabilities in integrations and interoperability
Aalpha’s engineering teams routinely build connectors for EHRs, payroll systems, HRMS platforms, and medical devices. Their experience working with HL7, FHIR, and enterprise API ecosystems supports the type of interoperability required for a hospital-grade workforce solution. - Proven track record delivering enterprise software at scale
Aalpha has delivered large, multi-module, and multi-stakeholder platforms across healthcare, finance, logistics, and SaaS verticals. This background demonstrates the capacity to handle complex requirements, multi-phase rollouts, and institutional-level expectations for security, uptime, and governance.
These strengths make Aalpha an appropriate engineering partner for organizations seeking a long-term, scalable approach to developing healthcare workforce management software — not as a promotional claim, but as a factual reflection of their delivery history and technical depth.
Conclusion
Healthcare workforce management has become one of the most strategically important operational capabilities for hospitals, clinics, and multi-facility health systems. As patient volumes rise, staffing shortages persist, and compliance expectations tighten, organizations can no longer rely on spreadsheets, manual schedules, or fragmented communication channels. A modern workforce management platform brings structure, consistency, and intelligence to the most resource-intensive function in healthcare: deploying the right clinician to the right place at the right time.
By incorporating automated scheduling, real-time attendance tracking, credential and compliance management, AI-powered forecasting, and deep interoperability with EHR, HRMS, and payroll systems, these platforms transform workforce operations from reactive crisis management into a data-driven discipline. Hospitals using advanced tools see measurable improvements in staffing adequacy, clinician satisfaction, cost control, patient safety, and continuity of care.
The development of such software requires careful planning, stakeholder alignment, rigorous adherence to compliance frameworks, and thoughtful integration of AI and analytics. It is not enough to build a scheduling tool; the system must reflect the realities of clinical care, multi-department workflows, union rules, and the need for real-time decision-making in high-pressure environments. This guide has outlined the scope, challenges, architecture, and costs associated with designing an enterprise-grade workforce management solution built specifically for healthcare.
Healthcare leaders who invest in intelligent workforce management lay the foundation for safer patient care, more predictable operations, and a healthier, more supported clinical workforce. As the industry moves toward predictive staffing and autonomous operations, the ability to manage workforce complexity at scale will become a defining competitive and clinical advantage.
If you’re exploring the development of a custom healthcare workforce management platform or looking to enhance an existing system with AI, predictive staffing, or deeper integrations — our team can help. Contact Aalpha to discuss your requirements, review technical possibilities, and receive a tailored roadmap aligned with your organization’s operational and compliance needs.