A tech stack also known as a technology stack is a list of all the technology services used to build and run an application. This typically consists of the programming languages, framework, a database, front-end tools, back-end tools, and applications connected via API.
It is also important to note that you will not find two identical tech stacks, the combination of the coding frameworks and languages will always be different from one tech stack to another. For example Facebook a social site has a combination of JavaScript, HTML, CSS, PHP, and ReactJS as its tech stack which is a different combination from that of Twitter another social site.so when choosing one you have to have in mind the problem you want to solve and not just go for the popular one in the market.
Since the advent of the computer era, there has been a rapid growth in the demand for healthcare tech stacks but none has been witnessed in magnitude as the one we have witnessed with the outbreak of covid 19. The pandemic disrupted the entire healthcare industry and gave rise to an explosive demand for healthcare software and applications.
Some of the popular tech stacks include:
LAMP STACK: Linux, Apache, MySQL, Php
Ruby on Rails: Ruby, Rails, Passenger, Rack
Mean stack: MongoDB, Express.js, AngularJS, Node.js
To name but a few.
What is a Technology Stack in Healthcare?
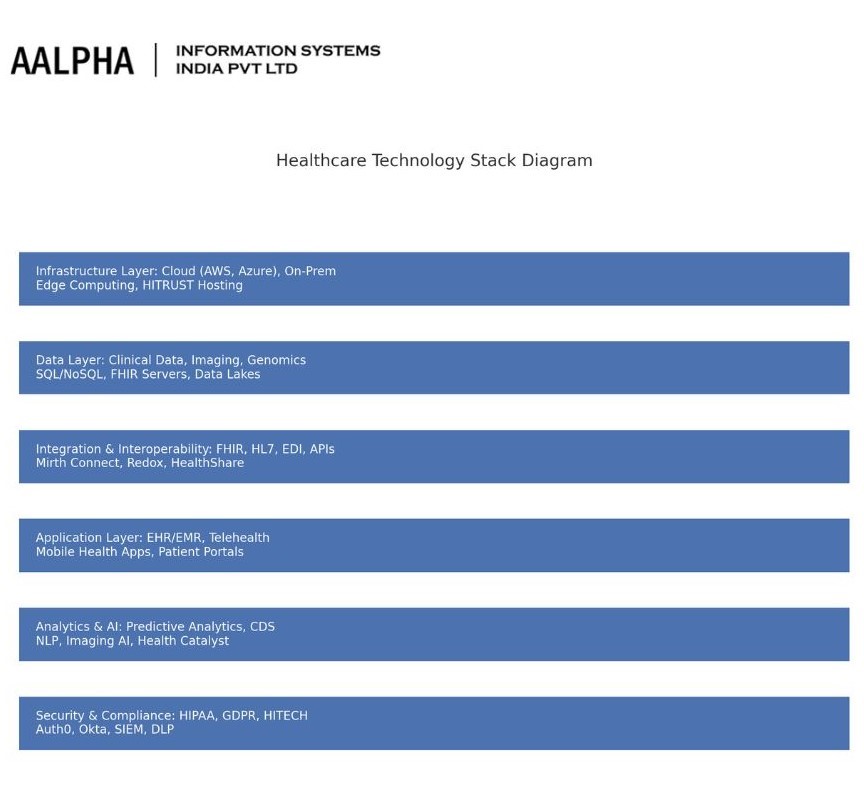
A technology stack refers to the layered set of software, hardware, and services used to build and operate healthcare applications and systems. Unlike generic enterprise IT stacks, a healthcare stack must operate in an environment where uptime, accuracy, security, and interoperability are not just business concerns—they’re matters of clinical safety and regulatory necessity.
At its core, a healthcare technology stack includes:
- Infrastructure Layer: Data centers, cloud platforms, edge devices, and networking components.
- Data Layer: Storage systems, relational and non-relational databases, data lakes, and formats like HL7 and FHIR.
- Integration Layer: Middleware, APIs, and message brokers that connect disparate systems.
- Application Layer: EHRs, scheduling platforms, patient portals, telemedicine systems, and mobile health apps.
- Analytics & AI Layer: Tools for real-time monitoring, clinical decision support, predictive analytics, and machine learning models.
- Security & Compliance Layer: Systems ensuring HIPAA/GDPR compliance, access control, encryption, and audit trails.
This stack functions like a living organism: interconnected, evolving, and often under strain. A decision made at one layer—say, cloud architecture—can impact everything from clinical workflows to regulatory audits.
2. Market Landscape & Growth Trends
Global Healthcare IT Market: 2025–2030 Outlook
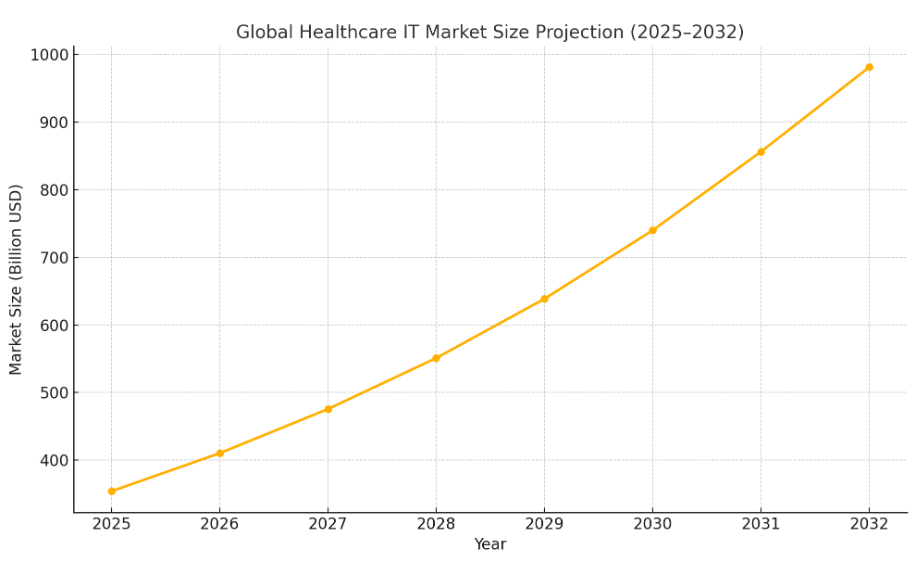
The global healthcare IT (HCIT) market is poised for substantial growth over the next decade. Estimates suggest the market will expand from $354.04 billion in 2025 to $981.23 billion by 2032, reflecting a compound annual growth rate (CAGR) of 15.7% . This surge is driven by factors such as the widespread adoption of electronic health records (EHRs), the proliferation of telehealth services, and the integration of artificial intelligence (AI) in healthcare operations. Source: Fortune Business Insights
Regional Breakdown
United States
The U.S. remains the largest market for healthcare IT, with expenditures reaching $176.6 billion, accounting for approximately 63% of global HCIT spending . Key growth drivers include:
- Regulatory initiatives like the Health Information Technology for Economic and Clinical Health (HITECH) Act, which allocated around $27 billion over a decade to promote EHR adoption.
- Advancements in AI and cloud computing, enhancing clinical documentation and hospital automation.
Europe
Europe holds a significant share of the HCIT market, with countries like the United Kingdom, Germany, and France leading in digital health adoption. The region’s growth is bolstered by:
- Government support for digital health initiatives, such as the European Health Data Space (EHDS) aimed at improving data sharing across borders.
- Increased AI adoption in healthcare, streamlining operations and enhancing patient care.
Asia-Pacific (APAC)
APAC is the fastest-growing region in the HCIT market, projected to grow at a CAGR of 11.4%, reaching $84.23 billion by 2031 . Growth factors include:
- Government investments in digital health infrastructure, exemplified by India’s National Digital Health Mission and China’s Healthy China 2030 plan.
- Rising demand for telehealth and mobile health applications, driven by increasing smartphone penetration and internet accessibility.
Key Market Drivers
Digital Transformation
The digitalization of healthcare services is a primary catalyst for HCIT market growth. Technologies such as cloud computing, big data analytics, and AI are revolutionizing patient care and administrative processes. For instance, AI-driven diagnostics and predictive analytics are enhancing clinical decision-making and operational efficiency.
Electronic Health Records (EHR) Mandates
Mandatory implementation of EHR systems across various countries has significantly contributed to market expansion. In the U.S., the HITECH Act incentivized EHR adoption, leading to widespread integration in healthcare facilities . Similarly, other regions have introduced policies to promote digital record-keeping, improving data accessibility and patient care continuity.
Artificial Intelligence Integration
AI is increasingly embedded in healthcare IT solutions, offering capabilities such as:
- Predictive analytics for patient risk stratification.
- Natural language processing to streamline clinical documentation.
- Computer vision for medical imaging analysis.
Major tech companies like Amazon, Nvidia, and Microsoft are investing heavily in healthcare AI, developing tools that enhance diagnostics, treatment planning, and administrative tasks.
Remote Care and Telehealth
The COVID-19 pandemic accelerated the adoption of telehealth services, a trend that continues to shape the HCIT landscape. Remote patient monitoring (RPM) and virtual consultations have become integral to healthcare delivery, offering benefits such as:
- Improved access to care for patients in remote or underserved areas.
- Reduced healthcare costs through decreased hospital readmissions.
- Enhanced patient engagement and satisfaction.
The global telehealth market is projected to grow substantially, with estimates suggesting it will reach over $475.50 billion by 2026.
Benefits of Tech stacks in healthcare development
Healthcare tech stacks have had far and wide-reaching benefits and to understand the benefits further we will subdivide them into 3, namely;
- Benefits to the doctors,
- Benefits to the patients
- Benefits to healthcare organizations
Benefits to the doctors
- Reduced paperwork
Paperwork is significantly reduced Which in turn reduces pressure on the doctors and allows them to concentrate more on quality care in primary healthcare and patient treatment as opposed to filling forms
- Increased collaboration with other specialists
Technology has removed all geographical boundaries and has enabled healthcare providers to connect and share knowledge with other practitioners across the globe
- Effective Patient management
Patients’ data is now more effectively and efficiently managed with software.
This in turn also saves time and more time is spent on quality care.
Benefits to patients
- Enhances patient outreach
Patients can connect easily with healthcare providers through their portals and mobile healthcare apps.
- Improved healthcare
With less paperwork involved the doctors can concentrate on primary care thus the patients received quality care.
- Enhanced communication
Managing communication has become easy through apps that facilitate instant messaging and calling, appointment scheduling, and even reminders.
Benefits to healthcare providers
- Improved medical business management
Improved data collection, storage, and management have led to an overall increase in organizations’ performance
- Patient satisfaction
Efficiency in the provision of services has led to satisfaction with services offered on the patients’ side which is always a plus in the service industry.
Core Layers of the Healthcare Technology Stack
Understanding the core layers of the healthcare technology stack is essential for building resilient, scalable, and compliant systems. Each layer contributes to the overall integrity, security, and functionality of the healthcare delivery infrastructure. This section breaks down each major layer in detail.
a. Infrastructure Layer
On-Premises vs. Cloud
Traditionally, healthcare institutions relied on on-premises data centers for hosting their systems. These environments gave institutions full control over physical hardware and data access. However, on-premises solutions are increasingly seen as costly, difficult to scale, and slow to innovate.
In contrast, cloud providers like Amazon Web Services (AWS) and Microsoft Azure offer healthcare-optimized solutions. Both platforms provide HIPAA-eligible services, region-specific data hosting, and elastic scalability. Cloud infrastructure reduces the burden of hardware management while enabling faster deployment cycles and real-time analytics.
Compliance-Focused Hosting
Healthcare providers must comply with strict regulatory standards such as HIPAA, HITECH, and GDPR. This has led to the rise of compliance-first cloud environments. HITRUST-certified hosting platforms ensure that infrastructure meets rigorous compliance frameworks. Vendors like AWS (through AWS Artifact), Google Cloud, and Azure provide documentation, audit trails, and compliance toolkits to simplify governance.
Edge Computing in Hospital Settings
Edge computing is gaining traction in healthcare for latency-sensitive applications. Devices such as connected imaging machines, surgical robots, or bedside monitors generate and process data locally, reducing the need to send everything to the cloud. This is critical for time-sensitive decision-making, particularly in emergency care and operating rooms.
b. Data Layer
Data Types
Healthcare generates diverse data types:
- Clinical data (EHRs, lab results, physician notes)
- Patient-generated health data (PGHD) (wearables, home devices)
- Imaging data (radiology, pathology)
- Genomic data (used in precision medicine and pharmacogenomics)
Databases and Standards
To manage this complexity, healthcare organizations use various database types:
- SQL databases (e.g., PostgreSQL, MS SQL Server) for structured data like patient records.
- NoSQL systems (e.g., MongoDB) for flexible data formats and unstructured content.
- FHIR servers for real-time, standardized data exchange.
- HL7 interfaces for legacy system integrations.
Data Lakes & Warehouses
Healthcare institutions are increasingly adopting:
- Data lakes to store raw, heterogeneous data in real time.
- Data warehouses (e.g., Snowflake, Google BigQuery, Amazon Redshift) for structured data analysis, reporting, and compliance auditing.
c. Integration & Interoperability Layer
Standards and Protocols
Interoperability is a cornerstone of modern healthcare IT. Key standards include:
- HL7 v2/v3: Widely used for clinical messaging.
- FHIR (Fast Healthcare Interoperability Resources): RESTful API-based standard supporting real-time data exchange.
- EDI (Electronic Data Interchange): Used for insurance claims and billing.
- APIs: Custom and open APIs connect systems across the care continuum.
Middleware and Message Brokers
Middleware platforms help bridge communication between disparate systems. Leading solutions include:
- Mirth Connect: Open-source integration engine.
- Redox: API platform enabling app-EHR interoperability.
- InterSystems HealthShare: Facilitates unified health records across systems.
Legacy Integration Challenges
Older hospital systems often lack API support or conform to outdated protocols. Integrating them with modern cloud-based apps requires middleware, custom adapters, and data normalization layers. These projects are resource-intensive and require domain-specific knowledge.
d. Application Layer
Electronic Health Records (EHR/EMR)
Core to any healthcare system, EHRs store longitudinal patient records. Key platforms include:
- Epic Systems
- Cerner (Oracle Health)
- Meditech
- OpenEMR (open-source)
These platforms are often customized per institution and integrated with ancillary systems like lab information systems (LIS) or radiology PACS.
Telehealth Platforms
Adoption of virtual care has surged, especially post-pandemic. Tools such as Teladoc Health, Amwell, and Doxy.me support video consultations, appointment scheduling, and digital prescriptions.
Patient Engagement Tools
Modern platforms include self-service portals for accessing medical records, booking appointments, and communicating with providers. These often integrate with EHRs and mobile apps.
Mobile and Wearable Integrations
Apple HealthKit, Google Fit, and various mHealth apps allow integration of fitness, vitals, and chronic condition tracking into clinical systems, enhancing remote patient monitoring and engagement.
e. Analytics & AI Layer
Predictive Analytics & Decision Support
Analytics platforms process clinical data to support:
- Early disease detection
- Readmission prediction
- Treatment pathway recommendations
Clinical decision support tools are often integrated with EHRs to provide real-time prompts and risk scores.
Population Health & Risk Stratification
Population health platforms aggregate and analyze data across demographics, chronic disease indicators, and care outcomes. Tools like Health Catalyst help segment patients for intervention and measure value-based care metrics.
AI in Diagnostics and NLP
AI applications include:
- Computer vision in radiology (e.g., Aidoc, Zebra Medical)
- NLP tools to parse unstructured clinical notes
- Chatbots for symptom triage and patient communication
Tools
- SAS: Advanced analytics and predictive modeling
- Health Catalyst: Data platform and analytics for population health
- Google Health AI: Research-focused tools for imaging and diagnostics
f. Security & Compliance Layer
Regulations
Security and compliance are governed by region-specific mandates:
- HIPAA (U.S.)
- GDPR (EU)
- HITECH (U.S., promotes EHR adoption and security)
These dictate rules for data storage, transmission, breach notifications, and patient access rights.
Identity and Access Management
Platforms like Okta and Auth0 manage secure user authentication, authorization, and role-based access control across clinical and administrative tools.
Data Protection Technologies
- Encryption: AES-256 encryption in transit and at rest.
- Data Loss Prevention (DLP): Tools like Microsoft Defender and Symantec for sensitive data monitoring.
- SIEM (Security Information and Event Management): Solutions like Splunk and IBM QRadar for real-time threat detection, audit logging, and compliance monitoring.
By understanding each of these six layers, decision-makers can make informed, future-ready technology investments that align with their organization’s goals for security, scalability, and patient-centric care.
What to consider when choosing a Healthcare tech stack
- Integration with other systems
- Know your Target audience
- Should be User friendly i.e. UI/UX
- Data security
Remember not to choose a tech stack because it works well for another healthcare provider or is currently trending. Instead, choose a set of tools that will work best for your current needs.
How to choose the right tech stack for a specific need
When looking to solve a particular need, the right tech stack is of paramount importance. Some factors to consider to ensure this is achieved include;
- The language or languages you intend to use for development
- The operating system(OS) you want to install on
- Database technologies you will use
- The technical assistance you might need or require in the development
A wrong choice of technology might lead to a situation where you don’t get a solution for what you intended to solve or a loss of time and money.
How tech stacks are contributing to the development of healthcare systems
Modern healthcare provision establishments have moved from excessive paperwork and are now seamlessly managing different processes using the various available healthcare software that has made things easier for both the medical practitioners and patients.
Different Tech stacks are being used in the development of these healthcare systems.
Let us look at some of the healthcare systems that have been developed.
Practice Management System
This software integrates all clinical and administrative processes helping greatly with efficiency.
The system may include a scheduling solution where patients book an appointment, a billing solution for various healthcare needs — taking cardiology medical billing as an example, where payments and insurance claims can be automated, and even an e-prescription solution where physicians can send prescriptions directly to pharmacies where patients will go pick up their prescriptions.
EMR
Electronic Medical Records system, is a system that stores data, giving an alternative to the old way of archiving records in paperwork
EHR
Known in full as Electronic Healthcare Records, EHR system, it is almost similar to EMR. The difference is that in EMR the data can be shared only in one office but in EHR the data can be shared with other clinical establishments.
Patient portals and Mobile Apps,
Patient portals and mobile apps have made healthcare more accessible and portable. Patients are now more educated and engaged in the treatment process than ever.
Portals and apps are now providing tools like online appointments, consultations, billing, and even educational information on healthcare.
The significant role that Tech stacks are playing in healthcare development cannot be therefore overemphasized and the revolution they have created has changed the ways of provision of healthcare as had been known before. Ours is to sit down and enjoy the new era of healthcare provision that is upon us.
Emerging Technologies in Healthcare IT
Blockchain in Patient Records
Blockchain technology is being explored to address long-standing issues in patient record management, particularly around data integrity, privacy, and interoperability. A decentralized, immutable ledger allows patients to control access to their health information and offers audit trails for every access or modification. Projects like Estonia’s eHealth Authority and the MIT MedRec initiative have demonstrated how blockchain can improve consent management, cross-institutional data sharing, and breach resilience.
Digital Twins and Simulation
Digital twins are real-time virtual replicas of patients, hospital operations, or medical devices. They are created using real-time sensor data and simulation models to forecast scenarios, predict outcomes, and guide treatment decisions. In healthcare, digital twins are used in areas such as:
- Personalized care simulations (e.g., for cardiology or orthopedics)
- Hospital workflow modeling
- Clinical trial simulations
Companies like Siemens Healthineers and Philips are investing heavily in this domain, integrating digital twins into diagnostic imaging and surgical planning tools.
Federated Learning in Healthcare AI
Traditional AI training methods require centralizing data, which poses privacy and compliance challenges. Federated learning enables model training across decentralized datasets without moving the data itself. Hospitals or labs can collaboratively train machine learning models while retaining local control over their data. Google has piloted federated learning in diabetic retinopathy screening, showing it’s feasible to deploy privacy-preserving AI at scale across multiple institutions.
Synthetic Data for Training Models
Access to high-quality medical datasets is limited due to privacy concerns. Synthetic data—artificially generated but statistically similar to real patient data—offers a solution. Tools like Syntegra and MDClone use generative models to create datasets for model training, clinical research, or system testing. Synthetic data helps address:
- Data sparsity in rare conditions
- Bias in training datasets
- Testing of interoperability and integration functions without PHI exposure
Explainable AI in Clinical Workflows
Adoption of AI in clinical settings depends on its explainability. Clinicians must understand and trust algorithmic outputs to make informed decisions. Explainable AI (XAI) techniques such as SHAP (SHapley Additive exPlanations) and LIME (Local Interpretable Model-Agnostic Explanations) are being embedded into diagnostic and decision support systems.
For instance, when an AI model flags a potential malignancy in an image, XAI tools can highlight the pixel regions and features influencing the decision. This transparency enhances clinician trust and meets emerging regulatory standards for AI accountability.
Selecting and Building a Scalable Tech Stack
Building an effective healthcare technology stack requires a strategic balance between performance, compliance, scalability, and cost. Given the complexity and regulatory nature of the healthcare sector, decision-makers must evaluate multiple dimensions before committing to technologies or vendors. This section offers a detailed guide for selecting and constructing a scalable tech stack that aligns with clinical, financial, and operational objectives.
Evaluation Criteria
Compliance
Compliance is the first and non-negotiable consideration in healthcare IT. Any system must support industry-specific regulations such as HIPAA (U.S.), GDPR (EU), and HITECH. Evaluation should focus on:
- Encryption standards (e.g., AES-256, TLS 1.2+)
- Logging and audit readiness
- Role-based access control (RBAC)
- Certifications (e.g., HITRUST, ISO 27001, SOC 2)
Integration Capability
The stack must be interoperable with existing and future systems. Key integration considerations include:
- API-first design and FHIR compatibility
- Middleware adaptability for legacy systems
- Event-driven architectures and message brokers
- Vendor support for EHR, billing, and device interfaces
Performance
The stack should deliver consistent performance across geographies and user types. Metrics to evaluate:
- Uptime SLAs and geographic redundancy
- Latency benchmarks for critical operations
- Response time under load (e.g., during emergencies)
- Support for mobile and low-bandwidth environments
Buy vs. Build vs. Hybrid Models
Buy (Off-the-Shelf Solutions)
Pros:
- Faster deployment and time-to-value
- Lower upfront development costs
- Built-in compliance and support services
Cons:
- Limited customization
- Risk of vendor lock-in
- May not align perfectly with specific workflows
Build (In-House Development)
Pros:
- Tailored to institutional workflows and needs
- Greater control over architecture, data, and security
- Easier integration with existing internal systems
Cons:
- High development and maintenance costs
- Longer time-to-market
- Requires deep technical expertise in healthcare
Hybrid Model
Combines commercial solutions with custom modules. For example:
- Use a commercial EHR but build a custom patient engagement platform
- Leverage third-party analytics tools but develop bespoke dashboards
This model offers flexibility and control while accelerating development.
Scalability and Modularity Principles
A scalable stack must grow in capacity, complexity, and functionality as needs evolve. Key principles include:
Modularity
- Adopt microservices or containerized architectures
- Use loosely coupled systems to isolate failures and allow independent updates
- Leverage modular data pipelines for analytics and AI
Elastic Scalability
- Choose cloud-native platforms with auto-scaling
- Ensure database scaling capabilities (horizontal and vertical)
- Implement stateless applications where possible
Future-Readiness
- Support for emerging protocols and APIs
- Expandability for new care models (e.g., remote patient monitoring, AI triage)
- Built-in observability and monitoring tools
Cost Forecasting and Vendor Lock-in Risks
Cost Forecasting
Healthcare organizations must understand not just the upfront costs, but the total cost of ownership (TCO). Elements to include:
- Licensing and subscription fees
- Customization and integration expenses
- Training and onboarding costs
- Long-term maintenance and support
- Cloud consumption and bandwidth usage
TCO modeling should also account for indirect savings (e.g., efficiency gains, reduced readmissions) and risk mitigation (e.g., avoidance of compliance penalties).
Vendor Lock-in
Vendor lock-in can limit flexibility and innovation. To mitigate:
- Choose vendors with open standards (FHIR, HL7)
- Insist on data export and portability features
- Avoid proprietary scripting languages or tightly coupled ecosystems
- Negotiate clear SLAs and exit clauses
Long-term planning should include a vendor exit strategy, migration roadmaps, and an internal knowledge transfer plan.
Selecting the right healthcare tech stack is not a one-time decision but an evolving strategy. Balancing compliance, integration, scalability, and cost is essential to ensure that the stack serves both immediate project needs and long-term organizational goals. By applying the principles outlined here, healthcare leaders can reduce risk, accelerate innovation, and build resilient digital infrastructures.
Case Studies: Real-World Technology Stacks
Understanding real-world implementations of healthcare technology stacks helps bridge the gap between theory and practice. This section examines three diverse examples—a mid-sized hospital, a national telehealth startup, and an AI diagnostics firm. Each case highlights architectural choices, key tools, integration challenges, and lessons learned.
Example 1: Mid-Sized U.S. Hospital System
Overview
This 300-bed hospital system with multiple outpatient clinics embarked on a digital transformation initiative to modernize its legacy infrastructure, improve interoperability, and adopt population health tools.
Technology Stack
- Infrastructure: Hybrid cloud with Microsoft Azure + on-prem data center for sensitive systems
- Data: SQL Server for structured data; Azure Data Lake for long-term storage
- Integration: HL7 and FHIR interfaces using InterSystems HealthShare
- Applications: Epic EHR, Nuance Dragon for voice-enabled charting, a custom patient portal
- Analytics: Tableau dashboards, predictive readmission models via Azure ML Studio
- Security: Okta for SSO, Veeam for backups, SentinelOne for endpoint protection
Decision Rationale
- Hybrid cloud balanced modernization and regulatory control
- Epic ensured deep clinical functionality and vendor ecosystem support
- Azure ML enabled experimentation with low entry cost
Lessons Learned
- Interfacing Epic with other applications required significant customization
- Training clinicians on voice tools took longer than expected but yielded productivity gains
- Data governance committees proved vital to ensure data quality across multiple facilities
Example 2: National Telehealth Startup
Overview
This fast-scaling telehealth provider offers virtual primary and urgent care nationwide, servicing over 500,000 patients annually. The organization needed a scalable, cloud-native stack to support real-time interactions and mobile-first experiences.
Technology Stack
- Infrastructure: AWS (EC2, Lambda, S3, CloudFront)
- Data: Amazon Aurora + MongoDB for hybrid workloads
- Integration: Redox engine for EHR interoperability with major health systems
- Applications: React Native mobile app, Twilio for secure video, Stripe for payments
- Analytics: Mixpanel for engagement analytics; Redshift for clinical trend analysis
- Security: Auth0 for OAuth2 login, AWS WAF and GuardDuty for protection
Decision Rationale
- Full serverless stack ensured elasticity and reduced ops overhead
- Redox accelerated integration without requiring internal HL7 expertise
- Open APIs enabled modular and iterative feature releases
Lessons Learned
- Managing video quality across varied patient bandwidth was challenging
- Real-time integration with external pharmacy systems required custom adapters
- Continuous user feedback loops informed UX improvements
Example 3: AI-Driven Diagnostics Firm
Overview
This startup uses computer vision models to assist radiologists in detecting early-stage abnormalities in X-rays and MRIs. It operates under FDA oversight and partners with diagnostic centers worldwide.
Technology Stack
- Infrastructure: Google Cloud Platform (GCP), GPUs via AI Platform
- Data: DICOM images stored in Cloud Storage; BigQuery for structured metadata
- Integration: Custom FHIR bridge + PACS integration for hospital connectivity
- Applications: AI inference engine built in TensorFlow and served via Flask APIs
- Analytics: In-house model monitoring dashboards; MLflow for model lifecycle tracking
- Security: HIPAA-compliant environment, VPC Service Controls, encrypted image storage
Decision Rationale
- GCP offered specialized support for AI/ML workflows and imaging
- Regulatory-ready architecture reduced FDA approval timelines
- PACS integration allowed seamless diagnostic workflow inclusion
Lessons Learned
- Bias mitigation required active dataset curation across diverse populations
- Latency of cloud inference was improved via regional model serving clusters
- Auditable AI explanations were crucial for radiologist adoption and regulatory filing
These case studies underscore the importance of customizing the technology stack to align with organizational scale, function, and regulatory exposure. Whether enabling AI-driven diagnostics or supporting hundreds of thousands of virtual visits, the foundational principles of scalability, compliance, and integration remain constant.
Future Outlook: Where Healthcare Stacks Are Headed
As digital transformation in healthcare matures, the future of technology stacks is moving toward greater platformization, deep interoperability, and native AI integration. The coming decade will redefine not only how systems are built, but how care is delivered, accessed, and optimized.
Platformization
Healthcare organizations are increasingly adopting comprehensive platforms that integrate multiple functionalities—clinical, administrative, operational—into a unified environment. Two leading examples include:
Salesforce Health Cloud
- Provides a 360-degree patient view combining EHR data, social determinants of health (SDoH), and engagement tools.
- Enables care coordination, remote case management, and CRM-driven workflows.
- Extensible via AppExchange and robust API integrations.
Microsoft Cloud for Healthcare
- Offers tools for patient engagement, care coordination, and health data analytics.
- Built on Azure, it integrates with Microsoft Teams for telehealth and Dynamics 365 for CRM.
- Includes compliance-ready frameworks for HIPAA and other standards.
These platforms allow healthcare organizations to reduce reliance on fragmented systems and instead operate within scalable, secure, and customizable ecosystems.
Unified Health Records
Fragmentation of patient data across systems and providers remains one of healthcare’s biggest challenges. The future stack will aim to create longitudinal health records that unify:
- EHR and EMR data
- Lab results, imaging, genomics
- Wearable and IoT health metrics
- Claims and billing data
This unified record will enable:
- Seamless care coordination across providers and settings
- Personalized treatment plans informed by a holistic data view
- Reduced administrative burden and duplication
Emerging standards like HL7 FHIR and initiatives like Apple Health Records and Google Health are laying the groundwork for interoperable, patient-controlled data models.
Interoperable Ecosystems
Rather than monolithic systems, future stacks will prioritize modular and interoperable ecosystems where services can be mixed, matched, and reused across applications. This shift will be driven by:
- API-first development
- Standard data protocols (FHIR, OpenEHR)
- Vendor-neutral middleware and open-source tools
Governments and consortiums are pushing for regional and global data exchange frameworks. For instance:
- TEFCA in the U.S. (Trusted Exchange Framework and Common Agreement)
- EHDS in the EU
These efforts aim to standardize how data moves across platforms and borders, fostering better research, outcomes tracking, and public health planning.
AI-Native Stack Evolution
AI is evolving from a bolt-on capability to a foundational element of healthcare IT architecture. AI-native stacks will:
- Include built-in model orchestration, monitoring, and retraining pipelines
- Support low-latency inferencing (on edge or in cloud)
- Integrate explainability and bias detection by default
Examples of such stacks include:
- Google Vertex AI for scalable model management and deployment
- NVIDIA Clara for imaging AI and edge inferencing
- Amazon HealthLake for structured data analysis and ML training
Healthcare AI will move beyond diagnostics into areas such as:
- Clinical workflow automation
- Personalized treatment recommendation engines
- Predictive operational analytics (e.g., staffing, inventory)
This shift necessitates IT environments that are not only AI-enabled but AI-optimized—designed from the ground up for data-centric and model-centric operations.
The future of healthcare technology stacks lies in convergence: of systems, data, platforms, and intelligence. Platformization will drive simplification and extensibility. Unified records and interoperability will unlock new efficiencies and patient outcomes. And AI-native designs will push innovation to the edge of care delivery. Organizations that align early with these trends will be best positioned to lead in an increasingly connected and intelligent healthcare ecosystem.
Conclusion & Takeaways
In a landscape shaped by continuous innovation, growing patient expectations, and evolving regulatory frameworks, healthcare IT leaders must make strategic, high-stakes decisions that impact both care delivery and organizational sustainability. This guide has outlined the structural, operational, and emerging layers of the healthcare technology stack. Here, we distill the key takeaways for actionable decision-making.
Strategic Imperatives for CTOs and IT Leaders
CTOs and healthcare technology leaders must go beyond system administration—they must architect ecosystems that are secure, scalable, and innovation-ready. This involves:
- Championing Interoperability: Advocate for open standards (FHIR, HL7) and API-first solutions that allow seamless integration and future extensibility.
- Aligning Tech with Clinical Goals: Collaborate closely with clinical and operational teams to ensure that every tech initiative supports improved patient outcomes and staff productivity.
- Leading with Governance: Establish clear data stewardship policies, governance frameworks, and cybersecurity protocols to build trust and accountability.
Reducing Complexity Without Compromising Compliance
Many healthcare organizations face a tangle of legacy systems, fragmented vendors, and siloed data. Simplification should be a goal—but not at the expense of compliance or resilience. Key principles include:
- Modularity over Monoliths: Build systems using microservices or service-oriented architecture to enable targeted upgrades and agile iteration.
- Centralized Identity and Access Management: Streamline security with unified login systems, role-based access, and audit-ready workflows.
- Leverage Platform-as-a-Service (PaaS): Reduce infrastructure complexity while maintaining control over sensitive operations through compliant cloud environments.
Effective simplification enhances responsiveness and cost-efficiency while minimizing operational and legal risks.
Investing in Forward-Compatible Stacks
Future-ready stacks are designed not just to solve today’s problems but to scale with tomorrow’s opportunities. Forward compatibility requires:
- Cloud-Native Infrastructure: Enables elastic compute and storage, global reach, and disaster recovery readiness.
- AI-Ready Architecture: Supports model training, real-time inference, and embedded explainability.
- Unified Data Strategies: Ensures that structured, unstructured, and streaming data can be integrated and leveraged for analytics and automation.
- Regulatory Flexibility: Prepares for evolving laws (e.g., EHDS, TEFCA) and cross-border data governance requirements.
Technology decisions made today will dictate the agility and resilience of an organization for years to come. Leaders must prioritize investments that maintain optionality and foster long-term value creation.
Healthcare technology is no longer a support function—it is a strategic enabler of care delivery, patient engagement, and institutional growth. By understanding and actively shaping the technology stack, healthcare leaders can ensure they are not only compliant and cost-effective, but also positioned at the forefront of innovation. The imperative now is to act decisively, collaborate cross-functionally, and architect ecosystems that are as dynamic and life-saving as the care they support.
To know more about healthcare tech stack, connect with healthcare software development company – Aalpha Information Systems!