Modernizing legacy systems in healthcare is no longer optional—it is a strategic imperative. In 2026, a significant number of hospitals and payers across the U.S., EU, and APAC regions continue to rely on outdated software infrastructure: mainframe EMRs, COBOL-based billing systems, on-premises lab systems, and fragmented databases that fail to support modern clinical workflows or real-time data exchange. These legacy environments not only slow down innovation but also increase security and compliance risks, limit interoperability, and inflate operational costs.
According to HIMSS Analytics (2024), over 60% of U.S. hospitals still operate at least one critical application on legacy software that lacks cloud-readiness, modern APIs, or FHIR-based interoperability. At the same time, patients are demanding more digital-first interactions, regulators are tightening compliance mandates, and medical staff are burdened with outdated workflows. This confluence of pressures has prompted many decision-makers to ask: “How do I modernize my hospital’s old IT systems?”
Why Legacy Modernization Is Urgent in Healthcare
Legacy systems present a complex mix of technical debt, security vulnerabilities, and inefficiency. The average hospital runs between 200–300 software systems, many of which don’t talk to each other—creating fragmented data silos that hinder coordinated care. These systems often lack modern encryption, audit logging, or compliance with the latest HIPAA and GDPR protocols.
A single breach involving protected health information (PHI) now costs $10.93 million on average in the healthcare sector—higher than in any other industry (IBM, Cost of a Data Breach Report, 2024). This is partly due to the slow patching cycles and unsupported architecture typical of legacy applications. The longer an organization delays modernization, the more they compound risk—technologically, legally, and financially. This leads many executives to explore, “What are the risks of not upgrading legacy EHR software?”
Beyond risk, legacy systems also impose significant hidden costs. Outdated UI/UX forces clinicians to spend up to 45% of their day on administrative or non-clinical tasks (American Medical Association, 2023). These inefficiencies directly impact patient care and staff morale, while limiting an organization’s ability to scale or integrate with new technologies—such as AI diagnostics, telemedicine, or wearable data.
Is It Worth Modernizing EMR/EHR Platforms?
Yes—but how modernization is approached is just as critical as whether it’s pursued. Full rip-and-replace initiatives are expensive and often disruptive. In many cases, healthcare providers achieve better outcomes through modular modernization strategies: using API gateways, middleware connectors, containerization, or microservices decomposition to gradually decouple legacy systems.
A 2023 Deloitte study found that phased modernization—starting with high-risk backend systems—led to 25–40% reduction in IT operational costs over three years, with minimal service interruption. This hybrid approach allows for technical improvement while maintaining business continuity and clinician trust.
This brings up a core strategic question facing every CTO in healthcare IT: “Which is better—replace or replatform a legacy healthcare system?” The answer depends on system interdependencies, clinical workflows, risk tolerance, and available budget. Replatforming offers a less disruptive middle path in many contexts, especially when paired with strong interoperability layers (e.g., HL7 FHIR, TEFCA gateways).
A High-Level Roadmap for Healthcare IT Leaders
A structured, cross-functional approach is required for effective legacy modernization. Key phases include:
-
Assessment
-
Audit all legacy systems, dependencies, and data silos
-
Identify security vulnerabilities and compliance gaps
-
Prioritize systems based on clinical impact and risk exposure
-
-
Strategy Selection
-
Evaluate options: rehost, replatform, refactor, or replace
-
Align roadmap with regulatory deadlines (e.g., 21st Century Cures Act, TEFCA compliance)
-
Assess patient and clinician experience goals
-
-
Architecture Design
-
Adopt modular, API-first architecture
-
Use cloud services like AWS HealthLake, Azure Health Data Services, or Google Cloud Healthcare API
-
Support real-time data exchange with FHIR and SMART on FHIR protocols
-
-
Data Migration & Security
-
Map, clean, and validate legacy data
-
Encrypt data in transit and at rest; implement RBAC
-
Establish audit trails and incident response protocols
-
-
Clinician Engagement & Change Management
-
Co-design new workflows with end users
-
Roll out in stages; provide role-specific training
-
Monitor user feedback to fine-tune adoption
-
-
Pilot Programs & Iterative Deployment
-
Start with low-risk departments or services
-
Evaluate technical metrics and clinician feedback
-
Scale rollout based on real-world outcomes
-
-
Modernizing healthcare IT is urgent due to escalating compliance risks, cybersecurity threats, and patient experience expectations.
-
The decision to replace or replatform must be contextual, balancing cost, disruption, and future scalability.
-
Selective modernization strategies (e.g., FHIR-based APIs or microservices) offer high ROI and lower risk than full system overhauls.
-
Healthcare CTOs should adopt a roadmap rooted in clinical input, architectural flexibility, and phased deployment.
Market Landscape—Size, Spend & Digital Transformation Momentum (2025–2030)
The global healthcare IT sector is undergoing a significant transformation, driven by the urgent need to modernize legacy systems, enhance patient care, and improve operational efficiency. As of 2025, the market exhibits robust growth, with substantial investments directed toward both legacy system modernization and the adoption of new technologies.
Global Healthcare IT Spend Projections (2025–2030)
In 2025, the global healthcare IT market was projected to reach approximately USD 354.04 billion, with expectations to grow to USD 981.23 billion by 2032, reflecting a compound annual growth rate (CAGR) of 15.7% . This growth is fueled by factors such as the increasing demand for digital health solutions, the integration of artificial intelligence (AI) in healthcare, and the necessity to replace outdated systems.
A significant portion of this investment is allocated to modernizing legacy systems. Healthcare organizations are recognizing that outdated IT infrastructures hinder innovation and efficiency. According to Gartner, up to 75% of healthcare IT budgets are currently consumed by maintaining legacy systems . This financial burden underscores the importance of transitioning to more agile and interoperable solutions.
Breakdown of Spend: Legacy Modernization vs. Net-New Systems
The allocation of healthcare IT budgets reflects a strategic shift toward modernization:
-
Legacy Modernization: Approximately 60–70% of IT budgets are dedicated to updating existing systems. This includes efforts such as replatforming electronic health records (EHRs), implementing interoperability standards like FHIR, and enhancing cybersecurity measures.
-
Net-New Systems: The remaining 30–40% is invested in new technologies, including AI-driven diagnostics, telehealth platforms, and patient engagement tools. These investments aim to improve patient outcomes and streamline healthcare delivery.
This distribution highlights the dual focus of healthcare organizations: addressing the immediate challenges posed by legacy systems while also embracing innovative solutions to meet future demands.
Regional Growth Trends: U.S., EU, and APAC
-
United States
The U.S. healthcare IT market is leading in terms of investment and innovation. In 2026, the market is valued at USD 354.04 billion, with projections to reach USD 981.23 billion by 2032 . Factors contributing to this growth include federal incentives for EHR adoption, a strong emphasis on patient-centered care, and the integration of advanced technologies.
-
European Union
The EU is experiencing steady growth in healthcare IT, driven by regulatory mandates and the need for cross-border interoperability. The market is expected to grow at a CAGR of 5.6% from 2022 to 2030, with significant investments in finance, billing, and inventory management systems . Countries like the UK and Germany are at the forefront, implementing national digital health strategies to modernize their healthcare infrastructures.
-
Asia-Pacific (APAC)
APAC represents the fastest-growing region in the healthcare IT sector. The market is projected to expand from USD 35.40 billion in 2024 to USD 84.23 billion by 2031, achieving a CAGR of 11.4% . This growth is propelled by government initiatives, increasing healthcare expenditures, and the adoption of telemedicine and mobile health solutions. Countries like China and India are investing heavily in digital health infrastructure to improve access and quality of care.
Digital Transformation Momentum
The momentum for digital transformation in healthcare is accelerating, with organizations prioritizing the modernization of IT systems to enhance efficiency and patient care. Key drivers include:
-
Regulatory Compliance: Adherence to regulations such as HIPAA and GDPR necessitates robust IT systems capable of ensuring data privacy and security.
-
Patient-Centric Care: There is a growing demand for personalized healthcare experiences, which requires the integration of advanced analytics and interoperable systems.
-
Technological Advancements: The adoption of AI, machine learning, and cloud computing is transforming healthcare delivery, enabling predictive analytics and remote patient monitoring.
These factors underscore the importance of modernizing legacy systems to remain competitive and meet the evolving needs of patients and healthcare providers.
-
“How big is the healthcare IT modernization market in 2025?”
The global healthcare IT market was projected to reach USD 354.04 billion in 2025, with a significant portion allocated to modernizing legacy systems. -
“What is the projected growth of healthcare IT spending by 2030?”
Healthcare IT spending is expected to grow to USD 981.23 billion by 2032, reflecting a CAGR of 15.7%. -
“Which regions are leading in healthcare IT investments?”
The United States leads in healthcare IT investments, followed by the European Union and the Asia-Pacific region, each exhibiting significant growth driven by technological adoption and regulatory initiatives.
The healthcare IT landscape in 2026 is marked by a concerted effort to modernize legacy systems and embrace digital transformation. Organizations are investing heavily to enhance interoperability, ensure regulatory compliance, and improve patient outcomes. As the market continues to evolve, staying informed about regional trends and technological advancements will be crucial for stakeholders aiming to navigate this dynamic environment.
Defining the Problem: What Are Legacy Systems in Healthcare?
Legacy systems are entrenched throughout healthcare—often invisible to patients, yet deeply embedded in the operational core of hospitals, laboratories, insurance providers, and public health institutions. In a sector where continuity is critical and stakes are high, the tolerance for disruption has kept outdated technologies in active use far longer than in other industries. However, the hidden cost of these systems is becoming increasingly difficult to ignore.
Defining Legacy Systems in a Healthcare Context
In healthcare IT, a “legacy system” refers to any application or technology that:
-
Is no longer actively developed or supported by its original vendor
-
Relies on outdated programming languages (e.g., COBOL, MUMPS)
-
Operates on obsolete or non-cloud-native infrastructure
-
Lacks modern interoperability (e.g., limited to HL7 v2, without FHIR support)
-
Cannot meet today’s data privacy, auditability, or security standards
Common examples include:
-
On-premises electronic medical records (EMRs) running on outdated database architectures
-
COBOL-based billing and financial platforms still used in some U.S. hospital networks
-
Custom-built laboratory information management systems (LIMS) that predate commercial SaaS alternatives
-
HL7-only messaging interfaces that lack the flexibility of modern FHIR or RESTful APIs
-
The Veterans Health Administration’s VistA system, a decentralized EHR originally developed in the 1970s, which remains in partial use despite efforts to replace it with Cerner Millennium
These systems were often built to solve a narrow set of needs in an era of paper records and local infrastructure. Over time, they were extended and patched—resulting in deeply customized environments that are resistant to change.
Why Are Legacy Systems Still Used in Hospitals?
Despite the known drawbacks, legacy systems persist in healthcare due to a mix of institutional inertia, financial constraints, and operational risk aversion. Many decision-makers ask, “Why are legacy systems still used in hospitals?” The answer lies in four major factors:
-
High Switching Costs
Replacing a core system such as an EHR or LIS is capital-intensive. A full-scale modernization project can cost tens of millions of dollars for even mid-sized hospital networks—particularly when accounting for downtime, staff training, and data migration complexities. -
Deep Integration with Clinical Workflows
Many legacy systems are deeply embedded in daily routines, from radiology reporting to pharmacy inventory management. Unwinding them without disrupting patient care is difficult and sometimes politically sensitive. -
Regulatory Constraints and Fear of Compliance Risks
Ironically, compliance itself can hinder modernization. Many older systems are so well documented and audited that replacing them introduces risk. As a result, healthcare organizations opt to “wrap” legacy systems with newer technologies rather than replace them outright. -
Limited Vendor Support for Migration
Some systems are proprietary, and the vendors offer no viable upgrade path. In other cases, the original developers are long gone, making the codebase effectively unmaintainable but irreplaceable without a full rewrite.
Risks Associated with Legacy Healthcare Systems
The continued use of legacy systems creates both immediate and long-term risks that impact every layer of a healthcare organization.
1. Security Vulnerabilities
Legacy applications often lack support for modern encryption protocols (TLS 1.3, AES-256), making them vulnerable to breaches. They also frequently miss critical patch updates or operate on unsupported operating systems. According to the IBM X-Force Threat Intelligence Index (2024), healthcare ranked as the most targeted industry for ransomware attacks, with legacy IT cited as a major entry point.
2. Compliance Gaps
Modern regulations such as HIPAA, GDPR, and the Cures Act demand transparency, audit trails, role-based access control, and data portability. Legacy systems often fail to meet these standards. For example, many older EHRs do not support APIs that allow patients to access or transfer their medical data in real-time.
3. High Maintenance and Operational Costs
Gartner estimates that up to 75% of IT budgets in hospitals are consumed by maintaining legacy systems. These platforms often require expensive hardware, highly specialized (and scarce) IT staff, and manual workarounds for tasks that modern systems automate natively.
4. Inability to Scale or Innovate
Legacy systems are often monolithic and inflexible. They cannot support modern capabilities such as cloud-native computing, AI diagnostics, or telehealth integration. This stalls innovation and limits the organization’s ability to respond to new care models or public health challenges.
Real-World Examples of Legacy Healthcare Systems
-
VistA (Veterans Health Information Systems and Technology Architecture)
Developed in the 1970s by the U.S. Department of Veterans Affairs, VistA remains in use in parts of the VA system despite long-running efforts to replace it. Its decentralized architecture, written in MUMPS, makes integration with modern platforms difficult. -
IBM Mainframe EHRs
Some U.S. health systems still operate EMRs on IBM mainframe systems using languages like COBOL or JCL. While stable, these systems are costly to maintain and lack modern data interoperability features. -
Custom LIMS in Public Health Labs
Public health labs in low-to-middle-income countries and some state-run facilities in the U.S. continue to use 1990s-era LIMS developed in-house. These systems lack web-based UIs and cannot interface with national disease surveillance networks.
Drivers of Modernization in Healthcare
The urgency to modernize healthcare IT systems in 2026 is no longer theoretical—it’s driven by a combination of hard regulatory mandates, escalating security threats, evolving patient expectations, and increasing clinician dissatisfaction. Each of these forces is compounding the need for CIOs, CTOs, and digital transformation leaders to re-evaluate their legacy infrastructure and transition toward agile, compliant, and interoperable systems.
For many decision-makers, the question is no longer if modernization is necessary but what’s driving healthcare IT modernization in 2026?
1. Regulatory Pressures and Mandates
Global regulatory bodies have significantly intensified their expectations for data accessibility, interoperability, and patient rights. Compliance is now a key driver of digital transformation.
a. ONC & 21st Century Cures Act (U.S.)
The U.S. Office of the National Coordinator for Health IT (ONC) mandates, particularly those emerging from the 21st Century Cures Act, are fundamentally reshaping EHR modernization priorities. The Act enforces:
-
Patient access to digital health data through standardized APIs (HL7 FHIR)
-
Prevention of information blocking, requiring systems to facilitate data sharing
-
Developer certification standards for HIT vendors
The implications are clear: legacy systems that cannot expose APIs or support FHIR will be non-compliant.
b. HIPAA and HITECH
HIPAA is evolving beyond traditional perimeter security. The updated guidelines emphasize:
-
Breach prevention and zero-trust architecture
-
Advanced audit logging
-
Identity-based access and encryption protocols
Legacy EHRs that lack audit trails or cannot log access events in real-time are increasingly seen as liabilities under HIPAA audits.
c. GDPR and Global Data Sovereignty Laws
For providers operating in the EU or handling data from EU citizens, GDPR mandates require:
-
Explicit consent for data usage
-
Right to data portability
-
Encryption and breach notification policies
Healthcare organizations using outdated systems incapable of fulfilling GDPR data requests—such as exporting full patient records on demand—face legal and reputational exposure.
2. Escalating Security Threats
Healthcare remains one of the most targeted industries for cyberattacks due to the value of PHI (Protected Health Information) and typically weak infrastructure.
a. Ransomware Epidemic
Ransomware attacks on hospitals have surged by more than 90% between 2021 and 2024 (SonicWall Cyber Threat Report, 2024). Many attacks exploit:
-
Legacy operating systems (e.g., Windows Server 2008)
-
Hardcoded credentials
-
Unpatched EHR or billing software
Healthcare breaches now cost an average of $10.93 million per incident (IBM, 2024). Outdated systems without endpoint detection, encryption at rest, or continuous patching processes are prime entry points for threat actors.
b. PHI Leaks and Insider Threats
Legacy applications often lack multi-factor authentication, audit trails, or least-privilege access controls—making it difficult to detect or prevent insider misuse. In cloud-native systems, by contrast, administrators can centrally manage user permissions, instantly revoke access, and detect anomalies using AI-based behavioral monitoring.
Modernization enables implementation of zero-trust security frameworks, which are rapidly becoming standard under NIST guidelines.
3. Patient Demand for Digital-First Healthcare Experiences
Modern patients expect healthcare to match the convenience and personalization of banking, retail, and entertainment platforms. Legacy systems are structurally incapable of supporting this experience.
a. On-Demand Access to Records
Patients increasingly expect to access lab results, appointment histories, and prescriptions from mobile apps or web portals. EHRs must now support real-time data access via SMART on FHIR apps, as required under U.S. rules. Systems without FHIR APIs or patient portals are effectively obsolete.
b. Omnichannel Engagement
Text reminders, digital check-ins, asynchronous chat with care teams, and remote consultations are becoming standard. This requires not only front-end innovation but also back-end modernization to ensure secure, interoperable workflows.
c. Personalized and AI-Augmented Care
Many new platforms use patient-reported data, wearable metrics, and historical EMR data to personalize care recommendations. Legacy systems that silo this data or rely on flat-file exports prevent the use of AI in clinical decision support.
4. Workforce Efficiency and Clinician Burnout
Clinician dissatisfaction with outdated health IT systems has reached a tipping point. The American Medical Association reports that over 50% of physician burnout is tied to administrative burden—often exacerbated by poorly designed EHR interfaces and fragmented data access.
a. Click Fatigue and Workflow Disruption
Legacy EHRs often require redundant data entry, screen-switching, or paper-based workarounds. In contrast, modern systems use task automation, role-based interfaces, and integration with clinical decision support to reduce clicks and increase throughput.
b. Talent Drain in IT and Clinical Ops
Hospitals are also struggling to retain IT staff familiar with COBOL, MUMPS, and AS/400 environments. Recruiting engineers for these systems is costly and unsustainable. Newer platforms based on modern stacks (e.g., Python, React, Node.js) are more appealing to developers and easier to maintain.
c. Integrated Decision Support
Modern platforms integrate AI to suggest diagnosis, flag abnormal labs, or recommend coding—all in real time. This significantly reduces cognitive load on physicians. Legacy systems, by contrast, lack the infrastructure for real-time inference engines or API-driven ML integrations.
What’s Driving Healthcare IT Modernization?
-
Mandatory regulations such as ONC’s API requirements and GDPR’s portability laws are forcing hospitals to rethink outdated IT systems.
-
Security vulnerabilities, including unpatched operating systems and lack of zero-trust design, are making legacy infrastructure untenable.
-
Patients expect digital-first services—mobile access to records, real-time messaging, and personalized care pathways.
-
Clinicians and IT teams are burning out under the weight of inefficient systems, driving institutional momentum toward modern platforms.
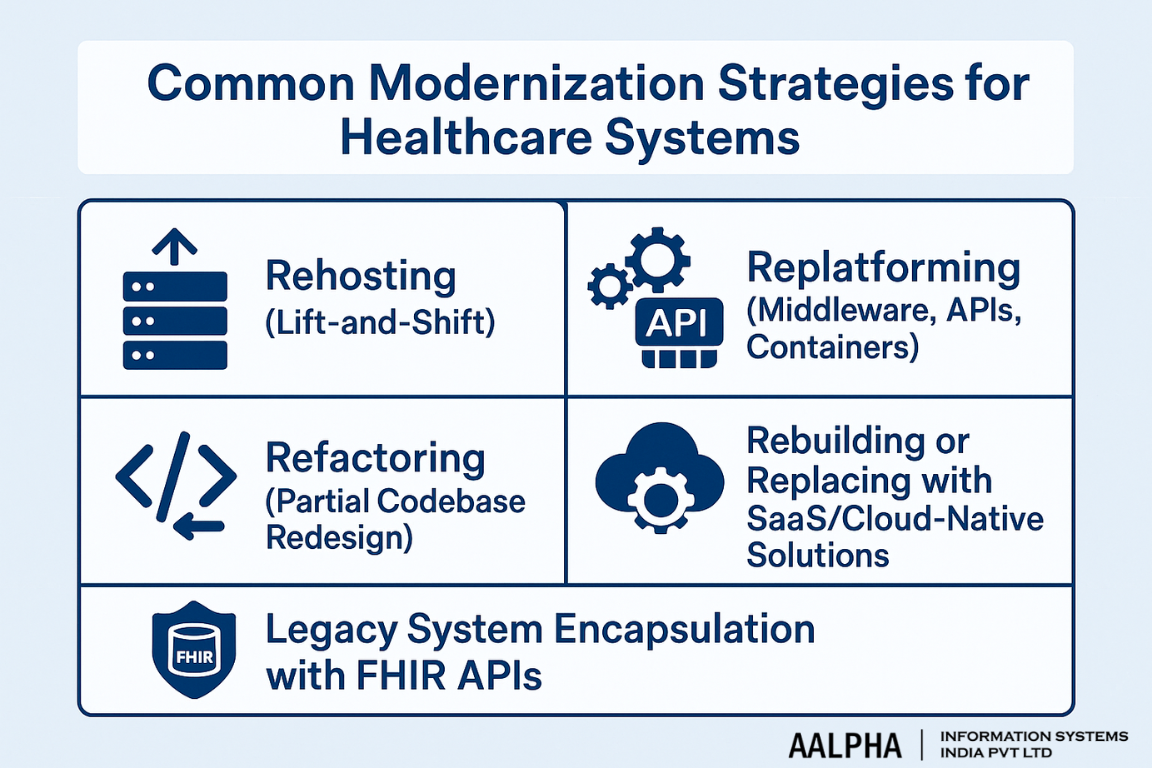
Common Modernization Strategies for Healthcare Systems
Modernizing healthcare IT infrastructure is complex, high-stakes, and often politically sensitive. Yet given the regulatory mandates, cybersecurity risks, and operational inefficiencies associated with outdated platforms, many health systems now face a pivotal decision: How to modernize a legacy healthcare system without full replacement?
Fortunately, a range of incremental strategies—rehosting, replatforming, refactoring, or encapsulating legacy systems with modern interfaces—allows organizations to modernize without disrupting clinical workflows or risking compliance. The right approach depends on budget, system criticality, and long-term strategic goals.
1. Rehosting (Lift-and-Shift)
Definition:
Rehosting moves an existing application from on-premises infrastructure to a cloud environment without altering its core codebase or architecture.
Use Case in Healthcare:
Rehosting is commonly used for legacy EHR systems, billing platforms, or imaging archives that run on aging hardware but are otherwise stable. For example, an on-prem EHR hosted on outdated servers can be moved to a private AWS or Azure environment to improve scalability, availability, and disaster recovery capabilities.
Benefits:
-
Minimal code change required
-
Faster implementation (typically weeks or months)
-
Reduces infrastructure maintenance burden
Limitations:
-
Does not solve software limitations or interoperability issues
-
Still carries forward inefficiencies and security flaws from the original architecture
2. Replatforming (Middleware, APIs, Containers)
Definition:
Replatforming involves upgrading the runtime platform (e.g., OS, database, infrastructure stack) while introducing minimal changes to the codebase. It often includes containerization (e.g., using Docker) or deploying middleware/APIs to improve integration.
Use Case in Healthcare:
A hospital may continue using a legacy LIS but deploy API middleware such as Mirth Connect, Redox, or Health Samurai to expose the data via HL7/FHIR. This allows integration with newer platforms—such as analytics dashboards, mobile apps, or patient portals—without replacing the core system.
Benefits:
-
Adds extensibility and interoperability to legacy apps
-
Enhances security and performance through containerization
-
Supports gradual modernization of individual modules
Limitations:
-
Middleware introduces additional complexity
-
May require a DevOps function to manage container orchestration (e.g., Kubernetes)
3. Refactoring (Partial Codebase Redesign)
Definition:
Refactoring means modifying the internal structure of code without changing its external behavior. It improves maintainability, performance, and modularity.
Use Case in Healthcare:
A radiology reporting system originally written in Visual Basic or Java 6 may be partially refactored to support RESTful APIs, replace obsolete libraries, or move to modern frameworks like Spring Boot or .NET Core.
Benefits:
-
Reduces technical debt and security risk
-
Prepares legacy apps for cloud-native deployment
-
Enables unit testing, CI/CD, and DevOps automation
Limitations:
-
Higher complexity and cost than replatforming
-
Requires skilled development teams with both legacy and modern stack expertise
4. Rebuilding or Replacing with SaaS/Cloud-Native Solutions
Definition:
Rebuilding involves rewriting the entire application from scratch using modern technologies and architectures. Replacing refers to adopting a third-party SaaS or cloud-native solution.
Use Case in Healthcare:
Replacing a custom-built on-prem EMR with a cloud-native system like Epic-as-a-Service, Athenahealth, or Cerner on Oracle Cloud. In public health, rebuilding could involve developing a modular disease surveillance platform using Node.js and FHIR-compliant APIs.
Benefits:
-
Eliminates legacy limitations entirely
-
Enables modern UX, mobile-first design, and real-time analytics
-
Reduces future maintenance and tech debt
Limitations:
-
High upfront cost
-
Long timelines (12–36 months)
-
Disruptive unless planned carefully with phased rollout and training
Key Insight:
Many health systems pursue this strategy only after incremental modernization efforts fail to deliver necessary improvements in scalability, compliance, or user satisfaction.
5. Legacy System Encapsulation with FHIR APIs
Definition:
Encapsulation involves wrapping a legacy system in an interoperability layer—usually an API gateway or FHIR proxy—so modern applications can interact with it securely and consistently.
Use Case in Healthcare:
A legacy EHR that supports only HL7 v2 messages can be encapsulated using an adapter that translates incoming FHIR requests into HL7 v2 internally. This allows the EHR to support SMART on FHIR apps or national health information exchanges (e.g., TEFCA in the U.S.) without re-engineering the core system.
Benefits:
-
Allows regulatory compliance (e.g., 21st Century Cures Act) without code rewrite
-
Supports mobile apps, external integrations, and data sharing
-
Lower cost and faster to deploy than full rebuild
Limitations:
-
Maintains underlying inefficiencies
-
May require constant patching as standards evolve
Decision Framework: What Strategy to Choose and When
Healthcare leaders often struggle with selecting the right modernization path. Here’s a simplified decision framework:
Decision Criteria | Best Fit Strategy |
Minimal downtime required | Rehosting |
Need better integration with new systems | Replatforming or Encapsulation |
Reducing tech debt and improving performance | Refactoring |
Enabling new capabilities and future-proofing | Rebuilding or SaaS Replacement |
Budget constraints with urgent compliance need | Encapsulation + Middleware |
Strategic Considerations:
-
Short-Term Compliance Need? → Prioritize encapsulation and API middleware.
-
Long-Term Cloud Strategy? → Use replatforming as a bridge to SaaS or rebuild.
-
Severe User Frustration with UX/UI? → Refactor or rebuild with clinician input.
-
Multiple Sites with Legacy Heterogeneity? → Consider phased replatforming by department or function.
Case-in-Point Example: Hybrid Modernization at a U.S. Health Network
A regional hospital group in the Midwest had a mix of 12-year-old radiology systems, a COBOL-based claims processing module, and a homegrown EMR. Instead of replacing everything at once:
-
They containerized the billing system to improve uptime and deployed it on AWS.
-
They refactored the radiology reporting tool to enable HL7-to-FHIR conversion.
-
They encapsulated the EMR using Redox API gateways to support patient mobile apps.
Result: Within 18 months, they achieved TEFCA compliance, reduced IT OPEX by 32%, and reported a 20% drop in clinician complaints about system slowness or fragmentation.
Modern Tech Stack for Healthcare IT
Modernizing healthcare infrastructure requires more than simply replacing legacy systems. It involves architecting a modular, interoperable, secure, and scalable healthcare tech stack that supports modern clinical workflows, real-time data exchange, AI integration, and compliance with evolving regulations. Whether building clinician-facing portals, mobile patient apps, or EHR platforms, healthcare organizations in 2025 must choose technologies that balance usability, reliability, and extensibility.
So, what is the best tech stack for building modern healthcare systems? The answer depends on use case, budget, compliance requirements, and existing architecture—but certain tools and frameworks have become the standard for high-performance digital health platforms.
1. Frontend Frameworks for Clinician and Patient Interfaces
Modern frontend development in healthcare must emphasize performance, accessibility, responsive design, and tight integration with backend APIs (often FHIR or HL7-based). The two dominant JavaScript frameworks are:
a. React.js
-
Use Cases: Patient portals, clinician dashboards, EMR interfaces, mobile-first applications
-
Why React?
-
Strong ecosystem (React Query, Redux, Next.js)
-
Component-based architecture for reusable design systems
-
Easy integration with FHIR APIs and GraphQL for dynamic data rendering
-
Example: Many healthcare startups now build their core apps using React paired with Material UI or Tailwind for HIPAA-compliant, responsive interfaces.
b. Angular
-
Use Cases: Enterprise-scale hospital systems and internal healthcare admin panels
-
Why Angular?
-
Built-in dependency injection and state management
-
Preferred by some government healthcare IT teams for structure and TypeScript support
-
Good for large, multi-role SPAs (e.g., clinician, billing, admin views)
-
2. Backend Technologies: Secure, Scalable, Maintainable
Backend services in healthcare must be secure-by-design, API-first, and horizontally scalable. The following are popular in healthcare SaaS and internal hospital systems:
a. Node.js
-
Strengths: Real-time communication (e.g., live chat with patients), lightweight services, API development
-
Why it’s used: Non-blocking I/O enables fast data flows from EHRs, labs, or devices
b. Python
-
Strengths: Data pipelines, AI/ML integration, health analytics
-
Libraries: FastAPI (for APIs), Django (for admin portals), Pandas/Numpy for data preprocessing
-
Why it’s used: Python is dominant in AI-driven diagnostics, clinical decision support, and health research platforms
c. .NET Core
-
Strengths: Enterprise-grade systems, Windows interoperability, integration with HL7 services
-
Why it’s used: Popular among hospital IT teams and vendors modernizing legacy .NET Framework apps; strong security and identity control via Microsoft Azure AD
Example: A U.S.-based hospital group uses .NET Core microservices to manage patient intake, physician scheduling, and insurance workflows—linked via internal APIs.
3. Data Layer: Structured, Interoperable, and Scalable
Healthcare data is complex, high-volume, and subject to regulatory constraints. Choosing the right database architecture is critical.
a. PostgreSQL
-
Why it’s used: Open-source, ACID-compliant, supports JSONB for semi-structured data (ideal for FHIR resources), strong indexing and query optimization
-
Use Cases: Storing patient records, audit logs, medical history
b. Snowflake
-
Why it’s used: High-performance analytics engine for large-scale medical datasets, seamless integration with BI tools
-
Use Cases: Population health analytics, predictive modeling, claims data aggregation
c. FHIR Stores
-
Examples: Google Cloud FHIR Store, Microsoft Azure FHIR Server
-
Why it’s used: Enables FHIR-native CRUD operations, integrated access controls, versioning, and compliance logging
-
Use Cases: Real-time health record exchange, SMART on FHIR apps, TEFCA compliance
d. HL7 Integrations
-
Purpose: For systems still using HL7 v2 or v3 messages (e.g., labs, radiology)
-
Tools: Mirth Connect for message transformation and routing
4. Middleware & API Gateways: Enabling Interoperability
Middleware layers bridge the gap between old and new systems, allowing standardized data exchange, audit trails, and modular service orchestration.
a. Mirth Connect
-
Purpose: HL7/FHIR transformation, message routing, legacy system integration
-
Deployment: On-prem or containerized
-
Use Case: Translating lab results from HL7 v2 to FHIR bundles for EHR use
b. Redox
-
Purpose: Cloud-based API gateway for hospitals and vendors
-
Why it’s used: Pre-built interfaces for common EHRs like Epic, Cerner, Allscripts; handles authentication, error management, and retries
-
Use Case: SaaS healthtech apps integrating with hospital EMRs across vendors
c. Health Samurai (Aidbox)
-
Purpose: FHIR-first backend and database platform
-
Why it’s used: Great for building FHIR-native applications, patient portals, or digital front doors with full FHIR compliance
-
Use Case: Organizations building TEFCA-ready services
5. Cloud Platforms Optimized for Healthcare
Healthcare cloud providers offer specialized tools for compliance, identity, observability, and data standardization.
a. AWS HealthLake
-
What it offers: FHIR-native data store, medical NLP for unstructured text, analytics pipelines, HIPAA-eligible services
-
Use Case: Converting radiology reports and clinical notes into searchable FHIR resources
b. Google Cloud Healthcare API
-
What it offers: HL7, FHIR, and DICOM ingestion endpoints; integrated BigQuery for analytics
-
Use Case: Integrating imaging, genomics, and EHR data into a single analytics layer
c. Azure Health Data Services
-
What it offers: FHIR server, IoMT (Internet of Medical Things) integration, strong identity and access control via Azure Active Directory
-
Use Case: Managing consent and data access at scale in multisite hospital networks
Example: NHS trusts in the UK often use Azure for secure identity management and FHIR-compliant data exchange between trusts and national systems.
Stack Composition Based on Use Case
Use Case | Frontend | Backend | Database | Middleware | Cloud |
Patient Mobile App | React | Node.js | PostgreSQL | Redox | AWS HealthLake |
Internal Clinical Dashboard | Angular | .NET Core | SQL Server/FHIR | Mirth Connect | Azure Health Data Services |
AI-Powered Diagnostics Platform | React | Python (FastAPI) | Snowflake | Health Samurai | Google Cloud Healthcare API |
Claims + Billing Modernization | React | Node.js/.NET | PostgreSQL | Redox or Mirth | Azure or AWS |
Migration Planning: Technical, Financial & Operational Readiness
Migrating from legacy systems to a modern healthcare IT infrastructure is a high-impact endeavor that demands meticulous planning, clinical engagement, financial foresight, and strong execution. Whether the goal is to move an aging EHR to a cloud-native solution, replace a homegrown LIMS, or unify disparate systems across hospital networks, successful modernization hinges on cross-functional alignment and phased rollout.
A critical question for healthcare executives is: How to plan a successful healthcare system migration?
The answer lies in a structured, risk-aware, and clinically grounded migration plan.
1. Stakeholder Alignment and Clinical Input
A common cause of migration failure is the lack of alignment between technical teams and clinical users. Healthcare IT is not just about software—it’s about workflow enablement, clinician productivity, and patient safety.
Key Stakeholders to Involve:
-
Clinical leadership (CMO, CNO, department heads): to validate workflow fit and prioritize features
-
Health IT leadership (CTO, CIO, enterprise architects): to define infrastructure, integration, and cloud strategy
-
Compliance and legal (HIPAA officer, DPO): to review patient data handling and audit compliance
-
Operations and scheduling: to coordinate rollout timing with clinical workloads
-
Vendor teams (EHR, middleware, analytics): to define cutover and integration points
Recommendation:
Form a Migration Task Force early in the project lifecycle to guide decisions and troubleshoot bottlenecks across clinical, technical, and administrative domains.
2. Data Mapping, Cleansing & Interoperability Requirements
One of the most resource-intensive aspects of system migration is managing data migration, especially in healthcare where data is high-volume, fragmented, and regulated.
a. Data Mapping & Transformation
-
Inventory all datasets across systems: EHR, LIMS, PACS, billing, CRM, wearable integrations
-
Map data fields from source schema (e.g., HL7 v2 messages, SQL records) to the target format (e.g., FHIR resources, JSON payloads)
-
Use ETL tools such as Talend, Apache NiFi, or custom pipelines to automate this process.
b. Data Cleansing
Legacy records often include duplicate patients, inconsistent codes (ICD-9/10), and outdated clinical terminologies. Cleansing should involve:
-
De-duplication
-
Standardizing formats (e.g., SNOMED CT, LOINC)
-
Flagging incomplete or corrupt records
c. Interoperability Requirements
Modern systems must communicate across vendor boundaries. Ensure:
-
FHIR-readiness (structured data + RESTful APIs)
-
HL7 v2/v3 compatibility for legacy lab, imaging, and pharmacy interfaces
-
Consent and identity management for cross-platform access
3. Risk Mitigation: Downtime, Data Loss, Clinician Training
System migrations introduce operational risk. The most successful transitions have well-rehearsed mitigation plans.
a. Downtime Management
-
Use cutover windows during low-traffic periods (e.g., nights, weekends)
-
Keep read-only access to legacy system post-migration for reference
-
Deploy rollback protocols in case of error during go-live
b. Data Loss Prevention
-
Implement a parallel validation environment to test migrated data for completeness and accuracy
-
Run reconciliation reports (e.g., lab results, medication lists) before switching production systems
-
Retain backups of original systems in cold storage for legal retention
c. Clinician Training
-
Use role-specific onboarding modules for physicians, nurses, and admin staff
-
Provide live support teams on-site for the first 2–4 weeks post-migration
-
Roll out simulation sandboxes so clinicians can practice workflows without patient impact
4. Budgeting: CapEx vs. OpEx, Funding Phases
One of the most underappreciated components of healthcare system migration is accurate financial modeling. Migration involves both capital expenditure (CapEx) and operational expenditure (OpEx), and the mix will vary depending on your modernization strategy.
a. CapEx Investments
-
One-time licensing fees for new platforms
-
Hardware and infrastructure upgrades (if not cloud-hosted)
-
Consultant or system integrator costs
-
Data migration tools and middleware licenses
b. OpEx Commitments
-
Ongoing SaaS subscriptions (e.g., cloud-based EHRs)
-
API usage fees (Redox, Health Samurai)
-
Cloud storage, compute, and backup costs
-
Ongoing support and compliance monitoring
c. Phased Funding Model
Break down funding into stages:
-
Assessment & Strategy Design
-
Prototype & Integration Testing
-
Data Migration & UAT (User Acceptance Testing)
-
Go-Live & Stabilization
-
Support & Optimization
Tip: Consider aligning funding timelines with annual budget cycles and potential incentive programs (e.g., CMS reimbursement for health IT modernization in the U.S.).
5. Change Management & User Adoption Planning
Migration projects often fail not due to poor technology but due to resistance among clinicians and administrative staff. A robust change management strategy is essential.
a. Pre-Migration Communication
-
Run awareness sessions explaining the why behind modernization
-
Highlight clinician benefits (fewer clicks, faster charting, mobile access)
b. Workflow Mapping
-
Document existing clinical workflows and map them to the new system
-
Identify pain points and customize where necessary (e.g., order sets, documentation templates)
c. Superuser Programs
-
Identify clinical champions early
-
Train them deeply so they can coach peers
-
Involve them in go-live and feedback loops
d. Feedback & Continuous Improvement
-
Use in-app feedback tools to capture issues in real-time
-
Schedule structured check-ins after 30, 60, and 90 days
-
Feed user insights into the next iteration (e.g., fixing UI issues, modifying templates)
6. Sample Migration Timeline (Mid-Sized Hospital System)
Phase | Duration | Milestones |
Assessment & Planning | 2 months | System inventory, stakeholder alignment, budgeting |
Data Mapping & Prototyping | 2–3 months | Schema design, interoperability setup |
Migration Testing | 2 months | Data cleansing, ETL, user validation |
Go-Live Preparation | 1 month | Training, sandbox use, downtime planning |
Go-Live & Support | 1–2 weeks | Cutover, live support, post-launch monitoring |
Post-Go-Live Optimization | 1–2 months | Feedback cycles, backlog triage, performance tuning |
Regulatory Compliance and Security Considerations
Healthcare IT modernization is not only a technical and operational challenge—it is a legal and security imperative. As systems transition from legacy environments to cloud-native and API-driven architectures, they must adhere to strict compliance standards and defend against sophisticated cyber threats. Mishandling protected health information (PHI) during migration can lead to severe regulatory penalties, litigation, and reputational damage.
The key question for healthcare organizations undergoing transformation is: “What are the compliance risks when modernizing EHR systems?”
1. Regulatory Frameworks: Compliance Mapping
Healthcare IT systems must align with a combination of country-specific and international regulations. Each framework governs how data is stored, accessed, shared, and protected—both during day-to-day operations and throughout the migration lifecycle.
a. HIPAA (Health Insurance Portability and Accountability Act – U.S.)
-
Applicability: All entities handling PHI in the U.S.
-
Key Requirements:
-
Data encryption (at rest and in transit)
-
Access controls and role-based permissions
-
Detailed audit logging and breach notification protocols
-
-
Modernization Implication: Systems must log every access, modification, or transmission of PHI—legacy platforms often lack this granularity, requiring API-level auditing in newer environments.
b. HITECH (Health Information Technology for Economic and Clinical Health Act)
-
Enhancement to HIPAA, particularly concerning breach accountability and electronic data exchange.
-
Impacts:
-
Heightened penalties for non-compliance
-
Emphasis on secure EHR adoption
-
-
Modernization Implication: Cloud-based EHR vendors must sign a Business Associate Agreement (BAA) with healthcare clients to meet HITECH standards.
c. GDPR (General Data Protection Regulation – EU)
-
Applicability: Any organization handling EU citizens’ personal health data.
-
Key Rights:
-
Data portability
-
Right to erasure
-
Explicit consent for processing
-
-
Modernization Implication: Systems must support exportable, structured data (e.g., FHIR resources). Legacy EHRs not supporting FHIR or RESTful APIs may violate GDPR data access clauses.
d. CCPA (California Consumer Privacy Act)
-
Applicability: Healthcare organizations handling California residents’ data (in addition to HIPAA)
-
Focus: Consumer rights and transparency
-
Modernization Implication: Adds complexity to data sharing and patient consent management—especially in mobile and web-based apps.
“What are the legal rules I must follow when upgrading a hospital EHR system?
You must comply with HIPAA, GDPR, and other relevant laws governing encryption, access control, and data sharing.
2. Secure Data Migration: Encryption, Access Controls, and Audit Logging
System modernization often involves large-scale data transfers from legacy databases into modern environments. Mishandling this data—even temporarily—creates vulnerabilities.
a. Encryption Protocols
-
At Rest: Use AES-256 for encrypting data stored on servers, especially patient charts, lab results, and medication records.
-
In Transit: Use TLS 1.3 to secure all data movement between source systems, middleware, and new platforms.
Cloud Best Practices:
-
Enforce encryption keys managed by the healthcare entity (e.g., AWS KMS, Azure Key Vault)
-
Audit key usage and expiration dates
b. Access Controls
-
Implement role-based access control (RBAC) to limit PHI access to authorized personnel only
-
Leverage multi-factor authentication (MFA) for all admin and clinical users
-
Automate provisioning/deprovisioning of users with systems like Azure AD or Okta
c. Audit Logging and Forensics
-
Record every access, modification, and transmission of sensitive data
-
Ensure logs are immutable, timestamped, and stored securely
-
Use centralized logging services (e.g., AWS CloudTrail, Azure Monitor, ELK stack)
3. Threat Modeling Legacy-to-Modern Transitions
The migration period is particularly vulnerable. Organizations must anticipate and mitigate cybersecurity threats through proactive risk modeling.
a. Attack Surface Expansion
Migration projects temporarily increase the number of systems, APIs, and users in play. These transitional states are often poorly monitored, making them targets for:
-
Credential theft
-
Misconfigured ports and open endpoints
-
Unencrypted temporary backups
Mitigation Tactics:
-
Conduct penetration testing pre- and post-migration
-
Use network segmentation and virtual private clouds (VPCs) during staging
-
Employ web application firewalls (WAFs) and DDoS protection
b. Insider Threats
Legacy platforms with static credentials and no logging offer ideal conditions for insider threats. Migrating to a modern platform should include:
-
User behavior analytics (UBA) to detect anomalies
-
Least privilege models to restrict access during the transition
c. Third-Party Vendor Risks
Many migrations involve external integrators, consultants, and cloud providers. Healthcare entities are liable for their vendors’ actions.
Mitigation Strategy:
-
Use vendor risk assessments and require BAA agreements
-
Confirm compliance certifications (e.g., HITRUST, ISO 27001, SOC 2 Type II)
Is migrating my hospital data to the cloud secure?
Yes—if encrypted, access-controlled, and logged properly. Follow HIPAA and use secure cloud configurations.
4. Compliance Integration in DevOps and Automation
Modern DevOps workflows must be compliance-aware by default.
a. Infrastructure as Code (IaC) + Security
Use tools like Terraform or AWS CloudFormation to codify:
-
Data residency (geofencing for GDPR)
-
Encrypted storage buckets
-
Identity policies and audit trails
b. CI/CD Compliance Gates
-
Integrate static code analysis tools to detect insecure patterns
-
Use security-as-code checks (e.g., Snyk, Checkov) during deployment
-
Automate documentation generation for audit readiness
c. Policy-as-Code
Leverage tools like OPA (Open Policy Agent) to enforce fine-grained rules across microservices—e.g., blocking unapproved data egress
5. Post-Migration Compliance Audits
Once modernization is complete, compliance doesn’t end—it transitions into continuous monitoring and policy enforcement.
Activities:
-
Perform external audits (e.g., SOC 2 or HITRUST recertification)
-
Run monthly or quarterly risk assessments
-
Monitor real-time access logs and generate compliance reports on demand
Case Studies: Real-World Examples of Legacy Modernization in Healthcare
Healthcare IT modernization is often perceived as high-risk due to its complexity, cost, and potential disruption to clinical workflows. However, real-world examples across different regions demonstrate that with the right strategy, healthcare providers can modernize legacy systems successfully—achieving improved performance, clinician satisfaction, and long-term cost savings.
Case Study 1: U.S. Hospital Chain – Legacy EHR Refactored into Microservices
Organization: A regional hospital group in the U.S. Midwest with six acute care facilities and 3,500 staff.
Legacy System:
A monolithic EHR built on Microsoft SQL Server and ASP.NET Web Forms, developed in-house between 2005–2010. The system handled everything from patient registration and clinical notes to billing, but lacked mobile access, integration capabilities, and performance scalability.
Modernization Strategy:
-
Approach: Refactoring into microservices
-
Frontend: Rewritten using React.js for responsive clinician dashboards
-
Backend: Core modules (e.g., appointment scheduling, medication orders) decoupled into Node.js microservices
-
Interoperability: Integrated Redox middleware to standardize HL7 and FHIR messaging with external labs and payers
-
Hosting: Migrated backend to AWS ECS with Docker containers for deployment flexibility
Results:
-
Performance: API latency reduced from 1.8 seconds to <500ms; system uptime improved from 96.5% to 99.95%
-
Cost: Reduced annual IT operations costs by 38% through containerization and decommissioning legacy hardware
-
Clinician Satisfaction: Physician engagement surveys showed a 28% improvement in usability and navigation; mobile usage increased by 42% for on-call doctors
-
Security: Added end-to-end TLS, granular access control, and immutable audit logging
Case Study 2: UK NHS Trust – VistA to FHIR-Based Open Source EHR Migration
Organization: A mid-sized NHS Trust serving 450,000+ patients annually in Northern England.
Legacy System:
Used a customized version of VistA, the U.S. Department of Veterans Affairs’ EHR. Originally adopted in 2006, the system used MUMPS and lacked support for modern integration protocols and APIs.
Modernization Strategy:
-
Approach: Full replacement with an open-source, modular EHR built on FHIR and SNOMED CT
-
Platform: Chose OpenMRS with custom-built FHIR modules for UK NHS alignment
-
Interoperability: Added REST APIs and integrated with NHS Spine services for lab results, prescriptions, and patient demographics
-
Migration Process: Over 6 million patient records migrated via ETL pipeline built using Apache NiFi and Python scripts
Results:
-
Data Portability: Enabled seamless exchange with NHS Digital services, pharmacy systems, and immunization registries
-
Cost: Saved approximately £2.1 million over 3 years in licensing and support compared to proprietary EHR vendors
-
Clinical Impact: Reduced documentation time by 23%, leading to higher face-to-face patient interaction
-
Governance: Achieved NHS Digital compliance and passed third-party penetration testing and FHIR conformance audit
Case Study 3: APAC Health Network – Containerized Lab System Replatforming
Organization: A large multi-specialty hospital group in Southeast Asia with 12 locations and over 10,000 outpatient visits per day.
Legacy System:
A proprietary, Windows-based Laboratory Information Management System (LIMS) developed in the late 1990s. It could not scale across facilities, lacked web-based access, and required VPNs for external lab access.
Modernization Strategy:
-
Approach: Replatforming + containerization
-
Architecture:
-
Legacy LIMS codebase containerized with Docker
-
Rehosted to Google Kubernetes Engine (GKE)
-
Backend API abstraction layer created using GraphQL to normalize legacy SOAP/XML responses
-
-
Security:
-
Introduced OAuth 2.0 for lab access
-
All API transactions encrypted using TLS 1.3
-
-
Integration:
-
Built HL7 interfaces using Mirth Connect
-
Connected to national disease reporting platform via FHIR API
-
Results:
-
Scalability: Cut provisioning time for new hospitals from 8 weeks to 3 days
-
Cost: Avoided $5M+ in replacement costs by extending life of existing codebase while improving interoperability
-
Operational Efficiency: Sample-to-result reporting cycle time reduced by 40%
-
Business Continuity: Zero downtime during cutover through blue/green deployment approach
Comparative Summary Table
Metric | U.S. Hospital Chain | UK NHS Trust | APAC Health Network |
Legacy System | Monolithic EHR | VistA (MUMPS-based) | Windows-based LIMS |
Strategy | Refactor to microservices | Full rebuild (open-source EHR) | Replatforming + containerization |
Cloud Platform | AWS (ECS, S3, IAM) | On-prem + NHS Spine APIs | Google Cloud (GKE) |
Integration Tools | Redox, FHIR APIs | Apache NiFi, OpenMRS FHIR modules | Mirth Connect, GraphQL adapters |
Performance Gains | API latency ↓ 72%; uptime ↑ to 99.95% | Documentation time ↓ 23% | Sample reporting cycle time ↓ 40% |
Cost Reduction | IT OPEX ↓ 38% | £2.1M saved over 3 years | $5M in capex avoided |
Clinician Satisfaction | ↑ 28% survey score | Higher system adoption, less training | No disruption, mobile-ready dashboards |
Key Takeaways from These Modernization Stories
-
Modernization ≠ Replacement
Each case study used a different strategy—refactoring, replatforming, or rebuild—based on specific operational, financial, and risk profiles. -
Phased Rollouts Prevent Disruption
None of the organizations used “big bang” go-lives. Instead, all employed phased deployment, sandboxes, and shadow production to reduce clinician stress. -
FHIR APIs and Containerization Are Common Enablers
All three projects relied on FHIR-based interoperability, secure cloud platforms, and container orchestration to manage services. -
Measurable Outcomes Are Critical
Each project was tied to quantifiable KPIs: cost reduction, latency improvement, error rate decline, or clinician usability scores.
Challenges, Pitfalls & How to Avoid Them
Despite growing urgency and investment in healthcare IT modernization, a significant number of projects stall, underperform, or fail outright. According to a 2024 HIMSS survey, over 38% of healthcare IT leaders cited their modernization efforts as only “partially successful,” while 19% classified them as failures due to performance issues, clinician pushback, or incomplete integrations.
The critical question facing healthcare CIOs and CTOs is: “Why do legacy modernization projects fail in healthcare?”
The answer lies in recurring, identifiable pitfalls that stem from technical, organizational, and vendor-related complexities. Below are the most common issues—along with evidence-based mitigation strategies.
1. Data Silos and Incomplete Migrations
The Problem:
Legacy systems often store decades’ worth of clinical, operational, and billing data in disparate databases, flat files, or proprietary formats. When organizations migrate to modern platforms, they frequently:
-
Omit low-use but critical historical data
-
Migrate incomplete datasets without reconciliation
-
Fail to unify records across departments or facilities
This creates functional gaps, inconsistent patient histories, and regulatory exposure (e.g., inability to furnish full records on request under HIPAA or GDPR).
Example:
A midwestern hospital migrated its EMR but left out 7 years of imaging data stored in an on-prem archive. Physicians had to rely on external systems to retrieve older radiology records, delaying diagnostics and undermining trust in the new platform.
Mitigation:
-
Conduct complete data inventory and dependency mapping pre-migration
-
Use reconciliation tools to validate migration completeness
-
Create an archive layer with searchable legacy access during transition
2. Staff Resistance and Training Burdens
The Problem:
Clinicians, nurses, and administrative users often perceive modernization as a productivity threat rather than an improvement—especially when it changes how they document care, view patient history, or navigate clinical workflows.
Key reasons for resistance include:
-
Poorly designed UIs or workflow mismatches
-
Inadequate training or change support
-
Fatigue from prior IT rollouts
This can lead to:
-
Increased error rates during the transition period
-
High-volume help desk tickets
-
Slow adoption or reversion to shadow systems
Mitigation:
-
Engage clinicians early in user story mapping and prototyping
-
Pilot the system with clinical “superusers” who can champion adoption
-
Allocate 10–15% of the project budget to training and post-launch support
-
Offer role-specific onboarding and simulate real workflows in sandboxes
Example:
A UK NHS Trust launched a new EHR without giving emergency department staff time to test documentation workflows. Within 48 hours, patient triage delays doubled and required on-site remediation teams.
3. Vendor Lock-In and Integration Gaps
The Problem:
Many healthcare modernization projects fall into the trap of closed vendor ecosystems—where core functions (EHR, scheduling, labs, billing) are bundled under a single provider with limited external APIs or support for standards like FHIR or HL7.
This results in:
-
Expensive customization fees for new integrations
-
Limited interoperability with national registries, wearable devices, or third-party apps
-
Disruption when the vendor sunsets older versions or raises licensing costs
Example:
An APAC hospital selected a proprietary cloud EHR that lacked out-of-the-box FHIR support. When the Ministry of Health mandated reporting via a national FHIR gateway, the hospital had to rebuild its entire integration layer from scratch.
Mitigation:
-
Select modular platforms that follow open standards (FHIR, SMART on FHIR, HL7 v2/v3)
-
Request source code escrow or open API documentation in all vendor contracts
-
Use middleware abstraction layers (e.g., Redox, Health Samurai) to buffer against vendor-specific implementations
4. Inadequate Risk Planning and Go-Live Support
The Problem:
Even well-designed modernization projects can fail due to poor execution during cutover. Downtime, missing data, login issues, or unavailable support at go-live can erode months of stakeholder trust within hours.
Common issues:
-
Lack of rollback plan
-
No pre-migration performance baselining
-
Incomplete go-live playbooks
Example:
A U.S. hospital group transitioned to a new scheduling platform during flu season. Performance lag and untested appointment APIs led to widespread overbooking and missed follow-ups.
Mitigation:
-
Run load tests and validate all APIs pre-launch
-
Create a “cutover playbook” including fallback procedures
-
Staff war rooms and live support channels during the first 2–3 weeks
5. Misaligned Success Metrics
The Problem:
Many modernization projects default to IT-focused KPIs: uptime, latency, number of APIs. While these are important, success must be measured through clinical and operational impact.
Lack of clarity in KPIs can:
-
Undermine stakeholder buy-in
-
Delay recognition of early wins
-
Obscure usability or performance regressions
Mitigation:
Define success metrics upfront, including:
-
Clinician satisfaction (via surveys or NPS)
-
Task time reduction (e.g., minutes to chart a patient note)
-
Error reduction in labs, billing, or medication ordering
-
Patient feedback on digital services
Track these metrics pre- and post-migration using observability tools, logs, and qualitative feedback loops.
The Future of Healthcare IT Modernization (2025–2030)
As healthcare continues its digital transformation, modernization will shift from reactive upgrades to proactive innovation. Between 2025 and 2030, legacy modernization won’t just mean replacing old systems—it will involve building AI-native, real-time, interoperable ecosystems designed for autonomy, scale, and intelligence. The future of healthcare legacy modernization is being shaped by four major forces: intelligent infrastructure, automation, real-time analytics, and universal data portability.
So, what’s the future of healthcare legacy modernization?
It’s a transition toward platformization, interoperability, and AI-augmented decision systems—not just modernization for maintenance, but for measurable clinical and economic outcomes.
1. AI-Native Infrastructure Replacing Procedural Systems
Legacy EHRs, billing systems, and lab platforms were designed as procedural databases: rule-driven, UI-heavy, and interaction-agnostic. Future platforms will be AI-native by design, meaning:
-
Built on event-driven architectures
-
Powered by real-time inference engines
-
Trained on longitudinal patient data for personalized recommendations
Examples of AI-Native Functions:
-
Clinical summarization agents that condense multi-year records into physician-ready narratives
-
Adaptive EHR interfaces that auto-adjust fields based on specialty, visit type, and historical patterns
-
Medical image analysis engines embedded directly into PACS viewers for faster diagnostics
This shift will require IT systems to incorporate:
-
Embedded LLMs for reasoning tasks
-
GPU-native databases for low-latency inference
-
Open telemetry for training feedback loops
2. Agent-Based Automation of Clinical Workflows
Modernization will move beyond APIs and dashboards toward agent-based automation—modular, task-specific digital workers that handle repetitive clinical and administrative tasks.
Use Cases:
-
Care coordination agents that triage cases, schedule referrals, and gather pre-visit data
-
Revenue cycle agents that validate insurance, auto-correct claim codes, and flag audit risks
-
Pre-charting agents that prepare SOAP notes based on recent labs, imaging, and visit history
These agents will be orchestrated by workflow engines such as LangGraph, AutoGen, or cloud-native services like AWS Step Functions.
Impact:
-
Reduces clinician data entry
-
Shortens time to reimbursement
-
Enables continuous, asynchronous care
3. Real-Time Data Lakes and Predictive Diagnostics
The future of modernization includes real-time data environments that connect EMRs, labs, wearables, and third-party data sources into unified analytics platforms.
Technologies Driving This Shift:
-
FHIR-based data lakes that ingest streaming health data from multiple systems
-
Feature stores for training predictive models (e.g., readmission risk, sepsis prediction)
-
Data mesh architectures that decentralize analytics while maintaining governance
By 2030, most health systems will rely on these capabilities to:
-
Trigger proactive interventions (e.g., adjusting care plans based on vitals)
-
Enable real-time dashboards for care teams and patients
-
Support adaptive clinical trial matching
Example:
A health network in Canada already uses FHIR and Snowflake to detect patterns across 2M+ patients in real time, leading to 21% faster interventions in cardiac emergencies.
4. Seamless Interoperability via FHIR, SMART on FHIR, and TEFCA Alignment
True modernization requires frictionless interoperability—the ability to send, receive, and act on health data across systems, organizations, and geographies.
Core Enablers:
-
HL7 FHIR as the canonical data format for clinical, billing, and admin data
-
SMART on FHIR apps for user-friendly patient and clinician experiences
-
TEFCA (Trusted Exchange Framework and Common Agreement) in the U.S. for national health information exchange compliance
By 2030, systems that cannot meet these interoperability requirements will be excluded from public networks, reimbursement programs, or clinical trials.
What This Looks Like in Practice:
-
Clinicians can access external imaging, labs, and medication lists within their own EHR UI
-
Patients can port their complete health record to any provider, globally
-
AI tools can train on de-identified multi-site data for precision medicine applications
Anticipated Impact:
-
Zero-friction data exchange
-
Reduction in duplicated tests and documentation
-
Improved outcomes from shared, longitudinal data views
From Modernization to Platformization
Legacy modernization is evolving from a one-time upgrade process into ongoing platform evolution. Future healthcare IT platforms will:
-
Be modular and composable by design
-
Support continuous deployment and feedback loops
-
Function as digital ecosystems, not isolated applications
These platforms will integrate not just EHR and scheduling, but also:
-
Population health tools
-
Remote monitoring systems
-
AI agents and microservices
-
Public health registries
Ultimately, modernization will not be about keeping up with regulation—it will be about leading care transformation with responsive, intelligent, and interoperable infrastructure.
Strategic Recommendations for CTOs & IT Leaders
Healthcare modernization is no longer a single-phase IT upgrade—it is an enterprise-wide transformation that affects clinical workflows, security posture, financial performance, and patient experience. For Chief Technology Officers, CIOs, and transformation leaders, the challenge lies in balancing innovation with continuity, all while delivering measurable returns on investment (ROI).
A question frequently raised in strategic planning sessions is: “How should healthcare CTOs approach legacy system replacement?”
The answer requires clarity on timing, scope, governance, and long-term operational fit.
1. Build an ROI-Driven Modernization Roadmap
A successful modernization plan must be tied to business and clinical outcomes, not just technical improvements. ROI should be measured across four dimensions:
a. Financial Efficiency
-
Reduce total cost of ownership (TCO) by migrating from legacy licensing and maintenance models to scalable cloud-native services.
-
Factor in cost avoidance from reduced security incidents, compliance fines, and hardware refreshes.
b. Clinical Productivity
-
Measure reductions in clinician time spent on data entry, duplicate documentation, and chart navigation.
-
Track improvements in throughput (e.g., patient encounters per physician per day).
c. Patient Engagement
-
Quantify improvements in portal usage, satisfaction scores (HCAHPS, NHS Friends & Family), and appointment adherence.
d. Operational Resilience
-
Measure downtime reduction, recovery time objective (RTO), and infrastructure scalability.
Recommendation:
Use a baseline-and-benchmark framework. Capture metrics from the legacy system before migration, define target KPIs, and track outcomes at 30/90/180-day intervals post-launch.
2. Decide When to Modernize vs. Replace
Not every legacy system needs to be rebuilt. CTOs must assess each system across four factors:
Assessment Area | Indicators to Modernize (Incremental) | Indicators to Replace (Full Rebuild) |
System Stability | Reliable, minimal critical issues | Frequent crashes, vendor end-of-life, security flaws |
Integration Flexibility | Can be wrapped with APIs or middleware | No API access, proprietary protocols, poor FHIR support |
User Satisfaction | Moderate complaints, usable with UI improvements | Severe workflow disruption, clinician rejection |
Regulatory Compliance | Minor gaps solvable via add-ons or encryption | Fails HIPAA/GDPR; lacks audit logging or access control |
Key Principle:
-
Modernize when the core logic still delivers value and integration is feasible.
-
Replace when foundational architecture limits growth, compliance, or user experience.
3. Structure Cross-Functional Modernization Teams
Technology decisions in healthcare are not solely the domain of IT. Successful modernization requires input from clinical, operational, legal, and financial stakeholders.
Recommended Team Structure:
-
Steering Committee
-
Roles: CIO, CMO, CFO, Compliance Officer
-
Responsibilities: Prioritization, funding, vendor approvals
-
-
Technical Core Team
-
Roles: CTO, Enterprise Architect, Security Lead, DevOps
-
Responsibilities: Architecture, integration, deployment planning
-
-
Clinical Advisory Group
-
Roles: Nurses, physicians, department heads
-
Responsibilities: Workflow mapping, usability testing, training feedback
-
-
Change & Adoption Team
-
Roles: PMO, HR, IT trainers, Superusers
-
Responsibilities: Training, support desk design, feedback channels
-
Key Success Factor:
Create bidirectional communication between clinical teams and developers—ideally via embedded clinical informaticists or “product owner” roles.
4. Plan for Long-Term Platform Evolution
Modernization should not be treated as a one-time event. Instead, CTOs should adopt platform thinking, where digital health systems evolve incrementally based on user feedback, regulatory change, and innovation cycles.
Key Strategies:
-
Embrace microservices and containerization to decouple components and reduce risk
-
Design for interoperability-first, not UI-first—ensuring FHIR APIs and standard data schemas
-
Invest in observability and usage analytics to continuously improve performance and adoption
Pro Tip:
Create a 3–5 year roadmap that includes:
-
Annual system upgrades
-
Feature deprecation planning
-
Technical debt management
-
Budget earmarks for emerging technology pilots (e.g., LLMs, RAG agents, synthetic data)
Legacy modernization is not simply about replacing outdated software—it’s about building the foundation for scalable, secure, and patient-centered care delivery. CTOs who succeed in this transformation focus not just on systems, but on stakeholders, outcomes, and sustainable evolution.
Conclusion & Final Checklist
Healthcare IT modernization is no longer just a technical requirement—it is a foundational capability for delivering secure, efficient, and patient-centered care in a connected ecosystem. This guide has outlined the strategic, technical, regulatory, and operational dimensions that healthcare leaders must navigate to modernize legacy systems in 2025 and beyond.
From obsolete EHRs and siloed LIMS to outdated billing systems and non-compliant data infrastructures, legacy technologies are increasingly incompatible with modern healthcare delivery. But modernization—when done right—is not only feasible, it’s transformative.
Summary of the Modernization Approach
This guide has provided a structured approach that healthcare IT leaders can apply to execute successful modernization initiatives:
-
Assess Systemic Risk: Start with a comprehensive inventory of outdated platforms, integration gaps, and compliance risks. Prioritize systems based on clinical impact and vulnerability.
-
Select the Right Modernization Strategy: Whether through rehosting, replatforming, refactoring, full replacement, or FHIR-based encapsulation, the strategy must align with operational readiness and long-term interoperability.
-
Deploy Modern, Interoperable Tech Stacks: Use frameworks like React and Angular for frontend interfaces, Node.js or .NET Core for backend services, and PostgreSQL or FHIR stores for data management. Enable communication through Mirth Connect, Redox, or Health Samurai.
-
Secure the Transition: Encrypt all data, enforce RBAC, enable full audit logging, and adopt cloud-native platforms with HIPAA/GDPR-ready infrastructure.
-
Align Around Outcomes: Define ROI across cost savings, clinician productivity, patient engagement, and infrastructure resilience.
-
Design for the Future: Build with FHIR, SMART on FHIR, and TEFCA in mind. Enable AI-native features, LLM-assisted workflows, and real-time analytics pipelines.
Back to You!
Modernization is no longer a future project—it is a present imperative. Systems built 15–20 years ago were not designed to support today’s clinical velocity, regulatory complexity, or patient expectations. Those that modernize now will define the next decade of healthcare delivery. Those that delay risk regulatory penalties, cyber breaches, and systemic inefficiency.
Whether you’re managing a community hospital, a national health service trust, or a multisite health network, modernization must be strategic, incremental, and outcome-oriented.
Modernization Partner: Aalpha Information Systems
Aalpha Information Systems is a trusted partner to healthcare software development company, offering deep expertise in legacy system modernization, FHIR integration, cloud-native architecture, and secure data migration. We support U.S., UK, EU, and APAC healthcare clients in rebuilding mission-critical systems with modern technologies—while ensuring clinical alignment, compliance readiness, and long-term scalability.
From planning phased migrations to building microservices-based EHRs, and integrating with TEFCA, NHS Spine, or national disease registries, Aalpha brings proven execution frameworks, domain-specific developers, and healthcare-grade DevOps to every engagement.
Get in touch to schedule a modernization readiness audit or to explore a proof of concept tailored to your institution’s legacy landscape.
Checklist to Get Started:
- Conduct a full inventory of legacy systems and dependencies
- Map out data sources, risks, and regulatory gaps
- Select your modernization path (rehost, refactor, replace, etc.)
- Define KPIs across clinical, financial, and operational dimensions
- Assemble cross-functional teams (clinical, IT, compliance, finance)
- Create a migration playbook with testing, training, and fallback plans
- Choose open-standard platforms and ensure FHIR compatibility
- Secure executive sponsorship and phased funding
- Measure post-launch performance and optimize iteratively
Modernization is not the finish line—it’s the launchpad. Build it deliberately, manage it collaboratively, and evolve it continuously.