What is an AI Patient Intake Agent?
An AI patient intake agent is a digital system powered by artificial intelligence that automates the process of gathering, verifying, and managing patient information before a medical consultation. Instead of relying on paper forms or manual data entry, these agents interact directly with patients through natural language—via WhatsApp, SMS, web portals, or in-clinic kiosks. They can collect demographics, medical history, insurance details, and consent forms, and then seamlessly transfer that data into a clinic’s electronic health record (EHR) or practice management system.
Unlike traditional chatbots, AI intake agents are context-aware. They use natural language processing (NLP) to understand patient responses, apply machine learning to verify accuracy, and integrate with healthcare databases to ensure compliance and consistency. For example, if a patient mentions they have diabetes, the agent not only records it but also prompts for related information such as current medications, last HbA1c test, or allergies. This structured, intelligent intake process reduces administrative workload and increases the accuracy of medical records.
In short, an AI intake agent serves as a virtual front-desk assistant—always available, multilingual, and capable of handling multiple patients simultaneously without fatigue or human error.
TL;DR
AI patient intake agents automate registration, form filling, insurance verification, and EHR integration to reduce wait times, cut data entry errors, improve compliance, and enhance patient satisfaction. They bring measurable ROI within 6–18 months by lowering costs, reducing claim denials, and increasing throughput. Small clinics use them to ease admin burden, large hospitals to scale intake across departments, and telehealth providers to streamline virtual onboarding. With features like pre-registration, multichannel access (WhatsApp, SMS, web, kiosks), predictive analytics, IoT integration, and voice-based intake, they are shaping the future of patient-centered healthcare. Partnering with experienced providers like Aalpha Information Systems ensures secure, scalable, and customized solutions.
Why Clinics Are Adopting AI for Front-Office Automation
Healthcare providers across the globe are facing mounting administrative pressures. A significant portion of staff time is consumed by repetitive tasks: handing out forms, verifying patient details, answering the same questions, and transcribing data into medical systems. These tasks are essential but add little value to actual clinical care.
AI intake agents address this gap by automating the entire front-office process. Clinics adopt them for several reasons:
- Operational efficiency: By digitizing and automating intake, staff are freed to focus on patient-facing tasks such as coordination, counseling, or urgent care needs.
- Scalability: Small clinics often lack staff to manage peak hours, while large hospitals struggle with hundreds of daily intakes. AI can scale without proportional cost increases.
- Accuracy and compliance: AI systems minimize transcription errors, flag missing fields, and maintain compliance with HIPAA or GDPR by ensuring structured and encrypted data flow.
- Patient expectations: As consumers grow accustomed to digital-first services in banking, retail, and travel, they expect similar convenience from healthcare. Self-service AI intake matches this expectation.
In practical terms, a clinic that previously needed three front-desk staff to handle registration during rush hours can now operate with fewer personnel without compromising patient experience. The AI agent works in parallel, checking insurance details or guiding patients through consent forms while staff handle emergencies or complex inquiries.
Benefits for Patients, Doctors, and Staff
-
Benefits for Patients
Patients are the most immediate beneficiaries of AI intake systems. Instead of waiting in line or repeatedly filling out forms, they can complete the process on their phone before arriving at the clinic. This reduces waiting times, ensures smoother appointments, and minimizes the frustration of repeated paperwork. Multilingual support makes healthcare more inclusive, particularly in communities where language barriers can deter patients from seeking care.
AI intake agents also provide transparency. Patients can review and correct their data instantly, receive reminders about missing details, and access clear instructions about what to bring for their appointment, such as prior test reports or ID cards. The result is a more informed and less stressful patient journey.
-
Benefits for Doctors
For doctors, the biggest advantage is receiving accurate, structured data before a consultation begins. Instead of spending the first ten minutes of an appointment gathering history, physicians can immediately focus on diagnosis and treatment. An AI intake agent can also flag potential risks, such as drug interactions or chronic conditions, providing doctors with valuable context at a glance.
This streamlined process not only improves efficiency but also enhances clinical decision-making. Physicians spend more time on patient care and less on documentation, ultimately improving outcomes and patient satisfaction.
-
Benefits for Staff
Front-desk and administrative staff often bear the brunt of patient frustration during long wait times. By automating repetitive intake tasks, AI reduces pressure on staff and allows them to focus on higher-value interactions. Instead of data entry, staff can assist elderly patients, resolve complex scheduling conflicts, or support clinicians with urgent needs.
Moreover, reducing human error in patient records protects staff from liability and saves time previously spent on corrections. In large healthcare facilities, this translates into significant cost savings and smoother operations across departments.
AI patient intake agents represent more than just a technological upgrade; they are a fundamental shift in how clinics interact with patients. By combining automation, natural language communication, and secure integration with medical systems, these agents eliminate inefficiencies that have long hindered patient care. Clinics adopting AI for front-office automation not only improve their bottom line but also create a more patient-centric healthcare experience—where waiting times shrink, data accuracy improves, and staff and doctors can focus on what matters most: delivering quality care.
Current Challenges in Patient Intake Without AI
The patient intake process is often the first point of interaction between a clinic and its patients. Unfortunately, in many healthcare facilities, this experience is marked by inefficiency, delays, and frustration. Traditional intake systems—whether paper-based or partially digitized—struggle to keep up with modern expectations for speed, accuracy, and convenience. Understanding these challenges is critical to appreciating why AI-powered intake agents are becoming a necessity rather than a luxury.
-
Long Wait Times and Patient Dissatisfaction
One of the most visible challenges in traditional intake is the long waiting period patients face before seeing a doctor. The process typically begins with registration, form filling, insurance checks, and manual verification—all before the patient even enters the consultation room. Each of these steps adds time, and when multiplied across dozens or hundreds of patients per day, delays can become overwhelming.
Long wait times have a direct impact on patient satisfaction. Research consistently shows that excessive waiting is one of the top complaints in healthcare. Patients perceive long waits as a sign of inefficiency and poor service, regardless of the quality of medical care they eventually receive. In high-pressure environments such as emergency rooms or multi-specialty clinics, delays can even worsen health outcomes, as conditions that require timely intervention may be pushed back by administrative bottlenecks.
Furthermore, the stress of waiting in crowded lobbies can discourage patients from returning for follow-up visits or adhering to preventive care schedules. In competitive healthcare markets, where patients can choose among several providers, long waits can drive patients to seek care elsewhere, affecting both revenue and reputation.
-
Manual Data Entry Errors and Inefficiencies
Traditional intake relies heavily on manual data entry. Patients often fill out paper forms, which staff must then transcribe into electronic health records (EHRs). This dual-step process introduces multiple points of failure. Handwritten forms may be illegible, details may be skipped, and staff may inadvertently enter incorrect information. Common mistakes include spelling errors in patient names, misreporting of allergies or medications, and incorrect insurance details.
These errors can have serious consequences. Inaccurate records may lead to misdiagnosis, medication conflicts, or billing disputes. Correcting errors requires additional staff time and resources, leading to operational inefficiency. For example, a simple typo in an insurance ID may require repeated calls to insurers, delaying claims processing and increasing administrative overhead.
Manual intake also wastes valuable staff hours. Instead of focusing on high-value activities such as coordinating care or assisting patients with special needs, staff are tied down by repetitive clerical tasks. This not only reduces productivity but also contributes to job dissatisfaction and burnout, particularly in busy clinics with limited administrative support.
-
Compliance and Documentation Gaps
Healthcare providers are bound by strict regulatory frameworks, such as HIPAA in the United States and GDPR in Europe, which require proper handling, storage, and sharing of patient data. Unfortunately, manual intake processes often fall short of these standards. Paper forms may be misplaced, left unattended at the front desk, or stored insecurely. Staff handling may also be inconsistent, with varying levels of training on compliance protocols.
Documentation gaps are another issue. Missing consent forms, incomplete medical histories, or improperly filed insurance documents can all expose a clinic to compliance risks and potential legal liabilities. Regulatory audits or disputes with insurers may reveal deficiencies in how data was collected, recorded, or stored. In the worst cases, data breaches or privacy violations can result in hefty fines and reputational damage.
These compliance challenges are particularly pressing as healthcare shifts toward digital-first ecosystems. Patients increasingly expect that their information will be handled securely and that they won’t have to repeatedly provide the same data across visits. Traditional intake systems often fail to deliver on this expectation, creating friction and mistrust between patients and providers.
-
Hidden Costs of Traditional Intake Processes
While the inefficiencies of manual intake are visible in patient frustration and staff workload, there are also substantial hidden costs that clinics may overlook. These include:
- Labor costs: Clinics must hire additional staff to manage data entry, verification, and error correction. Over time, this inflates operational expenses.
- Paper and storage expenses: Maintaining physical forms requires printing, filing cabinets, and long-term storage, all of which add recurring costs.
- Claim denials and revenue leakage: Inaccurate intake data often leads to insurance claim denials, which can delay or reduce reimbursement. Reprocessing denied claims consumes additional staff time and may still result in lost revenue.
- Patient attrition: Dissatisfied patients who leave due to poor intake experiences indirectly cost the clinic in lost lifetime value and negative word-of-mouth.
For example, a mid-sized clinic that handles 100 patients daily may lose thousands of dollars per year simply due to inefficiencies in intake. These costs are not always visible in financial statements but accumulate over time, eroding profitability and reducing resources available for clinical improvements.
The traditional patient intake process is riddled with inefficiencies that affect every stakeholder in the healthcare ecosystem. Patients are forced to endure long waits, doctors receive incomplete or inaccurate data, staff are burdened with repetitive tasks, and clinics face compliance risks and hidden costs. These challenges make a compelling case for modernizing intake workflows.
AI-powered patient intake agents directly address these pain points by eliminating manual inefficiencies, reducing wait times, ensuring compliance, and lowering operational costs. Before exploring how to implement such a system, it is essential to understand the depth of the problem—and why sticking to traditional methods is no longer sustainable in a healthcare environment that demands speed, accuracy, and patient-centered service.
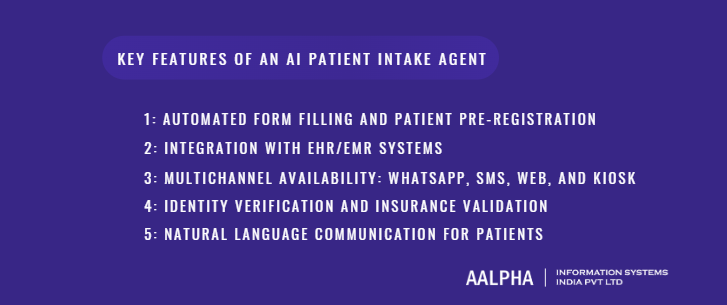
Key Features of an AI Patient Intake Agent
An AI-powered patient intake agent is far more than a digital form; it is a smart, context-aware assistant designed to simplify how patients interact with healthcare providers. The most effective solutions combine automation, integration, and conversational intelligence, ensuring that the patient journey begins smoothly and efficiently. Below are the core features that define a robust AI intake agent.
-
Automated Form Filling and Patient Pre-Registration
One of the most time-consuming aspects of traditional intake is filling out forms—demographic details, medical history, allergies, insurance information, and consent documents. Patients often complete these forms in waiting rooms, under time pressure, and sometimes multiple times if they visit different departments. Staff must then manually enter the information into digital systems, creating bottlenecks and errors.
AI intake agents automate this process by enabling pre-registration. Patients can provide their details online before their appointment, through a secure web link or messaging platform. The agent dynamically guides patients, asking only the relevant questions based on previous responses. For example, if a patient indicates they have asthma, the system will prompt follow-up questions about inhaler use or recent hospitalizations.
Additionally, AI can autofill forms by retrieving data from previous visits or integrated databases. Returning patients no longer need to re-enter information, and updates—such as changes in address, phone number, or insurance provider—are seamlessly merged. This automation not only reduces wait times but also ensures clinicians have complete, accurate records before the consultation begins.
-
Integration with EHR/EMR Systems
The true value of an AI intake agent lies in its ability to integrate with a clinic’s existing Electronic Health Record (EHR) or Electronic Medical Record (EMR) systems. Without integration, intake automation remains a silo, requiring manual uploads or cross-checks, which defeats the purpose of streamlining workflows.
Modern AI agents connect directly to EHR platforms like Epic, Cerner, Athenahealth, or custom practice management software. Through secure APIs, the agent can push patient data—including demographics, medical history, and consent—directly into the right fields. This ensures that doctors and nurses have immediate access to structured, standardized information.
Integration also supports real-time updates. For example, if a patient changes their pharmacy preference or updates their insurance provider, the EHR reflects those changes instantly, avoiding downstream errors in prescriptions or billing. In addition, some systems allow bi-directional communication, where the AI intake agent can pull relevant historical data from the EHR to pre-populate intake forms or personalize questions.
This seamless data flow improves efficiency, reduces duplication, and enhances patient safety by ensuring the care team works with accurate, up-to-date information at all times.
-
Multichannel Availability: WhatsApp, SMS, Web, and Kiosk
Patients differ widely in their comfort with technology. While some prefer mobile-first interactions, others may feel more comfortable with a web form or a physical kiosk in the clinic. A key strength of modern AI intake agents is multichannel availability, which ensures accessibility for all patient demographics.
- WhatsApp and SMS: Messaging platforms are especially powerful for intake because they are familiar, easy to use, and do not require downloading a new app. Patients can confirm appointments, complete intake forms, or upload documents directly through their phones. This channel is particularly effective in regions where smartphone penetration is high but patients avoid specialized healthcare apps.
- Web portals: For patients who prefer completing intake at their convenience, web-based portals provide a secure environment. These can be customized to reflect the clinic’s branding and allow for multimedia inputs such as scanned reports or digital consent signatures.
- In-clinic kiosks: For patients who do not complete intake ahead of time, self-service kiosks can be placed in waiting areas. These devices are designed for accessibility, with large fonts, multilingual options, and touch interfaces, enabling quick and independent form completion.
By offering a choice of channels, clinics remove barriers to adoption and improve overall compliance with intake requirements. This flexibility is crucial in diverse patient populations where age, literacy, and digital access vary widely.
-
Identity Verification and Insurance Validation
Accurate identity verification is essential to prevent medical errors, fraudulent claims, and compliance violations. In traditional workflows, staff manually check photo IDs and insurance cards, which is time-intensive and prone to oversight.
AI intake agents can automate identity verification using methods such as:
- Optical Character Recognition (OCR) to scan government-issued IDs.
- Biometric verification through facial recognition or fingerprints where regulations allow.
- Two-factor authentication (2FA) via secure SMS or email codes.
Beyond identity, insurance validation is another critical feature. AI agents can automatically check the validity of insurance policies by connecting with payer databases or clearinghouses. Instead of discovering insurance issues at the billing stage, clinics can identify eligibility problems upfront—reducing claim denials and financial disputes.
For patients, this means fewer surprises about coverage or out-of-pocket costs. For clinics, it ensures accurate billing and faster reimbursements, significantly reducing revenue leakage associated with manual verification errors.
-
Natural Language Communication for Patients
The defining characteristic of an AI patient intake agent is its ability to interact naturally with patients. Unlike rigid digital forms, AI agents employ Natural Language Processing (NLP) to understand and respond to patient inputs conversationally.
For example, if a patient types, “I’ve been having severe headaches for three weeks,” the agent doesn’t just capture “headache” as a symptom. It recognizes duration, severity, and context, then follows up with clarifying questions such as, “Do these headaches occur at a specific time of day?” or “Are you currently taking any medication for pain relief?”
This natural interaction reduces friction, especially for patients who may feel overwhelmed by long forms or unfamiliar medical terminology. Instead of struggling to fill out a checklist, patients communicate in their own words, and the AI translates this into structured clinical data for doctors.
Multilingual support further enhances accessibility. Clinics in diverse communities can configure agents to interact in multiple languages, making healthcare more inclusive. For patients with disabilities, agents can support voice-to-text or text-to-voice interactions, ensuring no one is left out of the digital transformation.
The effectiveness of an AI patient intake agent lies in the combination of these features: automation, integration, accessibility, verification, and natural communication. Each feature addresses a specific pain point of traditional intake systems, from reducing waiting times to eliminating data entry errors and ensuring compliance.
Together, they redefine the intake process into a seamless, patient-centric experience. Patients enjoy shorter waits and greater convenience, staff are relieved of repetitive tasks, and doctors receive cleaner, more reliable data. For clinics, this translates into better operational efficiency, reduced costs, and stronger patient loyalty.
Implementing an intake agent is not just about adopting new technology—it is about building the foundation for a smarter, more responsive healthcare ecosystem that meets the needs of modern patients while supporting clinical excellence.
AI Patient Intake Agent Implementation Step-by-Step Process
Implementing an AI patient intake agent in a clinic is not a plug-and-play exercise. It requires careful planning, integration, and change management to ensure that the technology delivers value without disrupting daily operations. For clinics looking to build healthcare AI agents, the following seven steps provide a structured roadmap to successfully adopt AI intake agents.
-
Assessing Clinic Needs
The first step in implementing an AI patient intake agent is conducting a comprehensive needs assessment. No two clinics operate the same way: a single-specialty dermatology practice will have very different intake requirements than a multi-specialty hospital. Before committing to technology, clinic leaders must evaluate current processes and identify where inefficiencies and pain points exist.
Key questions include:
- How long does the average intake process currently take?
- What percentage of patient records contain errors or missing data?
- Where are the biggest sources of patient dissatisfaction (e.g., waiting time, form complexity)?
- Which staff tasks are most repetitive and could be automated?
Gathering this baseline information allows clinics to establish benchmarks. For example, if the current average wait time is 25 minutes, the goal might be to reduce it to under 10 minutes. If claim denials due to intake errors are at 15 percent, the target could be to cut that figure in half.
This stage should also consider regulatory requirements and patient demographics. A clinic serving multilingual communities may prioritize language support, while one focused on chronic care may emphasize detailed medical history capture. Engaging frontline staff during this phase is critical—they can provide insights into bottlenecks and identify features that would bring immediate relief.
Ultimately, a clear understanding of needs helps ensure that the AI solution is not adopted for novelty but as a targeted tool aligned with measurable outcomes.
-
Choosing the Right AI Platform
Once the clinic’s requirements are clear, the next step is selecting an AI platform that meets both functional and compliance needs. The choice of platform determines the scalability, cost, and overall effectiveness of the intake system.
Key criteria include:
- Integration capabilities: Does the platform support seamless APIs with existing EHR/EMR systems? Without this, staff may still have to re-enter data.
- Multichannel support: Can the AI agent operate across WhatsApp, SMS, web portals, and kiosks to serve different patient groups?
- Customization flexibility: Can workflows be tailored for different specialties (e.g., pediatrics vs. cardiology)?
- Security and compliance: Does the platform support HIPAA, GDPR, or other applicable data protection regulations? Encryption and audit trails should be standard.
- User experience: Is the interface intuitive for patients across age groups, literacy levels, and technical comfort?
There are typically two options:
- Off-the-shelf solutions: These are pre-built platforms that offer quick deployment but may have limited customization. They are ideal for smaller clinics looking for basic automation.
- Custom-built solutions: These are tailored systems developed specifically for a clinic’s workflows. They require higher upfront investment but deliver long-term flexibility and integration.
Clinics must also evaluate vendor support. A strong vendor provides not just software but also ongoing maintenance, updates, and training. Requesting demonstrations and pilot programs from multiple vendors allows decision-makers to compare usability, feature sets, and pricing before making a final selection.
-
Data Collection and Pre-Implementation Planning
The success of any AI system depends on the quality of data it handles. Before implementation, clinics must conduct data preparation and planning. This involves both technical and operational activities.
First, existing patient data should be audited for completeness and accuracy. Missing records, outdated insurance information, or inconsistent formatting can all undermine the performance of an AI intake agent. For example, if addresses are stored in multiple formats (“Street” vs. “St.”), the AI may struggle to match records accurately. A data-cleaning exercise ensures consistency.
Second, clinics should identify the types of data the intake agent will collect: demographics, insurance details, consent, allergies, symptoms, and prior visits. Each data category must be mapped to the corresponding fields in the EHR system to enable smooth integration.
Third, pre-implementation planning requires establishing policies and protocols. Who will oversee the AI agent? How will exceptions—such as incomplete forms or patients unable to use digital tools—be handled? Will the clinic maintain hybrid workflows during the transition?
Patient communication is also vital. Informing patients in advance about the upcoming AI intake system builds trust and reduces resistance. Simple messaging—such as “Now complete your forms at home on your phone to save waiting time”—can generate excitement rather than confusion.
This step creates a strong foundation, ensuring that when the AI system is activated, it functions smoothly and meets both clinical and patient expectations.
-
Integration with EHR and Existing Systems
Perhaps the most technically complex phase is integration with EHR and other clinic systems. An AI intake agent has limited value if the data it collects cannot be securely and automatically synchronized with existing platforms.
Integration typically involves:
- API connections: Secure APIs allow the AI intake system to push structured data directly into the EHR without manual input. This requires compatibility between the agent and the clinic’s chosen EHR provider.
- Data mapping: Intake fields must align precisely with EHR fields. For example, “Patient Phone Number” should not overwrite “Emergency Contact Phone Number.” Mapping prevents data loss or duplication.
- Real-time syncing: Ideally, data should update in real time, ensuring clinicians see the latest patient information before appointments. Batch uploads may be acceptable in low-volume clinics but are inefficient for larger facilities.
- Interoperability with third-party systems: Beyond EHRs, intake agents may need to communicate with billing platforms, insurance verification services, or patient portals.
Security is paramount. Integration must use encrypted transmission protocols and comply with regional health IT standards such as HL7 or FHIR. Audit logs should record all data exchanges for regulatory compliance.
Clinics should involve both healthcare software development teams and clinical staff during this stage. While IT ensures technical integrity, clinicians validate that the data appears in usable formats. A phased integration—starting with one department or a small patient cohort—helps identify and resolve issues before scaling across the entire organization.
When executed correctly, integration eliminates redundant tasks, ensures doctors have complete information, and creates a unified data environment that supports both clinical and administrative workflows.
-
Workflow Automation and Customization
Once integration is complete, clinics must customize workflows to align with their unique needs. AI intake agents are highly flexible; they can be configured to adapt to specialty-specific requirements, patient demographics, and clinic policies.
Examples of customization include:
- Specialty-driven workflows: A cardiology clinic may require detailed information on blood pressure, cholesterol levels, and heart history, while a dermatology practice focuses on skin conditions, allergies, and prior treatments.
- Conditional logic: The AI can ask follow-up questions based on patient inputs. If a patient reports pregnancy, the system prompts for obstetric history.
- Insurance routing: The agent can guide patients through different insurance questions based on the provider they select.
- Language and accessibility settings: Multilingual support and voice-enabled features can be activated depending on patient demographics.
Automation also extends to follow-up actions. Once intake is complete, the AI can automatically trigger appointment reminders, send instructions (e.g., fasting before a test), or route data to billing teams.
This stage ensures that the AI agent is not a generic solution but a clinic-specific digital assistant that reflects the realities of daily operations. Customization also increases patient compliance, as they interact with an agent that feels relevant and user-friendly.
-
Testing, Pilot Rollout, and Feedback
Before full deployment, clinics should conduct a pilot rollout to test the AI intake agent in a controlled environment. This approach minimizes risk and allows for adjustments based on real-world usage.
A pilot typically involves:
- Selecting a small patient group: For example, only new patients in a single department.
- Monitoring key metrics: Wait times, error rates, patient satisfaction, and staff feedback are tracked to measure performance against benchmarks.
- Collecting qualitative feedback: Patients can be surveyed about ease of use, while staff can report whether the data presented in the EHR is accurate and complete.
- Iterative improvement: Feedback is used to fine-tune the AI agent, such as rewording confusing questions or adding additional follow-ups for clinical completeness.
Pilots also reveal unexpected challenges, such as connectivity issues in kiosks, older patients struggling with digital tools, or insurance data mismatches. Identifying these problems early prevents them from scaling across the entire patient population.
By approaching implementation incrementally, clinics build confidence in the system, earn staff buy-in, and ensure that the technology is genuinely improving workflows rather than creating new burdens.
-
Full Deployment and Staff Training
The final step is full deployment across the clinic, supported by comprehensive staff training. Even the most advanced AI intake agent will fail if staff are not comfortable using it or do not understand its value.
Deployment involves rolling out the AI system to all patient groups, communication channels, and departments. To support adoption, clinics must invest in structured training programs. These should cover:
- How the AI agent interacts with patients and how staff can monitor or intervene if needed.
- Data flow: how intake information appears in the EHR and how to correct errors if they occur.
- Patient communication: equipping staff with scripts to explain the new process to patients, especially those hesitant about AI.
- Escalation procedures: what to do when patients cannot or will not use the AI system.
Ongoing training is equally important. As AI agents evolve and workflows expand, staff must remain informed of updates. Establishing a dedicated support team or vendor liaison ensures that technical issues are resolved quickly.
Finally, clinics should continue to measure performance post-deployment, using KPIs such as patient satisfaction scores, reduced claim denials, and time saved per intake. Celebrating early wins—such as cutting wait times in half—reinforces the system’s value and motivates staff to embrace the change.
Implementing an AI patient intake agent is a strategic transformation, not just a technology upgrade. By following a structured process—assessing needs, selecting the right platform, preparing data, integrating systems, customizing workflows, testing thoroughly, and training staff—clinics can maximize both clinical and financial benefits.
When executed properly, AI intake agents deliver measurable improvements: shorter waits, fewer errors, happier patients, and more focused doctors. They set the foundation for a digital-first healthcare environment where efficiency and empathy coexist, and where technology amplifies rather than replaces human care.
Compliance and Security Considerations
Implementing an AI patient intake agent in a clinic is not just a technical exercise—it is also a compliance and security challenge. Healthcare data is among the most sensitive categories of personal information, and mishandling it can result in regulatory penalties, reputational damage, and loss of patient trust. For an AI intake agent to succeed, it must be designed with privacy-first architecture, aligning with international and regional health regulations while safeguarding every data transaction.
-
HIPAA, GDPR, and Regional Health Data Laws
Two of the most widely recognized frameworks for health data protection are the Health Insurance Portability and Accountability Act (HIPAA) in the United States and the General Data Protection Regulation (GDPR) in the European Union. While they differ in scope, both emphasize patient privacy, secure data handling, and informed consent.
- HIPAA requires healthcare providers and their technology partners to ensure the confidentiality, integrity, and availability of Protected Health Information (PHI). This includes safeguards around data collection, storage, and transfer, as well as strict auditing and breach reporting requirements.
- GDPR applies to any organization processing personal data of EU citizens, regardless of where the provider is located. It emphasizes data minimization, lawful processing, and the patient’s right to access, correct, or delete their data.
Other regions have similar regulations: for example, the UK’s Data Protection Act, Canada’s PIPEDA, and India’s emerging Digital Personal Data Protection Act (DPDPA). Clinics must ensure that their AI intake agents are compliant with the laws relevant to their operating geography.
For global vendors, this means building systems that support configurable compliance—allowing clinics in different regions to enforce the specific rules applicable to their patient base.
-
Data Encryption and Secure Transmission
Encryption is the backbone of healthcare data protection. An AI intake agent must implement end-to-end encryption for both data in transit and data at rest.
- In transit: When patients submit data through WhatsApp, SMS, or a web portal, it must be encrypted using protocols such as TLS (Transport Layer Security). This prevents interception during transmission.
- At rest: Once stored in servers or integrated into an EHR, the data must remain encrypted, typically using AES-256 or similar advanced encryption standards.
Secure transmission extends beyond encryption to include authentication protocols. Multi-factor authentication ensures that only authorized users access sensitive systems. Additionally, audit trails must record every data access, modification, or transfer, providing accountability in case of security reviews or incidents.
Another key consideration is vendor infrastructure. Clinics must evaluate whether the AI intake platform is hosted on compliant cloud environments (e.g., AWS HIPAA-eligible services, Microsoft Azure Healthcare APIs) and whether data centers meet international security certifications such as ISO 27001 or SOC 2.
-
Role-Based Access Controls
Not every staff member should have access to all patient data. Role-based access control (RBAC) ensures that employees only see the information necessary for their duties. For example:
- Front-desk staff may access demographic and scheduling data but not detailed medical histories.
- Nurses may view symptoms and vital signs but not financial data.
- Billing teams may require insurance details but not clinical notes.
AI intake systems must support RBAC by integrating with a clinic’s identity and access management tools. Permissions should be granular and regularly reviewed to avoid privilege creep, where employees accumulate unnecessary access over time.
Additionally, automatic session timeouts, login monitoring, and real-time alerts for unusual access patterns can further strengthen security. These measures not only align with regulatory expectations but also reduce insider threats, which remain one of the leading causes of healthcare data breaches.
-
Consent Management
One of the most important elements of compliance is ensuring informed patient consent. AI intake agents must provide patients with clear, understandable explanations of how their data will be used, stored, and shared.
Best practices for consent management include:
- Transparent disclosures: Present patients with concise, plain-language statements about data collection. Avoid technical jargon that obscures meaning.
- Granular options: Allow patients to consent to some uses of their data (e.g., sharing with insurance providers) while declining others (e.g., third-party research).
- Revocation rights: Patients must have the ability to withdraw consent at any time, with processes in place to delete or anonymize their data upon request.
- Audit trails: Every consent action should be logged and time-stamped for legal accountability.
In regions governed by GDPR, consent is especially strict—silence or pre-ticked boxes are not valid. Clinics must design AI agents that actively prompt patients for opt-ins, ensuring compliance from the start.
Effective consent management not only satisfies regulations but also builds patient trust. When patients know they are in control of their information, they are more likely to engage with digital intake systems confidently.
Compliance and security considerations are not optional add-ons—they are fundamental requirements for implementing AI intake agents in healthcare. Adhering to HIPAA, GDPR, and regional laws, encrypting data across its lifecycle, enforcing role-based access, and managing patient consent transparently are all essential safeguards.
Clinics that overlook these issues risk regulatory fines, reputational damage, and—most importantly—loss of patient trust. Conversely, those that implement AI intake agents with a strong compliance-first strategy can position themselves as trustworthy, modern, and patient-centric. In an era where data privacy is as important as medical quality, secure and compliant AI intake is the foundation for sustainable digital transformation in healthcare.
Measuring Success and ROI
Adopting an AI patient intake agent is a strategic investment, and like any investment, clinics must measure whether it delivers the promised value. Success cannot be determined by implementation alone—it must be tracked using concrete metrics, financial outcomes, and patient experience improvements. By establishing clear key performance indicators (KPIs) and comparing them against pre-implementation baselines, clinics can evaluate both immediate impact and long-term return on investment (ROI).
Key Performance Indicators
Wait Time Reduction
One of the most visible improvements from an AI intake agent is a reduction in patient waiting times. Traditional intake can consume 15–30 minutes per patient, especially when forms are completed onsite and insurance verification is manual. With AI, much of this work happens before the patient arrives, or in parallel with staff operations.
To measure success, clinics should track:
- Average patient wait time before consultation.
- Percentage of patients completing intake digitally before arrival.
- Reduction in front-desk congestion during peak hours.
For example, if wait times fall from 25 minutes to 10 minutes on average, this not only boosts satisfaction but also increases the clinic’s throughput, allowing more patients to be seen daily.
Error Reduction
Manual data entry is a common source of errors, from misspelled names to missing insurance details. These errors lead to claim denials, billing disputes, and clinical risks. AI intake agents minimize these problems by autofilling known data, validating entries in real time, and prompting patients to correct missing fields.
Error reduction can be tracked through:
- Percentage of intake records requiring staff correction.
- Number of claim denials due to incorrect intake data.
- Reduction in duplicate or incomplete patient files.
Even a modest 30–40 percent reduction in intake errors can translate into significant time and cost savings over a year.
Patient Satisfaction
Ultimately, healthcare success is measured by patient experience. AI intake systems improve convenience by allowing patients to complete forms on their phones, in their preferred language, and without repeating details at every visit.
Patient satisfaction can be tracked via:
- Post-visit surveys focusing on intake ease.
- Net Promoter Score (NPS) improvements.
- Volume of positive vs. negative feedback about front-office operations.
High satisfaction scores translate into stronger patient loyalty, better compliance with follow-ups, and more referrals—all of which have downstream financial benefits.
Cost Savings vs. Traditional Intake Methods
AI intake agents deliver measurable financial benefits by reducing reliance on manual processes. The savings often come from areas that are otherwise considered sunk costs:
- Labor Efficiency
Front-desk staff spend less time on repetitive tasks like transcription, insurance validation, and form distribution. A clinic that needed three staff for registration may operate with two, redeploying the third to higher-value roles such as patient navigation or coordination.
- Reduced Paper and Storage Costs
Paper-based systems require printing, storage space, and archiving—costs that accumulate over time. Digital intake eliminates these expenses almost entirely.
- Fewer Claim Denials
Insurance claim denials are costly, requiring reprocessing and often leading to delayed or lost revenue. By improving accuracy and eligibility checks, AI systems reduce denial rates and accelerate reimbursement.
- Increased Throughput
Shorter wait times mean clinics can accommodate more patients without additional staff or infrastructure. A clinic that increases its daily patient volume by 10–15 percent without expanding resources realizes immediate financial benefits.
When quantified, these savings often outweigh the subscription or development costs of an AI intake platform.
Timeline for ROI Realization
Healthcare technology investments often face scrutiny for their payback periods. With AI intake agents, ROI can typically be realized within 6 to 18 months, depending on the clinic’s size and patient volume.
- Short-term gains (0–6 months): Reduced paper usage, lower error correction workload, and visible improvements in patient satisfaction.
- Medium-term gains (6–12 months): Significant reduction in claim denials, lower labor costs, and smoother peak-hour operations.
- Long-term gains (12–18 months): Increased patient retention, stronger referral patterns, and improved brand reputation as a tech-forward, patient-centric provider.
For larger hospital systems, the ROI window may be closer to 18–24 months due to higher implementation complexity. However, once established, the scalability of AI intake ensures that benefits compound over time.
Measuring success with an AI patient intake agent requires a balanced approach that considers operational efficiency, financial performance, and patient experience. By focusing on KPIs like wait time reduction, error minimization, and satisfaction scores, clinics can track tangible improvements. When combined with cost savings from labor efficiency, reduced claim denials, and increased throughput, these outcomes create a strong case for ROI within the first 12–18 months.
For clinics evaluating whether the investment is worthwhile, the evidence is clear: AI intake agents are not just a cost-saving tool but a long-term enabler of sustainable, patient-centered healthcare.
Real-World Use Cases and Case Studies
While the theoretical benefits of AI-powered patient intake agents are compelling, their true value is best illustrated through real-world applications. Clinics and hospitals of different sizes, as well as virtual healthcare providers, have adopted AI intake systems to address specific operational challenges. The following case-based scenarios highlight how these solutions deliver tangible results across different healthcare contexts.
Small Clinic Adoption: Reducing Administrative Overhead
The Challenge
A small, independent family practice with two physicians and limited front-desk staff was struggling with administrative overload. Staff members spent up to 40 percent of their time on repetitive tasks such as transcribing handwritten forms, calling insurance providers, and correcting patient records. During busy mornings, patients often waited over 20 minutes to complete intake, and dissatisfied patients frequently voiced frustration about delays.
The AI Solution
The clinic implemented a lightweight AI intake agent integrated with its EHR. The system allowed patients to pre-register via WhatsApp or a web link before their visit. Returning patients’ information was automatically retrieved and verified, requiring updates only when necessary. Insurance details were validated through real-time connections with payer systems, eliminating many claim rejections.
The Outcome
Within three months, the clinic reported:
- 70% of patients completing intake before arrival, significantly reducing congestion at the front desk.
- Average intake time per patient dropped from 20 minutes to under 8 minutes.
- Claim denials related to incorrect intake data decreased by 30%, improving revenue cycle efficiency.
- Staff satisfaction improved, with employees reporting more time available to focus on patient support rather than paperwork.
This example demonstrates how even small clinics—often constrained by resources—can use AI intake systems to operate more efficiently, improve patient experience, and compete with larger providers in terms of service quality.
Multi-Specialty Hospital: Scaling Intake Across Departments
The Challenge
A large multi-specialty hospital with more than 500 daily outpatient visits faced a different problem: scalability. Each department—cardiology, orthopedics, pediatrics, dermatology—had its own intake forms and processes, creating inconsistencies in data collection. Patients often repeated the same details multiple times if they visited different departments. Administrative staff were stretched thin, and average patient wait times exceeded 30 minutes.
The AI Solution
The hospital adopted a custom AI intake platform that was integrated with its centralized EHR and configured for department-specific workflows. The system used conditional logic to tailor questions based on patient needs. For example:
- Cardiology patients were prompted for blood pressure history and cholesterol medications.
- Orthopedic patients were asked about past injuries, physical therapy, and mobility challenges.
- Pediatric visits required vaccination history and parental consent forms.
The AI system supported multiple intake channels—web portals for tech-savvy patients, in-clinic kiosks for walk-ins, and SMS/WhatsApp options for those who preferred mobile communication.
The Outcome
After six months of rollout across all departments, the hospital achieved:
- A 45% reduction in patient wait times, bringing the average from 32 minutes to 17 minutes.
- Improved data quality, with error rates dropping by 60% compared to manual entry.
- Increased patient throughput, enabling the hospital to accommodate 12% more appointments without adding staff.
- Enhanced compliance, as consent forms were digitally stored and automatically linked to patient records.
By standardizing intake across departments while allowing specialty-level customization, the hospital created a unified but flexible system. This not only improved operational efficiency but also enhanced patient trust, as patients no longer had to repeatedly provide the same information.
Telehealth Practices: Virtual Patient Onboarding
The Challenge
A rapidly growing telehealth provider offering general consultations and mental health services struggled with virtual onboarding. Patients often booked appointments online but skipped filling out intake forms, leaving doctors unprepared for consultations. Administrative staff had to chase patients via email or phone, creating delays and reducing the effectiveness of telehealth visits. Incomplete histories also led to clinical inefficiencies, as doctors spent the first portion of consultations gathering basic details.
The AI Solution
The provider introduced a virtual AI intake agent integrated directly into its booking platform. After scheduling an appointment, patients automatically received intake prompts via their chosen channel (email, SMS, or in-app chat). The AI guided them through symptom descriptions, medication histories, and insurance details. For mental health consultations, the system included sensitive but essential questions on prior diagnoses and ongoing treatments, using conversational language to make patients feel comfortable.
Because telehealth patients often needed flexibility, the AI system allowed asynchronous intake. Patients could pause and resume the intake process, with data automatically saved and synced to the doctor’s dashboard before the consultation.
The Outcome
Within four months of deployment, the telehealth provider saw:
- 92% completion rate for digital intake before the start of consultations.
- Consultations began with structured data already in the doctor’s EHR view, reducing wasted time.
- Patient satisfaction scores increased, with surveys citing “smooth onboarding” as a key improvement.
- Doctors reported being able to spend 15–20% more of each consultation on diagnosis and treatment, rather than intake.
This case underscores the unique value of AI intake systems for virtual healthcare providers. By ensuring doctors are fully prepared before a telehealth call, AI improves both efficiency and quality of care.
These real-world scenarios highlight how AI patient intake agents can be adapted to very different contexts: a small clinic reducing administrative burden, a large hospital standardizing processes across departments, and a telehealth provider streamlining virtual onboarding. In each case, the common outcomes were shorter wait times, fewer errors, higher patient satisfaction, and improved financial performance.
The lesson is clear: whether serving dozens of patients or thousands, whether onsite or online, AI intake agents are a scalable solution. They transform intake from a bottleneck into a streamlined, patient-friendly process that benefits every stakeholder in the healthcare ecosystem.
Future of AI in Patient Intake
AI-driven patient intake is already reshaping healthcare, but the technology is far from reaching its full potential. As innovations in artificial intelligence, natural language processing, and connected health ecosystems advance, the scope of intake agents will expand beyond basic automation. The future of AI in patient intake lies in systems that are predictive, proactive, and seamlessly integrated into the broader healthcare journey. Four emerging trends highlight where this evolution is headed.
-
Predictive Analytics for Patient Care
Future intake agents will not simply collect data—they will interpret it in real time to generate actionable insights. By leveraging predictive analytics, AI can detect potential health risks based on patient responses, historical data, and population health trends.
For example, if a patient reports chest discomfort and has a history of high cholesterol and smoking, the intake agent could flag the case as potentially urgent and recommend immediate diagnostic tests. Similarly, in primary care settings, AI could identify patterns indicating risk of diabetes, hypertension, or depression and alert clinicians before the consultation begins.
Predictive intake reduces the risk of missed red flags, supports early intervention, and enhances preventive care. Over time, as agents accumulate longitudinal patient data, their ability to provide personalized health predictions will grow, turning intake into an essential part of risk management.
-
AI-Powered Triage Agents
Today, intake agents streamline paperwork; tomorrow, they will evolve into triage assistants. By analyzing symptom descriptions and patient histories, AI agents will classify cases by urgency and direct patients to the most appropriate care pathway.
For example:
- A patient with flu-like symptoms may be directed toward a telehealth consultation.
- A patient describing chest pain and shortness of breath may be flagged for immediate emergency evaluation.
- Non-urgent cases such as prescription refills could be routed to automated self-service workflows, saving clinician time.
This triage capability will not replace clinical judgment but will prioritize and route cases efficiently, ensuring patients receive timely care and providers allocate resources where they are needed most. Hospitals and urgent care centers, in particular, stand to benefit from this intelligent front-line screening, reducing overcrowding and optimizing patient flow.
-
Integration with Wearable Devices and IoT in Healthcare
The future of intake will not be limited to patient self-reporting. With the rise of wearable devices and healthcare IoT, intake agents will have access to continuous streams of patient data—heart rate, blood pressure, glucose levels, sleep patterns, and more.
Imagine a patient arriving for a cardiology appointment. Instead of filling out forms about recent symptoms, the intake agent could pull real-time data from their smartwatch or connected blood pressure monitor. This integration allows intake to move beyond static snapshots into dynamic, data-rich profiles of patients’ health.
For chronic disease management, such as diabetes or hypertension, IoT integration ensures that doctors begin consultations with a clear picture of recent trends rather than relying solely on patient recollection. In the long term, this could reduce hospital readmissions, enable proactive interventions, and personalize care plans more effectively.
-
Voice-Based Intake Agents
Another frontier in patient intake is voice interaction. Not all patients are comfortable with typing or digital forms, particularly the elderly or those with limited literacy. Voice-enabled AI intake agents provide an intuitive alternative, allowing patients to complete intake simply by speaking.
Using advanced speech recognition and natural language understanding, these agents can capture detailed histories in conversational form. For example, a patient might say, “I’ve been having stomach pain after meals for about two weeks.” The AI can extract relevant details—symptom type, duration, and frequency—while prompting follow-up questions for clarity.
Voice-based intake will also enhance accessibility for patients with disabilities, ensuring inclusivity. Clinics could deploy voice-enabled kiosks in waiting rooms, while telehealth providers could integrate voice intake directly into pre-consultation calls.
As voice technology improves, it will make intake more human-like and less transactional, further reducing friction in the patient journey.
The future of AI in patient intake is moving toward intelligent, connected, and personalized systems. Predictive analytics will help identify risks before they escalate, triage agents will prioritize patients more effectively, IoT integration will provide clinicians with continuous real-world data, and voice-enabled systems will make intake universally accessible.
For clinics, these advancements mean not only smoother operations but also better clinical outcomes and stronger patient engagement. For patients, it means an intake process that feels less like paperwork and more like the beginning of a meaningful, proactive healthcare experience.
AI intake agents are already solving today’s challenges—but their future role promises to transform the very foundation of patient-provider interaction, bringing healthcare closer to being truly preventive, inclusive, and data-driven.
Why Choose Aalpha for AI Patient Intake Agent Development
Selecting the right technology partner is as important as choosing the right AI platform. Implementing an AI patient intake agent requires deep domain knowledge, technical expertise, and an understanding of healthcare compliance. This is where Aalpha stands apart. With years of experience in building healthcare automation solutions, Aalpha combines innovation with reliability, offering clinics a trusted pathway to digital transformation.
Experience in Healthcare Automation
Aalpha has a proven track record in developing automation solutions tailored for healthcare providers. From electronic health record (EHR) integrations to secure telehealth platforms, our team has worked across multiple domains of healthcare IT. This experience ensures that we not only understand the technology but also the unique operational challenges faced by clinics and hospitals.
For example, we have successfully delivered projects where intake automation reduced patient waiting times by more than half, while also cutting claim denial rates. This hands-on expertise allows us to anticipate common pitfalls, such as data integration issues or compliance hurdles, and proactively design solutions that are both efficient and regulation-ready.
End-to-End Development and Support
Implementing an AI intake agent is not a one-off task; it is a continuous process that involves planning, deployment, monitoring, and iteration. At Aalpha, we provide end-to-end services to ensure success at every stage.
- Consultation and planning: We begin by assessing your clinic’s specific needs, identifying bottlenecks, and recommending the best-fit solution.
- Custom development: Our team builds AI intake systems that align with your workflows, integrating seamlessly with your existing EHR or practice management software.
- Testing and rollout: We support controlled pilot rollouts, gather feedback, and optimize the system before full deployment.
- Ongoing support: Once live, we provide continuous maintenance, compliance updates, and enhancements to keep your system future-ready.
This full-lifecycle approach means that clinics never have to worry about being left behind once the technology is implemented. Our partnership model is designed to ensure that the system grows with your practice.
Custom Solutions for Different Clinic Sizes
Healthcare is not one-size-fits-all, and neither are AI intake agents. Aalpha specializes in building scalable solutions that can adapt to the size and complexity of each clinic.
- Small clinics and practices: We develop lightweight, cost-effective systems that automate key tasks like pre-registration, insurance validation, and consent management—helping small teams reduce administrative burden without overwhelming budgets.
- Large hospitals and multi-specialty centers: For high-volume environments, we design advanced intake systems capable of supporting multiple departments, conditional workflows, multilingual interfaces, and real-time data synchronization across complex EHR infrastructures.
- Telehealth providers: For virtual care, we build intake solutions optimized for remote onboarding, ensuring patients complete forms and share medical histories before video consultations begin.
By tailoring solutions to the scale and scope of each client, Aalpha ensures that every healthcare provider—regardless of size—can unlock the benefits of AI intake automation.
Implementing an AI patient intake agent is not just about adopting new technology; it is about redefining how patients and providers interact. With Aalpha, clinics gain a partner who understands both the technical and regulatory landscape of healthcare. Our experience in automation, commitment to end-to-end support, and ability to deliver custom solutions for different clinic sizes make us the ideal choice for providers ready to modernize their intake process.
By choosing Aalpha, you ensure that your clinic is not just keeping pace with digital transformation but leading it—offering patients a seamless, efficient, and trustworthy intake experience.
Conclusion
AI-powered patient intake agents are no longer a futuristic concept—they are a practical, proven solution to one of the most persistent bottlenecks in healthcare. By reducing wait times, minimizing errors, streamlining compliance, and improving patient satisfaction, these systems redefine the front-office experience. For doctors, they provide accurate, structured data at the point of care; for staff, they eliminate repetitive work; and for patients, they make the journey from registration to consultation faster, smoother, and less stressful.
The steps outlined in this guide demonstrate that successful implementation requires more than just technology—it demands careful planning, integration, and support. Clinics that take this leap are not only improving efficiency today but also positioning themselves for the future of patient-centered, data-driven healthcare.
If your clinic is ready to transform patient intake with AI, the top rated AI development company – Aalpha is here to help. With deep expertise in healthcare automation, end-to-end development support, and customized solutions for practices of every size, we deliver AI intake agents built for real-world clinical impact.
Reach out to our team today to discuss your clinic’s needs and explore how an AI-powered intake system can reduce costs, improve patient experience, and strengthen your operations.
FAQs
How long does it take to implement an AI intake agent?
Implementation time depends on the clinic’s size and complexity. Small practices can go live in 4–8 weeks, while mid-sized clinics may need 2–3 months for customization and EHR integration. Large hospitals with multiple departments typically require 4–6 months due to more complex workflows and phased rollouts. A short pilot phase is often recommended before full deployment to refine processes and ensure smooth adoption.
Can it integrate with my existing EHR/EMR?
Yes. Most AI intake agents connect with major systems such as Epic, Cerner, and Athenahealth via secure APIs. This allows patient data—demographics, medical history, insurance, consent forms—to flow directly into the right fields in your EHR. For older or custom-built systems, integration bridges can be developed to maintain compatibility while meeting compliance standards.
Is it suitable for small clinics or only large hospitals?
AI intake is valuable for both. Small clinics use it to reduce front-desk workload, cut waiting times, and free limited staff for patient-facing tasks. Large hospitals use it to handle intake at scale, standardize processes across departments, and manage hundreds of daily patients without expanding staff. The systems are designed to scale up or down depending on practice size.
How secure is patient data with AI intake agents?
Patient data security is a top priority. Leading systems comply with HIPAA, GDPR, and local health data laws, ensuring all information is encrypted both in transit and at rest. Role-based access controls limit who can view sensitive information, and detailed audit logs track every action. Patients also provide explicit consent, and clinics can configure systems to honor regional privacy regulations.
What is the cost of implementation and maintenance?
Costs vary by scope:
- Small practices can expect lower upfront or subscription fees for off-the-shelf solutions.
- Mid to large providers investing in custom integrations will see higher initial costs but greater efficiency gains.
Maintenance typically includes software updates, compliance upgrades, and ongoing support. Most clinics achieve a return on investment in 6–18 months through reduced labor costs, fewer claim denials, and increased patient throughput.
Do patients prefer interacting with AI over staff?
Surveys show that many patients appreciate the speed and convenience of AI intake, especially when it’s offered via familiar channels like WhatsApp or web forms. Younger and tech-comfortable patients often prefer digital intake, while some older patients may still lean on staff for help. The most effective approach is hybrid: AI handles routine tasks, while staff assist patients who need extra support. This balance improves satisfaction for all demographics.
AI intake agents are flexible, secure, and scalable—designed to support clinics of every size. By integrating smoothly with existing systems, reducing administrative overhead, and improving patient experiences, they offer one of the clearest paths to measurable ROI in healthcare technology today.
Want to implement AI patient intake the smart way? Connect with Aalpha now.