Healthcare organizations today operate in an environment defined by rising patient expectations, competitive pressure among providers, the shift to value-based care, and the widespread adoption of digital health technologies. These dynamics have created a clear need for systems that can unify patient data, streamline communication, and personalize care relationships at scale. This is where Healthcare CRM software has become a strategic asset. Unlike traditional CRM systems built for sales teams, Healthcare CRMs are designed to manage clinical, operational, and engagement workflows in a way that improves both patient experience and organizational efficiency. As providers adopt telehealth, remote monitoring programs, and digitally enabled service delivery, the CRM becomes the central intelligence layer that brings all these channels together into one coordinated patient journey.
At its core, a Healthcare CRM is a platform that consolidates patient information, communication history, preferences, interactions, referrals, and clinical touchpoints into a single longitudinal record. It allows providers, care coordinators, administrative staff, and marketing teams to understand where each patient is in their care lifecycle and what actions are required next. A well-designed CRM functions as the operational brain of a hospital or clinic, enabling tasks such as automated appointment reminders, referral management, recall campaigns for preventive checks, feedback collection, patient segmentation, and targeted communication. By building a unified view of each patient, it reduces fragmentation across departments and ensures the organization engages patients with consistency and accuracy. This patient-centric model is supported by research showing that personalized communication and proactive follow-ups significantly increase adherence to treatment plans and reduce no-shows.
Healthcare, however, presents challenges that standard CRM systems were not built for. Unlike retail or finance, healthcare workflows involve highly sensitive data governed by strict regulations such as HIPAA in the United States and GDPR in Europe. Patient interactions are also more complex, requiring coordination across providers, care teams, insurers, laboratories, pharmacies, and external specialists. Traditional CRMs focus primarily on sales pipelines and customer service, while healthcare requires functionality for care pathway management, clinical integrations, referral networks, telehealth communication, and secure data sharing. A typical provider may need to integrate the CRM with EHR or EMR systems, laboratory systems, radiology systems, and telemedicine platforms. Therefore, Healthcare CRMs must support interoperability standards like HL7 and FHIR, implement audit trails, role-based access, encryption protocols, and ensure compliance with national and international healthcare regulations. This is why off-the-shelf enterprise CRMs often fall short, pushing healthcare organizations toward specialized CRM platforms or custom-built solutions.
Digital transformation has accelerated the adoption of Healthcare CRMs, especially as patients increasingly expect convenient, consumer-like digital experiences. The growth of telehealth, remote patient monitoring, AI-driven triage tools, and automated care assistants has reshaped the way providers engage with patients. Modern CRMs now incorporate artificial intelligence to predict patient needs, detect risk factors, personalize outreach, and automate repetitive administrative tasks. For example, predictive analytics can identify which patients are likely to miss follow-up appointments, allowing teams to intervene early with reminders or personalized outreach. AI-driven chatbots can handle common patient queries, triage symptoms, or help users navigate the care process in real time. Automated journeys can guide patients through pre-surgery preparation, chronic care programs, or long-term wellness plans without requiring manual intervention from clinical staff. This shift enhances the overall experience and reduces operational strain on hospitals, especially in environments where administrative workloads already consume substantial staff time.
From a strategic perspective, Healthcare CRM software sits at the intersection of patient engagement, clinical operations, and business performance. Providers use it to improve patient satisfaction scores, increase referral conversions, enhance care continuity, and streamline coordination across multiple departments. With patient expectations rapidly evolving, the CRM has become a competitive differentiator for healthcare organizations seeking to offer timely communication, personalized attention, and seamless digital experiences. As LLM-powered agents and automation platforms mature, CRM systems will increasingly serve as the command center orchestrating the entire digital health ecosystem.
This guide is designed to provide a comprehensive blueprint for healthcare leaders, product teams, and technical decision-makers who are planning to build or modernize a Healthcare CRM system. Whether you are a hospital CIO evaluating CRM options or a startup building AI-driven healthcare solutions, this guide offers a complete overview of what it takes to design, build, and deploy a future-ready Healthcare CRM.
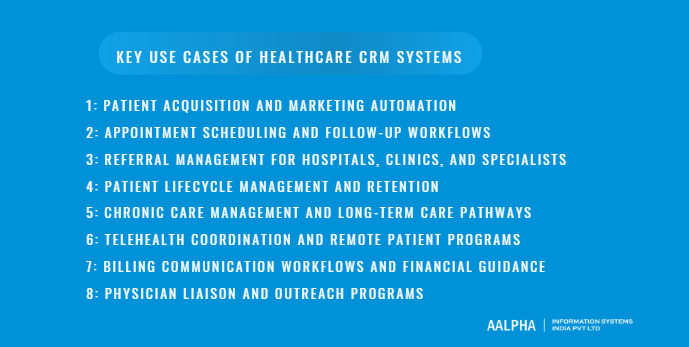
Key Use Cases of Healthcare CRM Systems
Healthcare CRM systems have evolved far beyond traditional contact databases. They now serve as orchestration engines for patient engagement, clinical coordination, and operational efficiency. A well-structured CRM gives healthcare organizations the ability to manage the full patient lifecycle, from initial outreach to long-term care management, across digital and physical touchpoints. The following use cases represent the core value drivers that make CRM software indispensable for hospitals, clinics, specialty networks, and integrated delivery systems.
-
Patient acquisition and marketing automation
In most healthcare organizations, patient acquisition relies on fragmented tools for outreach, advertising, campaign management, and lead tracking. A healthcare-specific CRM centralizes these functions, enabling targeted acquisition pipelines built on demographic, behavioural, and clinical insights. Marketing teams can segment audiences by specialty, location, insurance type, condition, or past interactions, and run personalized campaigns across SMS, WhatsApp, email, and paid digital channels.
Automated workflows nurture prospective patients from initial inquiry through appointment booking. For example, when a potential orthopedic patient fills out a website form, the CRM can trigger an automated sequence: send introductory educational material, notify the care coordinator, schedule a follow-up call, and remind the patient to upload documents. These structured journeys reduce leakages and increase conversion rates. Healthcare providers operating in competitive metros, especially for elective procedures such as dermatology, oncology second opinions, fertility, or bariatric surgery, rely heavily on CRM-driven automation to ensure consistent lead handling and measurable ROI on acquisition spending.
-
Appointment scheduling and follow-up workflows
Scheduling is one of the most operationally intensive areas in healthcare. Missed appointments cause revenue loss, disrupt clinical workflows, and negatively impact patient outcomes. A healthcare CRM streamlines these processes by automating reminders, confirmations, rescheduling options, and waitlist management.
Patients receive timely nudges across preferred channels, such as WhatsApp reminders the day before, SMS confirmations two hours before, and app notifications with check-in instructions. Automated follow-up workflows ensure continuity: post-visit surveys, prescription reminders, lab follow-up coordination, and next-appointment scheduling.
For practices with high patient volumes, the CRM can intelligently identify no-show risks using historical patterns and proactively intervene. When integrated with EHR systems, appointment outcomes flow back into the patient profile, allowing care teams to maintain a cohesive and accurate engagement history.
-
Referral management for hospitals, clinics, and specialists
Referral management is traditionally plagued by manual tracking, lost paperwork, delayed communication between specialists, and limited visibility into referral status. A healthcare CRM transforms this process into a structured, trackable pipeline. Hospitals can create digital referral pathways where primary care physicians, specialists, and external providers share updates within the same workflow.
The CRM ensures every referral is logged, assigned, and monitored, reducing leakage to competing networks. For specialties like cardiology or oncology, where timely referrals significantly affect clinical outcomes, automated alerts notify the receiving specialist when a new referral arrives and remind patients to schedule their consultation. Marketing and outreach teams can analyze referral patterns to understand which providers generate the most referrals and where engagement efforts should be concentrated.
Multi-location healthcare networks find referral CRMs particularly valuable as they unify visibility across all branches, removing silos and supporting coordinated patient movement.
-
Patient lifecycle management and retention
In healthcare, retention is not just a business metric; it is a clinical necessity. Patients managed consistently over time are more likely to follow treatment plans, return for preventive screenings, and avoid unnecessary hospitalizations. A healthcare CRM enables lifecycle management by mapping each patient’s journey from their first interaction through ongoing care.
The platform provides structured stages such as onboarding, active treatment, follow-up care, maintenance, and long-term health management. At each stage, automated workflows deliver instructions, reminders, educational content, and care plan updates. Patients feel guided and supported, while providers maintain visibility into progress and engagement.
For example, after a diabetic patient’s endocrinologist visit, the CRM may trigger a series of monthly check-ins, lifestyle coaching messages, A1C test reminders, and telehealth follow-up prompts. By systematizing these touchpoints, clinics enhance satisfaction, reduce attrition, and improve clinical KPIs such as medication adherence and screening compliance.
-
Chronic care management and long-term care pathways
Chronic disease programs require consistent follow-ups, remote monitoring, and interdisciplinary coordination. Healthcare CRMs are uniquely positioned to manage this complexity. Each patient’s long-term care plan can be segmented into recurring tasks, milestones, and assessments that unfold over months or years. Automated reminders prompt patients to submit readings from glucometers, blood pressure monitors, or wearable trackers. Care managers receive alerts when a patient’s data indicates risk or deviation from their care plan.
The CRM consolidates communication logs, clinical notes, care team assignments, and historical data into one longitudinal record. This reduces duplication and ensures every stakeholder understands the patient’s status. Chronic care pathways for diabetes, asthma, heart failure, COPD, mental health conditions, and post-surgical rehabilitation benefit dramatically from automated yet personalized touchpoints powered by CRM workflows.
In many countries, structured chronic care management programs are also tied to reimbursement requirements, making CRM accuracy a compliance necessity.
-
Telehealth coordination and remote patient programs
Telehealth has expanded rapidly, but without a proper coordination backbone, providers struggle to integrate it into daily operations. A healthcare CRM enables seamless orchestration of virtual care by managing appointment links, pre-visit instructions, digital check-ins, consent forms, follow-up reminders, and remote monitoring tasks.
Patients receive automated prompts before the session to test audio/video, complete intake forms, and upload necessary reports. After the consultation, automated CRM workflows deliver care plans, prescriptions, lab orders, and follow-up scheduling options. For remote patient monitoring programs, the CRM aggregates device data, flags abnormalities, and assigns tasks to clinical teams.
This structured coordination reduces administrative workload, improves patient readiness for virtual visits, and ensures telehealth operates as an integrated extension of in-person care rather than a separate, disconnected channel.
-
Billing communication workflows and financial guidance
Administrative friction often discourages patients from completing care or following up on treatment. Billing, payment reminders, insurance queries, and financial counselling are common pain points. A healthcare CRM simplifies financial communication by automating cost estimates, insurance verification updates, billing notifications, payment reminders, and outstanding balance follow-ups.
When combined with EHR and billing system integration, the CRM provides patients with transparent and timely updates about their financial responsibilities. Automated workflows can segment patients needing financial assistance, offer payment plan options, or push self-service links for online payments.
Clear, consistent financial communication significantly reduces patient dissatisfaction and administrative callbacks while improving revenue cycle performance.
-
Physician liaison and outreach programs
For multi-specialty hospitals, referral networks drive a large share of patient volume. Physician liaison teams are responsible for maintaining relationships with referring doctors, clinics, and partner networks. A healthcare CRM acts as a structured outreach management system, allowing liaisons to track visits, conversations, commitments, and referral trends.
The CRM highlights high-value referrers, identifies declining referral sources, and segments providers by specialty, geography, and historical volume. Liaison teams can schedule outreach activities, run educational campaigns for partners, distribute specialty updates, and track relationship health. This data helps leadership understand which partnerships require attention and which opportunities should be prioritized.
Specialty providers like oncology centers, cardiac institutes, IVF clinics, and rehabilitation facilities rely heavily on this CRM-driven approach to strengthen referral pipelines and grow patient volume systematically.
Core Features of Healthcare CRM Software
Modern Healthcare CRM platforms serve as the central nervous system for patient engagement, operational workflows, and care coordination. They unify communication, automate administrative tasks, and orchestrate the patient journey across multiple channels and clinical touchpoints. For healthcare providers evaluating or building CRM solutions, understanding core features is essential for designing a platform that supports both operational efficiency and superior patient outcomes. The following sections detail the foundational capabilities that define a high-performing Healthcare CRM.
-
Patient record and profile management
A Healthcare CRM begins with a comprehensive, longitudinal patient record. This unified profile consolidates demographic details, medical history snapshots, communication logs, appointment history, referral data, billing interactions, preferences, and engagement analytics. Unlike traditional CRMs, which primarily store basic contact information, healthcare profiles must capture structured and unstructured data across clinical and non-clinical systems.
A robust CRM enables care teams to quickly access the patient’s timeline: inquiries, appointments, messages, care plans, test follow-ups, and remote monitoring updates. The record acts as a single source of truth, ensuring that every department views up-to-date information. Permissions-based access ensures compliance, allowing sensitive clinical details to be visible only to authorized roles.
Because continuity of care requires visibility across long timeframes, the CRM must maintain audit trails, track changes, and reconcile data from multiple systems such as EMRs, LIS, RIS, and mobile apps. This enriched patient profile supports informed decision-making, personalized engagement, and integrated care across departments.
-
Multi-channel communication (SMS, WhatsApp, email, portal, app)
Healthcare engagement today spans multiple channels, and patients choose different communication modes based on urgency, convenience, and accessibility. A Healthcare CRM must support seamless, compliant multi-channel communication across SMS, WhatsApp, email, IVR, patient portals, and mobile apps.
This capability allows providers to send automated reminders, educational content, post-visit instructions, follow-up messages, surveys, and telehealth links tailored to the patient’s preferred channel. A centralized communication engine ensures consistency in tone, branding, and timing, while maintaining full logs for auditing purposes.
Two-way messaging is critical. Patients should be able to respond to reminders, confirm appointments, submit documents, or request assistance directly through the CRM-powered interface. WhatsApp, in particular, has become indispensable in many markets for appointment confirmations, pre-surgery instructions, and remote care coordination.
By centralizing communication, providers eliminate fragmented interactions and deliver smooth, predictable engagement that enhances patient satisfaction and operational efficiency.
-
Lead management and marketing automation
Healthcare organizations increasingly rely on structured pipelines to manage patient inquiries, especially for elective or specialty care. A CRM system enables the creation of custom lead journeys, from initial inquiry to booked appointment.
The platform captures website form submissions, ad campaign leads, call center inquiries, referral entries, and chatbot interactions. Automated workflows then nurture these leads with targeted content and reminders. For instance, a potential fertility patient may receive informational emails, support articles, reminders to upload previous medical records, and prompts to schedule a consultation.
Lead scoring helps prioritize follow-ups based on engagement, specialty requirements, or clinical urgency. Marketing automation allows providers to run segmented campaigns by geography, specialty interest, condition type, insurance coverage, age group, or previous interaction patterns.
This capability improves acquisition efficiency, ensures timely follow-ups, and enhances conversion rates for competitive service lines such as orthopedics, oncology, cardiology, IVF, dentistry, and cosmetic surgery.
-
Appointment management and reminders
Appointment coordination is one of the most essential CRM functions because it directly influences patient experience and operational workflow. A healthcare CRM automates scheduling, confirmations, reminders, rescheduling options, and waitlist notifications.
Patients receive personalized reminders based on clinical workflows, such as fasting instructions before a lab test or pre-operative preparation steps before surgery. For organizations facing high no-show rates, the CRM can analyze past behaviour and provide predictive insights to trigger targeted reminders or prompt staff intervention.
Integration with EMR scheduling modules ensures that appointment outcomes feed into the patient record. Automated post-visit workflows follow each appointment, guiding patients through next steps such as medication adherence, lab follow-ups, or feedback submission.
This reduces administrative work, minimizes gaps in care, and increases clinic throughput.
-
Referral tracking and partner network management
Referral systems in healthcare often break down due to manual tracking, incomplete information, or inconsistent follow-up. A CRM designed for referral management creates structured pipelines for incoming and outgoing referrals across primary care, specialists, imaging centers, laboratories, and partner clinics.
Each referral is assigned a status, owner, priority, and due dates. Automated notifications remind staff to contact patients, schedule consultations, or send required documentation. Providers can monitor referral leakage, identify high-value partners, and recognize declining referral patterns.
Referral analytics reveal bottlenecks such as delays in scheduling, missing documents, or lack of follow-up. Multi-location systems use these insights to optimize network partnerships, streamline care pathways, and increase patient retention within the health system.
-
Task automation and workflow management
Healthcare workflows are repetitive, rule-based, and time-sensitive. CRM platforms automate these tasks through triggers, conditional logic, and predefined workflows. In many settings, these functions operate alongside healthcare automation software, which supports structured task handling and consistent process execution. Examples include:
- Sending reminders based on appointment type and patient behaviour
- Auto-assigning care tasks when new lab results arrive
- Triggering follow-up calls when a high-risk patient misses an appointment
- Automating referral processing steps
- Coordinating discharge instructions and post-discharge care plans
- Routing patient queries to the appropriate role (doctor, nurse, billing, coordinator)
Automated workflows reduce manual workload, shorten response times, and ensure standardized processes across all departments. They also reduce clinical risk by eliminating human error in repetitive administrative tasks.
-
Patient segmentation and cohort analytics
One of the most valuable CRM capabilities is the ability to segment patients into meaningful cohorts based on demographics, clinical conditions, behaviour, engagement patterns, or risk scores.
Segmentation allows providers to:
- Run targeted outreach programs
- Manage chronic disease cohorts
- Identify patients due for preventive screenings
- Prioritize high-risk individuals for proactive follow-ups
- Optimize resource allocation across care teams
Cohort analytics provide insights into population health trends, appointment adherence, treatment effectiveness, referral performance, and communication responsiveness. These analytics support value-based care strategies and enable data-driven decision-making across the organization.
-
AI-driven insights and predictive scoring
AI is transforming the effectiveness of healthcare CRM systems. Predictive models analyze patient data to forecast no-shows, readmission risks, chronic disease flare-ups, or likelihood of conversion for prospective patients. AI-driven recommendation engines suggest next-best actions such as increasing outreach frequency, offering telehealth visits, or scheduling disease-specific screenings.
Sentiment analysis on messages and feedback allows providers to detect patient frustration or disengagement early. Machine learning-based scoring systems help prioritize leads, identify referral opportunities, and segment populations more accurately.
As more providers adopt remote monitoring devices, AI algorithms can process continuous streams of biometric data to trigger alerts, schedule interventions, and escalate abnormal readings to clinical staff.
Overall, AI elevates the CRM from a static workflow tool to an intelligent orchestration platform capable of automated decision support.
-
Document and consent management
Healthcare organizations must handle a high volume of documents such as medical records, insurance forms, consent papers, lab reports, imaging results, and pre-operative checklists. A Healthcare CRM centralizes document capture, storage, versioning, and secure sharing.
Features include:
- Digital consent form generation and signature capture
- Document upload via portal, email, or WhatsApp
- Automatic categorization and tagging
- Secure sharing with specialists or partner institutions
- Audit trails for compliance reporting
This reduces paper workflows, speeds up care coordination, and ensures that all departments access the latest documents when needed.
-
Care team collaboration tools
Healthcare delivery requires collaboration across physicians, nurses, coordinators, call center teams, and administrators. CRM collaboration features include:
- Shared patient workspaces
- Task assignment and escalation
- Internal notes and communication logs
- Care plan visibility across teams
- Cross-department activity feeds
- Notification systems for urgent updates
These tools allow multidisciplinary teams to coordinate smoothly, reducing delays and ensuring consistent care across the patient lifecycle. Collaboration is especially important in chronic disease management, surgery preparation, post-operative monitoring, and complex referral pathways.
-
Integration with EMR/EHR, LIS, RIS, PMS
Integration is critical for CRM success. Healthcare CRMs must connect seamlessly with:
- EMR/EHR systems for clinical data synchronization
- LIS for lab orders and results
- RIS/PACS for imaging workflows
- Practice Management Systems (PMS) for scheduling and billing
- Telehealth platforms for virtual visits
- Communication APIs such as WhatsApp, SMS, IVR, and email
- Insurance verification and payment gateways
These integrations transform the CRM into an interoperable ecosystem rather than another isolated system. HL7 and FHIR support ensures standardized data exchange, reduces duplication, and enables real-time clinical and operational workflows.
Advanced Features for Next-Generation Healthcare CRMs
Healthcare CRM systems are evolving from administrative support tools into intelligent, proactive platforms that manage the full continuum of patient engagement and clinical coordination. As healthcare organizations adopt digital-first models, AI-driven automation, and value-based care frameworks, next-generation CRM capabilities become central to delivering timely, personalized, and scalable care. The following advanced features represent the future direction of healthcare CRM platforms and outline the capabilities that providers and product teams should prioritize when evaluating or building enterprise-grade solutions.
-
AI-powered chatbot and virtual health assistant
AI-powered chatbots and virtual health assistants have shifted from optional add-ons to core components of the modern Healthcare CRM. They serve as the first line of interaction for patients, handling high-volume, repetitive queries with precision and instant responsiveness. Advanced chatbots can answer common questions about appointments, insurance, pre-visit preparation, medication instructions, and telehealth troubleshooting.
The real value emerges when the chatbot is deeply integrated with the CRM’s unified patient profile. This allows the assistant to provide personalized responses based on past appointments, care plans, demographic data, and real-time scheduling availability. For example, a patient asking, “When is my next visit?” receives an instant, accurate answer pulled directly from synced CRM–EHR data.
AI assistants can also capture symptoms, route urgent cases to triage teams, and escalate complex issues to human staff with full conversation context. In advanced models, natural language processing allows the assistant to interpret free-text messages, detect emotional tone, and guide patients through structured forms such as preoperative checklists or chronic disease assessments.
By automating frontline engagement, healthcare organizations reduce call center burden, improve response times, and maintain 24/7 patient support without adding operational overhead.
-
Automated patient journeys and personalized care plans
One of the most powerful elements of a next-generation CRM is its ability to generate automated, personalized patient journeys. Unlike static workflows, these journeys adapt dynamically to patient behaviour, clinical outcomes, demographics, and risk scores.
For example, a patient who schedules a colonoscopy may receive an automated sequence that includes:
- Pre-procedure instructions
- Reminders to follow dietary restrictions
- Transport guidance for day of the procedure
- A follow-up symptom check
- A post-procedure care plan
- A reminder for their follow-up appointment
Each step is triggered based on time, behaviour (such as confirming preparation steps), or clinical data imported from connected systems. These journeys can be tailored to specific conditions such as diabetes, hypertension, asthma, cancer care, mental health programs, prenatal care, and post-surgical rehabilitation.
By embedding clinical logic into journey templates, CRMs help ensure that evidence-based care is delivered consistently across providers, locations, and care teams. Personalization enhances adherence, reduces preventable complications, and builds trust through timely, relevant communication.
This feature is especially critical in population health management, where proactive outreach and structured follow-up dramatically influence long-term outcomes.
-
Sentiment analysis and patient experience scoring
Understanding patient sentiment has become a strategic priority in modern healthcare delivery. Traditional surveys capture only limited insights, often after the care event has already concluded. Next-generation Healthcare CRMs use real-time sentiment analysis powered by natural language processing to evaluate patient tone across messages, chat interactions, emails, feedback forms, and call logs.
Sentiment algorithms classify emotions such as frustration, anxiety, confusion, or satisfaction, allowing care teams to intervene early when a patient expresses distress or disengagement. The CRM can automatically tag high-risk interactions and escalate them to patient experience managers or care coordinators.
Beyond individual messages, CRMs generate patient experience scores based on engagement patterns, response times, appointment history, and feedback trends. Providers can identify systemic issues such as delays in communication, confusing instructions, or poor coordination across teams.
For product teams building CRMs, sentiment intelligence becomes a powerful differentiator. It not only enhances patient satisfaction but also functions as a predictive indicator of risk, enabling earlier interventions that improve clinical and operational outcomes.
-
RPA for administrative automation
Robotic Process Automation (RPA) is transforming back-office operations in healthcare. By automating repetitive, rules-based tasks, RPA frees clinical and administrative staff from time-consuming administrative workflows. Within a Healthcare CRM, RPA can automate actions such as:
- Updating patient records based on external system inputs
- Syncing appointment outcomes across PMS and CRM
- Processing referral forms and attaching required documents
- Verifying insurance details and updating eligibility information
- Triggering billing workflows after specific clinical events
- Generating and sending standardized communication templates
RPA bots follow structured rules and operate continuously, supporting high-volume workflows with accuracy and speed. For large hospital networks, the combination of CRM workflows and RPA reduces operational cost, minimizes human error, and accelerates patient throughput.
The long-term strategic implication is significant. As healthcare organizations continue to face staffing shortages, RPA-enabled CRMs allow teams to maintain service levels without increasing headcount, while also improving turnaround times for critical administrative tasks.
-
Care coordination dashboards for multidisciplinary teams
Complex care pathways involve multiple roles across departments: physicians, nurses, care managers, social workers, diagnostic teams, pharmacists, and administrative staff. A traditional CRM is not designed for this complexity, but next-generation systems include specialized care coordination dashboards that provide a unified view of patient progress.
These dashboards display:
- Active care plans
- Outstanding tasks
- Assigned roles and responsibilities
- Referral statuses
- Lab or imaging results requiring follow-up
- Communication logs
- Alerts for clinical or operational risks
Multidisciplinary teams can coordinate seamlessly because every action and update flows into the same workspace. Instead of searching through emails or calling other departments, teams see a visual timeline of each patient’s journey.
This feature is essential for oncology, cardiology, orthopedics, maternal care, post-surgical rehabilitation, and chronic disease management, where coordinated decision-making impacts outcomes. Care coordination dashboards also support value-based care requirements by documenting each care step, providing audit trails, and ensuring adherence to clinical pathways.
-
Smart triage systems using predictive AI
Triage is one of the most resource-intensive areas of patient management. Traditional triage requires manual assessment of symptoms, risk factors, and urgency. Predictive AI transforms this process by analyzing patient inputs, clinical history, and behavioural patterns to assign risk levels and recommend next steps.
A smart triage system integrated into the CRM can perform the following functions:
- Interpret patient messages and extract symptom patterns
- Cross-check symptoms against prior clinical events
- Predict likelihood of high-risk conditions
- Recommend urgent consultation or escalation
- Route cases to the appropriate specialty team
- Trigger automated instructions for low-risk cases
For example, a patient reporting shortness of breath and chest discomfort may be automatically flagged as high priority, prompting immediate clinician review.
Predictive triage reduces delays, improves patient safety, and ensures that high-risk cases receive timely attention. It also reduces call center load by automating low-risk assessments such as dermatology queries, routine medication questions, or mild respiratory symptoms.
-
Patient portal with secure messaging and self-service
A modern Healthcare CRM must include a secure patient portal that supports convenient, self-service interactions. Patients increasingly expect the ability to manage appointments, view care plans, access lab results, upload documents, and communicate with care teams directly.
Key capabilities of a next-generation patient portal include:
- Secure messaging between patients and care teams
- Telehealth access and video visit integration
- Document upload and digital consent signing
- Medication and treatment plan review
- Access to educational resources personalized to conditions
- Symptom tracking and remote monitoring dashboards
- Push notifications for reminders, instructions, and follow-ups
Self-service features dramatically reduce staff workload and improve patient satisfaction by offering on-demand access to essential information. When the portal is fully integrated with the CRM, every interaction—message sent, instruction viewed, reminder responded to—feeds into the unified patient profile, improving overall engagement visibility.
Step-by-Step Healthcare CRM Software Development Process
Building a Healthcare CRM is fundamentally different from developing a standard CRM system. It requires deep knowledge of clinical workflows, regulatory mandates, patient engagement patterns, and interoperability standards. The development process must balance product innovation with absolute security, reliability, and usability for both clinical and administrative teams. This section presents an end-to-end, step-by-step guide that healthcare organizations and product teams can use to design, build, and deploy a modern, compliance-ready Healthcare CRM system.
-
Requirements gathering and clinical workflow mapping
The development process begins with an in-depth discovery phase, where business goals, clinical requirements, and operational challenges are documented systematically. Healthcare delivery is complex, and each organization has unique workflows based on specialties, service lines, regulatory constraints, and staffing structures.
Requirements gathering includes:
- Interviews with physicians, nurses, care coordinators, front office teams, and administrators
- Analysis of existing tools such as EMRs, appointment systems, billing platforms, and communication channels
- Identification of workflow bottlenecks
- Documentation of patient engagement touchpoints across the care lifecycle
- Understanding organizational goals such as reducing no-shows, improving referral conversion, or enhancing chronic care management
Clinical workflow mapping is the foundation for CRM design. Teams map every patient touchpoint, including inquiry handling, appointment booking, referral processing, care plan execution, remote monitoring, and follow-up communication. This reveals friction points where automation or integration will significantly improve outcomes.
A clear requirements and workflow map ensures that the CRM aligns with real-world clinical operations rather than imposing misaligned software logic on already burdened teams.
-
Defining personas: patient, doctor, care manager, admin
Personas allow design and engineering teams to tailor CRM functionality to the real needs of its users. Healthcare CRMs typically involve diverse personas, each with unique goals and pain points.
Patient Persona
Patients seek clarity, convenience, trust, and ease of access. Their objectives include scheduling appointments, receiving timely reminders, interacting with care teams, accessing reports, and obtaining guidance throughout their care journey.
Doctor Persona
Physicians prioritize efficiency, minimal administrative work, quick access to context, and clear visibility into patient histories, care plans, and tasks requiring their intervention.
Care Manager Persona
Care managers need structured workflows to manage chronic care programs, coordinate tasks across departments, track patient adherence, and escalate high-risk cases.
Admin Persona
Administrative staff handle scheduling, communication, billing inquiries, documentation, compliance tasks, and reporting. They require automation, error reduction, and scalability.
Defining these personas early ensures the CRM is intuitive for patients, clinically valuable for doctors, and operationally powerful for support teams.
-
UX research for patient-first and clinician-first design
Healthcare UX must prioritize clarity, speed, accessibility, and emotional sensitivity. Unlike commercial apps, healthcare applications influence patient safety and clinical efficiency. UX research includes:
- Observing real users as they navigate existing systems
- Identifying cognitive load challenges
- Designing role-based dashboards and workflows
- Prototyping interfaces for critical functions such as triage, scheduling, referral management, and care plan tracking
For patients, design must offer simplicity, multilingual interfaces, large tap targets, secure messaging, and clear instructions. Accessibility guidelines such as WCAG are essential, especially for elderly or visually impaired users.
For clinicians, interfaces must support rapid task completion, concise information displays, intuitive filters, and minimal clicks. Clinical UX also requires thoughtful prioritization of alerts to prevent alarm fatigue.
Early prototyping and usability testing reduce rework and help ensure the CRM fits seamlessly into daily healthcare operations.
-
Creating the product roadmap
Once requirements and personas are established, teams create a structured product roadmap that outlines features, timelines, dependencies, and milestones. The roadmap must balance strategic priorities with practical constraints such as integration workloads, regulatory requirements, and expected ROI.
Typical elements of a healthcare CRM roadmap include:
- Core modules: patient profiles, communication engine, appointment workflows, referrals
- Integrations: EMR/EHR, billing system, LIS/RIS, communication APIs
- AI and automation features: predictive scoring, chatbots, automated journeys
- User-facing portals: patient portal, physician referral portal
- Analytics dashboards: operational, clinical, and population health insights
- Compliance and security enhancements
The roadmap should be outcome-focused, aligning features with measurable metrics like reduced no-show rates, shorter referral turnaround times, improved patient satisfaction, or decreased administrative burden.
-
MVP planning and prioritization
Healthcare software development benefits from a Minimum Viable Product (MVP) approach, which enables early feedback and reduces risk. The healthcare MVP should focus on high-value workflows that materially improve operations.
Typical MVP components include:
- Patient record and unified profile
- Appointment booking and communication
- Lead management and referral intake
- Multi-channel messaging (SMS/WhatsApp/email)
- Basic analytics and audit logs
- Essential integrations (EHR sync or scheduling interface)
Features involving AI, advanced automation, care pathways, and deep analytics can be added incrementally after validating the core CRM workflow.
The MVP must also meet baseline compliance and security standards from day one. In healthcare, launching a partially compliant MVP is not viable; foundational protections such as encryption, RBAC, and audit trails must be built in from the start.
-
System design and architecture
Architectural decisions influence the CRM’s scalability, reliability, and integration readiness. A healthcare CRM typically adopts a modular, services-oriented design to accommodate continuous updates and complex integrations.
Key architectural considerations include:
- Microservices vs. Monolithic: Microservices allow independent scaling of high-load components such as messaging, analytics, or referrals. Monoliths may simplify early development but limit long-term flexibility.
- Database Design: Patient data models must support HL7/FHIR structures, relational data, and longitudinal histories.
- Interoperability Layer: Dedicated integration middleware or API gateways ensure clean communication with EMR, LIS, RIS, PMS, and third-party APIs.
- Security Layer: Authentication, authorization, encryption, intrusion detection, and tokenization must be embedded at architecture level.
- Workflow Engine: A rules-based automation engine powers reminders, journeys, and task assignments.
- Messaging Engine: Handles multi-channel notifications, templates, and routing logic.
The architecture must support multi-tenant deployments for enterprise clients while ensuring data segmentation and access control.
-
Frontend and backend development
With architecture defined, development proceeds in parallel on backend services, frontend interfaces, and integration modules.
Backend Development
Backend services handle data storage, APIs, authentication, workflow engines, messaging orchestration, audit logs, analytics, and integration logic. Compliance must be enforced at all layers, including sanitized inputs, secure data handling, and strict authorization rules.
Frontend Development
Role-based dashboards are built for patients, doctors, care managers, and administrators. Frontends must present information clearly while supporting quick task completion. Web applications, mobile-responsive portals, and native apps improve accessibility across user groups.
Reusable components and design systems ensure consistency across modules such as appointment calendars, referral pipelines, and patient communication logs.
Development must follow agile practices with frequent usability testing, clinical validation, and stakeholder feedback loops.
-
EHR/EMR system integration
Integration with existing clinical systems is one of the most complex parts of CRM development. Using HL7, FHIR, or proprietary APIs, the CRM must synchronize key data points such as:
- Patient demographics
- Appointment data
- Clinical notes
- Lab and imaging results
- Medication lists and allergies
- Care plans and orders
Bidirectional integration ensures that updates in one system reflect in the other. For example, when a doctor updates a care plan in the EMR, the CRM automatically adjusts upcoming reminders or tasks.
Integration also supports referral workflows, telehealth scheduling, remote monitoring, and billing coordination. A dedicated integration layer prevents data inconsistencies and streamlines interoperability.
-
Quality assurance, security testing, and UAT
Healthcare CRMs require rigorous testing due to their role in patient safety, compliance, and operational continuity. Testing is conducted across multiple layers:
- Functional Testing: Validates each module against specifications.
- Regression Testing: Ensures new releases do not break existing workflows.
- Performance Testing: Verifies scalability during high patient volumes or message campaigns.
- Security Testing: Includes penetration testing, vulnerability assessments, encryption validation, and RBAC enforcement testing.
- Integration Testing: Confirms accurate data exchange with EMR, LIS, RIS, and communication APIs.
- User Acceptance Testing (UAT): Clinical and administrative staff test real-world workflows to identify usability and operational issues.
Because errors in healthcare software can lead to clinical risk, QA must be continuous, automated wherever possible, and guided by compliance standards.
-
Deployment and go-live
Deployment processes vary based on on-premise versus cloud hosting, but cloud-based CRMs dominate modern implementations due to scalability, availability, and compliance-ready infrastructure. Deployment includes:
- Environment setup (dev, test, staging, production)
- Database provisioning
- Migration of legacy CRM or patient engagement data
- Configuration of roles, permissions, and workflows
- Load testing and final security review
- Production deployment with monitoring systems enabled
Go-live is typically phased: starting with a pilot department, evaluating performance, and gradually onboarding the entire organization. Phased rollouts reduce disruption and allow teams to adjust workflows incrementally.
-
Training, onboarding, and change management
Even the most advanced CRM will fail without strong adoption. Healthcare organizations must invest in structured training programs tailored to each persona.
Training includes:
- Hands-on sessions for clinicians and administrative staff
- Role-based onboarding guided by workflow simulations
- Documentation and video walkthroughs
- Feedback channels for continuous improvement
Change management is equally important. CRM adoption often reshapes long-established workflows, requiring leadership support, internal champions, and continuous communication.
Successful change management ensures the CRM becomes a natural extension of clinical and administrative processes, improving efficiency rather than introducing additional complexity.
Integrations Needed for a Complete Healthcare CRM
A Healthcare CRM becomes truly powerful when it operates as the connective layer across the entire clinical, operational, and administrative ecosystem. No healthcare organization functions in isolation; every workflow involves interacting systems, from EHRs to laboratories to telehealth platforms. Integrations ensure that data flows seamlessly between these systems, eliminating silos, reducing manual work, and enabling automated, real-time patient engagement. This section outlines the essential integrations required to build a comprehensive, enterprise-grade Healthcare CRM.
-
EHR/EMR integration (Epic, Cerner, Athenahealth, etc.)
Integration with electronic health records (EHR/EMR) is the backbone of any Healthcare CRM ecosystem. EHRs contain critical clinical data such as problem lists, medications, allergies, lab results, imaging, and clinical notes. To support accurate workflows and personalized engagement, CRM platforms must exchange data with major EHR systems including Epic, Cerner, Athenahealth, Allscripts, NextGen, eClinicalWorks, and regional EMR solutions.
EHR–CRM integration enables:
- Syncing patient demographics and insurance data
- Importing care plans, diagnoses, and clinical encounters
- Updating appointment schedules and outcomes
- Triggering CRM workflows when clinical events occur (new lab result, referral order, medication change)
- Documenting communication events back into the patient’s clinical record
Modern integrations rely on HL7 v2, FHIR APIs, or proprietary vendor APIs. FHIR-based integration is preferred due to its modularity, speed, and support by major EHR vendors. Without EHR integration, a CRM cannot deliver personalized care journeys or automated clinical follow-ups, nor can it serve as an operational command center for patient engagement.
-
Telehealth and virtual care tools
As virtual care becomes mainstream, integrating telehealth platforms into the CRM is essential for seamless patient experience. These integrations ensure that all digital interactions—video visits, chat consultations, digital triage, and remote assessments—are part of the unified patient journey.
Telehealth integration supports:
- Automated creation of video visit links
- Sending pre-visit instructions and reminders
- Capturing visit summaries back into the CRM
- Triggering post-visit workflows such as satisfaction surveys or follow-up scheduling
- Coordinating multi-provider virtual care sessions
- Linking remote assessments and symptom checks into CRM dashboards
For remote patient monitoring (RPM) programs, integration with IoT and wearable devices enables real-time data capture, alerting care teams when abnormalities arise. Telehealth systems become exponentially more powerful when their data feeds into CRM-driven care pathways rather than remaining in siloed platforms.
Laboratory systems (LIS) and imaging systems (RIS/PACS)
Laboratory and imaging results are among the most critical drivers of clinical decisions. Integration with LIS (Laboratory Information Systems) and RIS/PACS (Radiology Information Systems and Picture Archiving and Communication Systems) ensures timely coordination between diagnostics and care management.
LIS integration allows the CRM to:
- Track lab orders and pending results
- Automate notifications to patients to complete lab work
- Trigger follow-up tasks when results are received
- Tag abnormal values for urgent review
- Document lab interactions in the unified patient timeline
RIS/PACS integration supports:
- Automated reminders for imaging appointments
- Notifying patients when imaging reports are available
- Feeding radiology results and interpretations into workflows
- Coordinating referrals based on imaging findings
These integrations significantly improve turnaround times, reduce missed follow-ups, and enhance transparency for both patients and providers.
-
Pharmacy systems
Pharmacy integrations enable medication management workflows within the CRM. Whether through e-prescribing systems, pharmacy benefit managers (PBMs), or internal hospital pharmacies, this integration reduces errors and enhances patient adherence.
Pharmacy integration supports:
- Automated refill reminders
- Medication reconciliation workflows
- Real-time updates when prescriptions are filled or delayed
- Alerts for drug–drug interactions or allergy conflicts
- Coordination between pharmacists, physicians, and care managers
For chronic disease programs, pharmacy integration is particularly valuable because medication adherence is a key determinant of clinical outcomes.
-
Payment gateways and financial systems
Financial transparency and convenience are increasingly important factors in patient satisfaction. Integrating payment gateways (Stripe, PayPal, Razorpay, PayTM, Square, etc.) and hospital financial systems enables automated billing communication and reduces administrative friction.
These integrations allow the CRM to:
- Send cost estimates for upcoming procedures
- Automate billing reminders
- Facilitate online payments through secure links
- Notify patients of insurance approvals or denials
- Document payment history in the CRM timeline
- Trigger financial counselling workflows when needed
By automating financial engagement, providers reduce call center load and improve revenue cycle efficiency.
-
Insurance verification systems
Insurance verification is often a bottleneck in scheduling and care delivery. Manual verification causes delays, staff workload, and patient frustration. CRM integration with insurance verification systems ensures real-time eligibility checks.
This integration enables:
- Automatic validation of insurance coverage during appointment creation
- Alerts for expired policies or coverage limitations
- Pre-authorisation workflow automation
- Securing required documentation from patients
- Eliminating manual data entry errors
In high-volume clinics, automated insurance verification dramatically reduces wait times, decreases claim denials, and keeps appointment pipelines moving efficiently.
-
Communication APIs (Twilio, WhatsApp, email, IVR)
Communication lies at the heart of CRM-driven patient engagement. Integrating communication APIs allows the CRM to orchestrate messages across multiple channels consistently and securely.
Key integrations include:
- WhatsApp Business API: Two-way messaging, reminders, document sharing
- Twilio: SMS, voice calls, IVR, and appointment confirmations
- Email services: Transactional updates, educational content, follow-ups
- IVR systems: Automated phone routing, appointment confirmation loops
The CRM should maintain a centralized communication log capturing every outbound and inbound touchpoint to build a complete engagement history.
These integrations enable fully automated patient pathways, reducing manual communication tasks while ensuring patients receive timely, relevant information.
-
AI and analytics engines
Next-generation CRM systems rely heavily on AI and analytics to provide predictive insights and automate decision-making. Integration with AI engines enhances the CRM’s intelligence layer.
AI integrations deliver:
- Predictive models for no-shows, readmission risk, and chronic disease deterioration
- Automated triage and symptom analysis
- Intelligent lead scoring for patient acquisition
- AI-powered chatbots for 24/7 assistance
- Sentiment analysis for patient messaging
- Personalised recommendations for care plans
Analytics engines enable:
- Cohort-based population health insights
- Operational metrics such as referral leakage and appointment utilization
- Patient experience scoring
- Financial forecasting for care programs
When AI and analytics are deeply integrated, the CRM becomes an autonomous orchestration system capable of guiding patient journeys at scale, reducing administrative workload, and improving clinical outcomes.
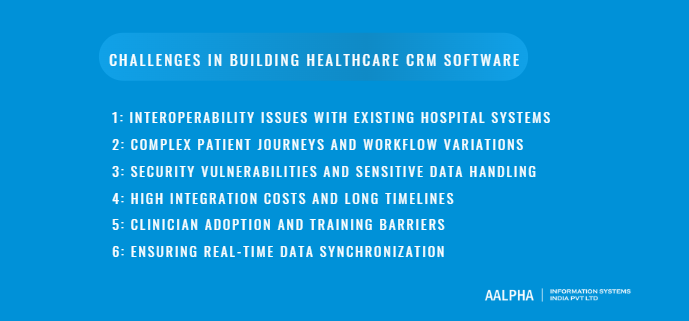
Challenges in Building Healthcare CRM Software
Building Healthcare CRM software is significantly more complex than creating traditional CRM systems because it must operate within a highly regulated, clinically sensitive, and operationally demanding environment. Healthcare organizations rely on accurate data, seamless interoperability, and consistent engagement to ensure high-quality care. A CRM, therefore, becomes the connective infrastructure linking administrative, clinical, and communication systems, which introduces technical and organizational challenges that product teams must anticipate early in the development process. The following sections outline the most critical challenges that arise when designing, integrating, and implementing enterprise-grade Healthcare CRM platforms.
-
Interoperability issues with existing hospital systems
One of the most persistent challenges in healthcare CRM development is achieving seamless interoperability across the diverse systems used within hospitals and clinics. Most healthcare organizations operate multiple systems: EHR/EMR platforms, billing tools, practice management systems, LIS, RIS, PACS, telehealth platforms, and various departmental applications. These systems were often implemented at different times, built on different architectures, and configured with proprietary data models.
Integrating a CRM into this ecosystem requires support for HL7, FHIR, DICOM, and vendor-specific APIs. However, many legacy systems are not fully compliant with modern standards or have limited API availability. As a result, CRM developers must build custom integration layers, data transformation engines, and reconciliation workflows to maintain consistency. Interoperability challenges also emerge when hospitals use multiple EMR systems across departments, requiring the CRM to harmonize data from fragmented sources. Without robust integration, the CRM risks becoming yet another silo rather than the unified engagement platform it is intended to be.
-
Complex patient journeys and workflow variations
Unlike industries with standardized customer journeys, healthcare involves highly diverse patient pathways shaped by medical conditions, specialties, treatment stages, and individual health needs. A cancer patient follows a vastly different journey from someone seeking dermatology care or chronic disease management. Additionally, workflows vary across hospitals, departments, and even individual clinicians.
Because of this complexity, CRM systems must be exceptionally flexible. They must support configurable workflows, branching logic, condition-specific pathways, automated reminders, personalized engagement, and role-based task assignments. Designing a CRM that accommodates dozens of specialties and hundreds of potential patient paths without overwhelming users requires a scalable workflow engine and deeply thought-out UX patterns.
Moreover, patient journeys are nonlinear. Patients may skip steps, receive conflicting information, or move between in-person and virtual care. The CRM must adapt dynamically, updating tasks and communication flows in real time. Mapping these variations into configurable system logic is one of the most difficult aspects of healthcare CRM design and often requires co-creation with clinical teams.
-
Security vulnerabilities and sensitive data handling
Healthcare data is one of the most targeted categories for cyberattacks. CRM systems store sensitive patient information, communication logs, clinical insights, billing details, and risk scores. Any vulnerability in this ecosystem can lead to serious legal and financial repercussions, especially under regulations such as HIPAA, GDPR, NABH, NHS DSPT, and regional health data laws.
Key security challenges include:
- Ensuring encryption of data at rest and in transit
- Implementing strict access controls such as RBAC and ABAC
- Maintaining comprehensive audit logs for every user action
- Protecting communication channels (WhatsApp, SMS, email) against unauthorized access
- Preventing injection, spoofing, and privilege escalation attacks
- Securing integrations with third-party APIs
- Managing identity and authentication across portals and mobile apps
Healthcare CRMs must also include breach detection, incident response workflows, and continuous monitoring. Because patient trust is foundational to care, even minor lapses can severely damage institutional reputation. As CRMs increasingly incorporate AI and automation, new attack surfaces emerge, requiring even stronger security governance.
-
High integration costs and long timelines
Healthcare CRMs demand extensive integration work that often surpasses the development complexity of the CRM itself. Connecting with EMR/EHR systems such as Epic, Cerner, Athenahealth, and regional EMRs requires deep technical expertise, vendor cooperation, and thorough testing. Many integrations involve custom HL7 interfaces, FHIR resource mapping, event-driven data syncing, and reconciliation workflows to handle conflicting or incomplete data.
Because of this complexity, integration work can extend development timelines significantly. Hospitals may also have outdated systems that require modernization or additional middleware. Data migration from legacy CRMs or manual records adds another layer of difficulty.
Costs also grow due to:
- Vendor licensing and API access fees
- Custom development for proprietary interfaces
- Required compliance audits and penetration testing
- Infrastructure scaling for high-volume messaging
- Ongoing maintenance to support regulatory changes
Organizations must realistically plan for integration-heavy timelines, recognizing that a fully interoperable CRM is a long-term investment rather than an immediate deployment.
-
Clinician adoption and training barriers
Even the most advanced CRM can fail if clinicians and support staff struggle to adopt it. Healthcare workflows are already burdened by documentation requirements, information overload, and tight schedules. Introducing a new system without thoughtful change management can create resistance or inconsistent usage.
Common adoption challenges include:
- Clinicians perceiving the CRM as adding extra steps
- Difficulty navigating complex dashboards
- Lack of alignment between CRM workflows and real-world clinical processes
- Insufficient hands-on training
- Variability in digital literacy among staff
- Alert fatigue from poorly configured notifications
Overcoming these barriers requires human-centered design, role-specific interfaces, and configurable workflows that match clinical realities. Comprehensive training, iterative onboarding, and user feedback loops dramatically improve adoption. Leadership support and clear communication about CRM benefits further reinforce trust and usage.
-
Ensuring real-time data synchronization
Healthcare engagement relies on accurate, up-to-date information. If a patient books an appointment in the hospital’s PMS, the CRM must reflect this change immediately to avoid sending incorrect reminders. If lab results arrive, the CRM must update workflows and alerts accordingly. Real-time synchronization is critical but technologically challenging.
Synchronization issues arise when:
- External systems update data asynchronously
- HL7 or FHIR messages fail or get delayed
- Conflicting records appear across systems
- Integration engines experience downtime
- APIs have rate limits that delay updates
Developers must build resilient sync mechanisms with retry logic, queuing, deduplication, and reconciliation processes. Event-driven architectures using message brokers (Kafka, RabbitMQ) help maintain real-time communication across distributed systems.
Without real-time sync, automated workflows may trigger inaccurate reminders, care plans may be outdated, and patients may receive conflicting instructions, undermining the CRM’s reliability and clinical credibility.
Cost of Healthcare CRM Software Development
The cost of developing Healthcare CRM software varies widely depending on the system’s complexity, the breadth of integrations, regulatory requirements, and organizational scale. Healthcare CRMs are inherently more expensive than general-purpose CRMs because they must support clinical workflows, meet strict compliance standards, and integrate with existing hospital infrastructure such as EHR/EMR, LIS, RIS, and billing systems. Understanding the cost components helps healthcare leaders plan budgets effectively and set realistic expectations for timelines and resource allocation. This section breaks down the primary cost factors, typical pricing ranges, ongoing expenses, and practical strategies for optimizing overall development investments.
Cost factors: complexity, modules, integrations, platforms
Several factors influence the total development cost of a Healthcare CRM:
- System Complexity and Scope
A CRM with basic features like patient records, appointment reminders, and communications is simpler and cheaper. However, systems with advanced workflows, AI-driven insights, automated patient journeys, and deep analytics require more architecture, engineering, and compliance work. - Number of Modules
Each module adds cost, such as:
- Lead management
- Referral workflows
- Care team collaboration
- Chronic care pathways
- Billing communication
- Patient portal
- AI features (triage, sentiment analysis, risk scoring)
- Analytics dashboards
More modules require additional UI development, backend logic, and testing cycles.
- Integrations with External Systems
Integrations often represent 30 to 50 percent of a healthcare CRM’s total cost. Connecting with systems like Epic, Cerner, Athenahealth, LIS/RIS, payment gateways, and insurance verification APIs requires specialized expertise and rigorous testing.
Complexity increases when:
- The hospital uses outdated or proprietary systems
- Many departments use different EMRs
- Bidirectional, real-time sync is required
- Data formats need normalization (HL7, FHIR, DICOM)
- Compliance Requirements
Regulations like HIPAA, GDPR, NABH, and NHS DSPT require encryption, access controls, audit logs, and secure infrastructure. Compliance adds cost through security audits, code hardening, and penetration testing. - Platform Choice
Development costs differ based on deployment models:
- Cloud-based CRM: Lower upfront cost but recurring cloud fees.
- On-premise CRM: Higher setup cost, infrastructure provisioning, and maintenance overhead.
- Hybrid models: Require more complex architecture and synchronization.
- Geographic Location of Development Team
Rates vary by region. Teams in North America or Western Europe cost significantly more than teams in Eastern Europe or India.
These cost drivers collectively determine the overall investment required for the CRM.
Estimated cost ranges for MVP, mid-size, enterprise-grade
MVP Healthcare CRM (USD 80,000 to 200,000+)
An MVP includes essential workflows such as:
- Patient profiles
- Appointment management
- Basic communication (SMS, WhatsApp, email)
- Lead and referral tracking
- Basic analytics
- Limited or one-way EMR integration
- HIPAA/GDPR-ready architecture
Suitable for clinics, small networks, or early-stage product pilots.
Mid-Size Healthcare CRM (USD 250,000 to 600,000+)
Includes:
- Full multi-channel communication engine
- Automated workflows and patient journeys
- Care team collaboration
- Two-way EHR/EMR integration
- Analytics dashboards
- Referral pipelines
- Patient portal with self-service
- Advanced role-based access controls
- Cloud-native infrastructure
Ideal for growing hospitals or multi-specialty networks that require robust operations.
Enterprise-Grade Healthcare CRM (USD 700,000 to 2 million+)
Built for large hospital networks, payers, or national-level healthcare organizations. Includes:
- Complex multi-department workflows
- Interoperability with EMR, LIS, RIS/PACS, PMS, billing systems
- Predictive AI engines
- RPA automation
- Multi-tenant architecture
- Population health analytics
- Extensive compliance hardening
- Disaster recovery, uptime SLAs, load balancing
- Custom portals for patients, physicians, and partners
Costs can exceed USD 2 million for highly customized, large-scale deployments.
Ongoing costs: maintenance, infrastructure, API usage
Healthcare CRMs require continuous operational expenditures after launch. These include:
- Maintenance and Enhancements (15–25 percent of development cost annually)
Covers bug fixes, module upgrades, new feature requests, compliance updates, and performance improvements. - Cloud Infrastructure (USD 1,000 to 10,000+ per month)
Depends on:
- User volume
- Data storage
- Messaging throughput
- Integrations and APIs
- Redundancy and uptime requirements
Enterprise deployments with large patient populations will incur higher cloud usage.
- API Usage Fees
Common recurring costs:
- WhatsApp Business API
- SMS gateways
- Email delivery services
- EHR/EMR vendor API fees
- AI engines or analytics platforms
- Payment gateway transaction charges
- Security and Compliance Audits
Regular penetration tests, SOC 2 audits, and HIPAA assessments are essential for maintaining trust and compliance. - Licensing Costs (if using third-party modules)
Hospitals may require licenses for interoperability engines, analytics tools, or communication platforms.
Comparing in-house development vs outsourcing
In-House Development
Pros:
- Complete control over architecture and product roadmap
- Full alignment with internal workflows
- Better long-term customization
Cons:
- Very expensive due to salaries, benefits, and turnover
- Hard to hire specialized roles (HL7/FHIR engineers, security experts, UX researchers)
- Slow time-to-market
- Risk of knowledge gaps or technical debt
Outsourcing to a Healthcare-Focused Development Partner
Pros:
- Access to specialized healthcare engineers experienced with HIPAA, HL7, FHIR
- Lower cost compared to in-house teams
- Faster development cycles
- Ability to scale teams up or down
- Exposure to best practices and prebuilt integration patterns
Cons:
- Requires strong project management
- Need clear documentation and communication
- Vendor lock-in risk if not managed correctly
Hybrid models work best: define product ownership internally while outsourcing development and integrations to experienced partners.
How to optimize development costs
Organizations can reduce CRM development expenses through strategic planning:
- Build an MVP and Expand Gradually
Focus on high-value workflows first. Add advanced modules (AI, chronic care pathways, portals) after validating core operations. - Use Prebuilt Integration Frameworks
Adopting existing HL7/FHIR integration engines shortens timelines and reduces custom work. - Leverage Open-Source Components
Workflow engines, BI tools, and communication modules can be partially built using open-source frameworks. - Avoid Over-Customization Early
Start with standardized workflows and refine based on usage patterns. - Use Cloud-Native Infrastructure
Cloud platforms optimize costs with auto-scaling, managed databases, and built-in security. - Prioritize Automation
Automated testing, CI/CD pipelines, and infrastructure-as-code reduce long-term maintenance burdens. - Expand in Phases Across Departments
A phased rollout avoids overwhelming staff and spreads costs over time.
Why Choose Aalpha for Healthcare CRM Software Development
Aalpha stands out as a trusted partner for Healthcare software development because of its deep domain expertise, strong technical capabilities, and proven experience in building secure, compliant, and workflow-driven healthcare systems. Unlike generic software firms, Aalpha understands the operational realities of hospitals, multi-specialty clinics, diagnostics networks, and telehealth providers. This enables the team to design CRM platforms that genuinely improve patient engagement, streamline referrals, reduce no-shows, and support care teams with intuitive interfaces and intelligent workflows. Aalpha’s engineers work extensively with HL7, FHIR, DICOM, HIPAA, GDPR, NABH, and NHS-aligned protocols, ensuring the CRM integrates seamlessly with EHR/EMR systems, LIS/RIS, pharmacy systems, billing platforms, and communication channels like WhatsApp, SMS, email, and IVR. With security and compliance embedded into every architectural layer, Aalpha delivers CRMs that are robust, interoperable, and ready for enterprise-scale deployment.
Beyond technical precision, Aalpha brings a strong product mindset focused on automation, AI-driven insights, and future-ready scalability. The team builds CRMs equipped with predictive analytics, automated patient journeys, care coordination dashboards, and sentiment-aware communication tools that elevate both patient experience and operational efficiency. Aalpha also emphasizes UI/UX tailored to clinicians, care managers, and administrative staff, ensuring the CRM fits naturally into daily workflows rather than adding friction. With transparent project management, agile delivery, and long-term support, Aalpha becomes an extension of the client’s digital transformation team. This combination of healthcare knowledge, engineering excellence, and partnership-driven execution makes Aalpha a leading choice for organizations seeking a high-performance, custom Healthcare CRM solution.
Future of Healthcare CRM
The future of Healthcare CRM is defined by a shift from passive data repositories to intelligent, autonomous systems that orchestrate patient engagement, predict care needs, and integrate seamlessly across physical and digital environments. As healthcare systems worldwide embrace digital transformation, CRM platforms will evolve into the command centers for patient experience, clinical coordination, and population health management. The combination of AI, automation, interoperability, and consumer-centric design will reshape how healthcare organizations communicate, deliver care, and measure outcomes. The following sections examine the key trends shaping the next decade of Healthcare CRM evolution.
Predictive healthcare and AI-first CRM
AI will transform Healthcare CRM systems into proactive engines capable of predicting patient needs before they arise. Instead of reacting to scheduled visits or patient inquiries, AI-first CRMs will continuously analyze historical data, behavioural patterns, clinical indicators, and population-level risk models to anticipate health events.
Key advancements include:
- No-show prediction models that identify patients who require early interventions or personalized reminders.
- Readmission risk monitoring driven by clinical and behavioural data.
- Predictive triage capable of analyzing symptoms, medical history, and messaging patterns to categorize urgency.
- Next-best-action engines that guide clinicians and care teams on when to escalate, intervene, or communicate.
AI-first CRM systems will act as autonomous assistants that orchestrate workflows across clinical and administrative teams, reducing manual workload and improving care outcomes. As healthcare organizations increasingly adopt LLM-based agents, these CRMs will become active decision-support hubs capable of adapting to changing patient needs in real time.
Integration with wearable devices and IoT
Wearables and connected medical devices are becoming central to chronic disease management, preventive care, and remote patient monitoring. As device adoption grows, Healthcare CRMs will integrate directly with IoT ecosystems to capture continuous patient data from smartwatches, glucometers, ECG patches, pulse oximeters, home blood pressure monitors, and hospital-grade IoT devices.
The CRM will serve as the central point where:
- Biometric data is aggregated into personalized dashboards.
- Abnormal readings trigger alerts to care teams.
- Patients receive automated nudges for lifestyle adjustments or medication adherence.
- Care plans evolve dynamically based on real-time physiological insights.
These IoT–CRM integrations will allow providers to shift from episodic care to continuous monitoring models. Instead of waiting for clinical deterioration, teams will intervene early, reducing hospital admissions and improving long-term outcomes. Wearable data, combined with AI-driven analytics, will unlock hyper-personalized patient journeys and enable scalable chronic care programs.
Fully automated patient journeys
Automation will become the driving force behind next-generation healthcare CRM platforms. Today’s automated reminders and basic workflows represent only the beginning. Future CRMs will support fully automated patient journeys spanning diagnostics, pre-treatment workflows, surgical care, rehabilitation, and long-term follow-up.
These journeys will adapt dynamically based on patient behaviour, clinical results, and real-time system events. Examples include:
- Preoperative pathways that automatically dispatch instructions, videos, checklists, and safety reminders.
- Chronic care pathways that adjust communication frequency based on remote monitoring trends.
- Post-discharge workflows that detect when a patient hasn’t filled a prescription or missed a follow-up appointment.
- AI-powered education flows that personalize content for each patient’s condition, age, and literacy level.
Automation will reduce administrative load, improve adherence, and create scalable care frameworks that do not depend on manual staff intervention. Eventually, automated journeys will integrate predictive models, enabling the CRM to personalize timing, communication channels, and instructions for each patient.
Unified patient experience across channels
The future of Healthcare CRM is omnichannel by default. Patients will interact with healthcare organizations through messaging apps, mobile apps, patient portals, kiosks, call centers, telehealth platforms, and wearables. A unified CRM will centralize all these interactions to create a connected, consistent patient experience.
This unified experience includes:
- Seamless data continuity as patients move between physical visits, telehealth, and remote care.
- Cross-channel messaging where a conversation started in WhatsApp can continue in the patient portal with full context.
- Integrated identity management enabling patients to authenticate once across all channels.
- Real-time personalization where the CRM adjusts communication tone, timing, and recommendations based on channel preferences.
Healthcare organizations will increasingly use CRM frameworks to deliver consumer-grade engagement similar to e-commerce and fintech platforms. The CRM will evolve into a patient experience platform that unifies care navigation, communication, education, and support.
Rise of healthcare CRM-as-a-Service platforms
As the demand for digital transformation accelerates, hospitals and healthcare startups are shifting away from building CRMs from scratch. Instead, they are adopting Healthcare CRM-as-a-Service platforms that provide out-of-the-box compliance, integrations, and modular workflows.
Key drivers of this shift include:
- Cost-efficiency: CRM-as-a-Service significantly reduces upfront development expenses.
- Rapid deployment: Ready-to-use modules accelerate digital adoption.
- Built-in interoperability: Pre-integrated HL7/FHIR connectors and communication APIs eliminate technical complexity.
- Scalability: Cloud-native architectures support rapid expansion across departments or locations.
- Continuous updates: Platforms receive frequent compliance, security, and feature updates without burdening internal teams.
These platforms resemble the evolution of ERP and HR systems, where organizations moved from custom builds to standardized yet configurable SaaS solutions. CRM-as-a-Service will dominate healthcare within the next few years, especially for organizations needing advanced automation, AI-driven workflows, and robust omnichannel engagement without extensive engineering investment.
Conclusion
Healthcare CRM software has evolved from a simple patient database into a mission-critical platform that shapes how healthcare organizations communicate, coordinate, and deliver care. As the healthcare ecosystem becomes more complex, digital-first, and patient-centric, CRM systems provide the foundation for managing the entire patient lifecycle with consistency, personalization, and operational precision. They bring together clinical data, communication channels, workflows, analytics, and AI into one unified environment, enabling providers to deliver care that is not only efficient but also deeply human-centered.
Throughout this guide, we examined every dimension of Healthcare CRM development: market trends, regulatory requirements, core and advanced features, technical architecture, integration challenges, cost structures, and long-term opportunities. Two themes appear consistently. First, healthcare organizations cannot scale modern care delivery without structured automation and integrated digital systems. Second, the value of a CRM multiplies when it is tightly connected with EHRs, telehealth, labs, pharmacies, and communication platforms, creating a seamless environment where the patient remains at the center of every interaction.
The future of healthcare CRM is defined by intelligence and autonomy. AI-driven predictive analytics, automated care journeys, sentiment monitoring, and integrations with IoT devices will transform CRMs from passive record systems into proactive orchestration engines. Instead of waiting for patients to engage, CRM systems will guide them through personalized paths, detect risks early, and support care teams with real-time insights. For healthcare leaders, the choice is no longer whether to invest in CRM technology but how quickly they can adopt a platform capable of supporting tomorrow’s care models.
For organizations planning to build or modernize their CRM, the key is clarity. Clear requirements, strong clinical workflow mapping, early integration planning, and measurable outcomes create the foundation for a successful project. Choosing the right development partner or internal team with healthcare expertise is equally critical. A well-implemented CRM does more than streamline operations; it elevates patient satisfaction, improves care quality, strengthens referral networks, and positions providers for value-based care.
Back to You!
If your organization is exploring Healthcare CRM software development, now is the time to take the next step. Whether you are evaluating a new digital transformation initiative, planning to modernize outdated systems, or building a custom CRM tailored to your clinical workflows, expert guidance can dramatically accelerate your progress and reduce risk.
Aalpha Information Systems specializes in building secure, scalable, and compliance-ready Healthcare CRM solutions tailored to hospitals, clinics, telehealth providers, and healthcare startups. Our team brings deep experience in EMR/EHR integration, HIPAA/GDPR compliance, automated patient journeys, and multi-channel engagement systems designed for both clinical and administrative users.
If you are ready to transform your patient engagement and operational workflows, connect with us for a detailed consultation.